Title:
Category:
Description:
Keratopathy secondary to lagophthalmos is a form of exposure keratoconjunctivitis. It is associated with the following clinical findings:
- A horizontal band of corneal damage that corresponds to the region of the exposed interpalpebral fissure
- Incomplete eyelid closure during blinking
- Incomplete eyelid closure during sleep
- Possible secondary ocular infection
Lagophthalmos may result from trauma, unexpected consequence of facial or eyelid surgery, seventh nerve palsy, Bell’s palsy and floppy eyelid syndrome. None of these conditions were noted.
Case Report
- An 71-year-old woman presented to the office with a chief complaint of chronic foreign body sensations
- Case history describes acute ocular discomfort that begins upon awakening and persists throughout the day
Conclusion
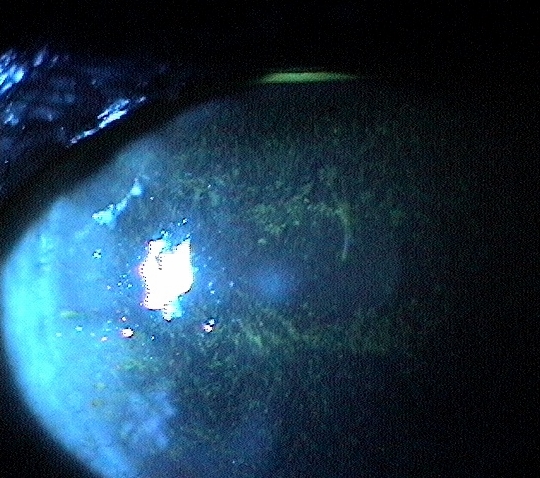
As with most eye diseases, the correct diagnosis is the key to proper treatment. The size, shape and location of the corneal staining pattern reveals the cause of the exposure keratopathy is nocturnal lagophthalmos.
History of Present Illness
- Associated Signs and Symptoms: fluctuating vision
- Location: both eyes
- Duration: variable over several months
- Quality: gritty, foreign body sensations
- Context: mildly sensitive to bright light
- Severity: moderate
- Timing: discomfort is getting worse over time
- Modifiers: none
Review of Systems
- The patient reported that she was in good health and taking no medications
Past, Family and Social History
- Non-contributory
Best Corrected Distance Visual Acuity
- 20/30 in the right eye
- 20/30 in the left eye
Normal Examination Findings
- Mental status
- General medical observation
- Pupils
- Ophthalmoscopy
Not Performed on Today’s Examination
- Gross visual fields
- Basic sensorimotor examination
Intraocular Pressure Measurements
- 13 mm Hg in the right eye
- 13 mm Hg in the left eye
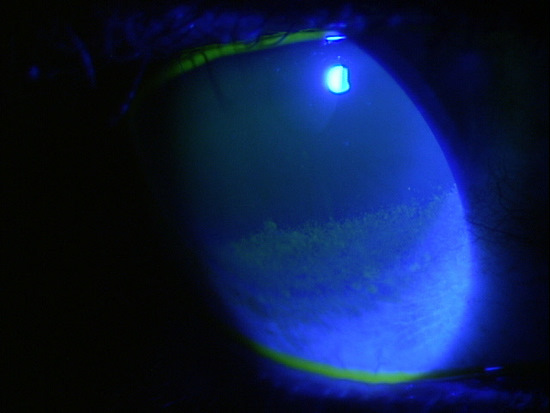
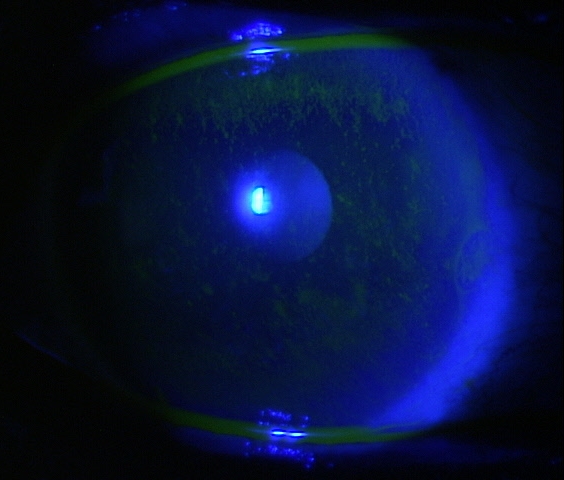
External Ocular Examination with Biomicroscopy
- Exposure keratopathy on the lower one-third of the cornea
- Incomplete blink even upon forced effort
 |
Clinical Appearance of the Cornea
|
Clinical Diagnosis
The clinical diagnosis is a determination based on the knowledge obtained from the patient’s medical history and from the results of the eye examination alone, without the benefit of diagnostic tests or procedures.
The patient’s clinical diagnosis is exposure keratopathy secondary to lagophthalmos based on the following clinical findings:
- Observation of incomplete lid closure
- Clinical appearance of the involved cornea
- Nature of the presenting problem
Treatment Plan
To gather the clinical information required to treat exposure keratopathy, a diagnostic and treatment program is initiated.
- Determination of different types of diagnoses
- Selection of one or more treatment options
After a clinical diagnosis has been determined, the diagnostic process continues with a process that involves the identification and exclusion of differential diagnoses.
The differential diagnostic process allows the doctor to distinguish between two or more diseases with similar signs and symptoms by systematically comparing their signs and symptoms. Potential conditions with similar presentations to exposure keratopathy could include the following:
The patient could also be experiencing a lagophthalmos secondary to:
- Bell’s palsy – (other facial muscle involvement)
- Isolated seventh nerve palsy – (history of injury, surgery)
- Orbital proptosis secondary to thyroid disease – (history of thyroid disease, proptosis)
- Floppy eyelid syndrome – (physical appearance of thickened lid, obese patient, males)
Ordering Diagnostic Tests
When additional clinical information is needed to complete the differential diagnostic process or to assist in the treatment program, diagnostic tests or services are ordered. The performance of these tests and/or services leads to the completion of the differential diagnostic process while simultaneously initiating the treatment program.
Based on a clinical diagnosis of exposure keratopathy secondary to lagophthalmos, the following diagnostic tests were ordered at the conclusion of the eye examination.
- External ocular photography
External Ocular Photography
Any case of compromised tissue that could pose a threat to function could justify the medical necessity of photodocumentation. In this case, the compromised cornea tissue posed risks of infection, scarring and neovascularization. Photodocumentation of the tissue provides a baseline to monitor disease regression and efficacy of treatment.
Physical Diagnosis
Completion of the differential diagnosis process either returns you to the original clinical diagnosis or it produces a more substantiated physical diagnosis. This component of the diagnostic and treatment program, the determination of a physical diagnosis, is accomplished by studying the physical manifestations of health and illness revealed in the eye examination, the patient’s complete medical history, and supported by various diagnostic tests and procedures.
The diagnostic tests results help substantiate the physical diagnosis of exposure keratopathy secondary to lagophthalmos and provide a framework for monitoring changes in the disease and response to therapeutic intervention.
This patient presents with a history of chronic eye irritation.
According to Current Procedural Terminology, when eye doctors perform ophthalmological examinations, the complexity of medical decision-making is not separated from the examining techniques used. However, as a tool to assist eye doctors in enhancing their medical decision-making skills, consider that the complexity of medical decision-making in this case report involves three components.
Diagnosis Guidelines
The first component concerns the number of possible diagnoses and treatment options that must be considered. The diagnosis and treatment of a exposure keratopathy is predicated on making the proper diagnosis and on understanding the natural history of the effects of chronic dessication on the corneal tissue.
The second component concerns the amount and complexity of medical records and diagnostic tests that have to be obtained, reviewed and analyzed. In addition to an eye examination, this visit required the review and analysis of external photodocumentation.
Third, the complexity of medical decision-making is affected by the risk of significant complications and/or morbidity associated with exposure keratopathy and the risks involved in any treatment options. Exposure keratopathy treatment can be considered at several levels but failure to eliminate the problem can result in chronic ocular irritation, secondary infection, neovascularization and/or loss of vision.
Treatment Options
To begin the treatment of a exposure keratopathy, the eye doctor must firmly establish the underlying etiology. In most cases, primary treatment of the resultant corneal condition is either supportive (moisturize) or prophylactic (antibiosis). But in most cases, unless the underlying causative factor is addressed, the condition tends to become chronic and more severe. Increased wetting of the cornea can be accomplished by prescribing artificial tears, lubricating ointments, or punctal occlusion.
Protection of the irritated cornea can be accomplished with a standard bandage contact lens or application of an amnionic membrane insert. Depending of the severity of corneal compromise, prophylactic antibiosis can be considered. Keratotoxic preparations should be avoided, especially aminoglycosides. Erythromycin or polysporin drops or ointment are excellent choices. To assist corneal healing, especially if waiting on a more permanent solution to the underlying eyelid pathology, taping the eyelids shut at night can be considered. Taping is rarely a definitive therapy and should be considered only for short-term treatment.
Exposure keratopathy secondary to incomplete eyelid closure is a common condition. If the condition cannot be controlled with more supportive measures, referral to an oculoplastic surgeon for eyelid reconstruction, tarsorrhaphy, or implantation of weights in the upper lid should be considered.
In this case, Systane Ultra (Alcon Laboratories, Inc.) artificial tears was prescribed along with bandage contact lenses. Polytrim drops were prescribed b.i.d. for prophylactic antibiosis. After two weeks, the condition improved significantly.
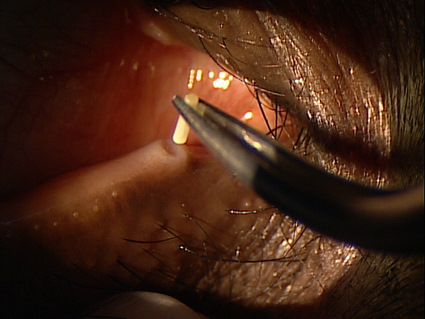
Because symptoms of ocular irritation were still present after two weeks, punctal occlusion was added to the treatment regimen.
Based on patient history, the nature of the presenting problem, and my own clinical judgement this patient did not need an evaluation of the complete visual system.
- Perform the eye examination that is medically necessary
- Provide the diagnostic test or service that is medically necessary
- Document the service provided
- Code from the documentation
- Report the service to the payor
Physician Quality Reporting System
PQRS Measure 130: Current Medications with Name, Dosage, Frequency and Route Documented – CPT code G8427
This measure applies to patients 18 years and older. The measure should be reported on the day of the examination and can be used with any diagnosis code.
PQRS Measure 226: Patient screened for tobacco use and identified as a non-user of tobacco – CPT code 1036F
This measure applies to patients 18 years and older. The measure should be reported on the day of the examination and can be used with any diagnosis code.
Modifier 50
This modifier describes a bilateral procedure. It is used when the procedure is performed on paired body parts (e.g., both eyes) at the same operative session. Do not use the modifier when the CPT code description contains “bilateral” or “unilateral or bilateral”. Procedures reported with the -50 modifier will have a unit of 1 on the service line.
Modifier 25
This modifier describes a significant, separately identifiable eye examination by the same doctor on the day of a surgical procedure. A different diagnosis is not needed and documentation should support the utilization of the -25 modifier. To assist in determining the medical necessity of appending the -25 modifier to an examination, ask yourself the following questions:
- What was the purpose of the patient’s visit?
- Is there anything that would prompt a separate eye examination?
- Does the documentation support an eye exam over and above the usual work for the minor surgical procedure?
Eyelid Site Modifiers
CPT code 68761 is used to report punctal occlusion. The code describes a service that is performed per punctum and therefore must be reported with an eyelid site modifier on the service line. The following site modifiers should be appended to CPT code 68761 as indicated:
E1 — Upper left punctum
E2 — Lower left punctum
E3 — Upper right punctum
E4 — Lower right punctum
INITIAL EXAMINATION – DAY 1
| Diagnosis Code | Procedure Code | Modifier | Quantity | Payor | Amount Allowed |
| H16.213 - Exposure keratoconjunctivitis, bilateral | 92002 - Medical eye examination | 1 | Medicare | 83.69 | |
| H16.213 - Exposure keratoconjunctivitis, bilateral | 92285 - External ocular photography | 1 | Medicare | 20.90 | |
| H16.213 - Exposure keratoconjunctivitis, bilateral | 92071 - Bandage contact lens | 2 | Medicare | 77.98 | |
| H16.213 - Exposure keratoconjunctivitis, bilateral | G8427 - Medications documented | Medicare | 44.31 | ||
| H16.213 - Exposure keratoconjunctivitis, bilateral | 1036F - Patient screened for tobacco use | Medicare | 0.00 |
SUBSEQUENT ENCOUNTER – DAY 7
| Diagnosis Code | Procedure Code | Modifier | Quantity | Payor | Amount Allowed |
| H16.213 - Exposure keratoconjunctivitis, bilateral | 92012 - Medical eye examination | 1 | Medicare | 87.69 | |
| H16.213 - Exposure keratoconjunctivitis, bilateral | G8427 - Medications documented | Medicare | 0.00 | ||
| H16.213 - Exposure keratoconjunctivitis, bilateral | 1036F - Screened for tobacco use | Medicare | 0.00 |
SUBSEQUENT ENCOUNTER – DAY 14
| Diagnosis Code | Procedure Code | Modifier | Quantity | Payor | Amount Allowed |
| H16.213 - Exposure keratoconjunctivitis, bilateral | 92012 - Medical eye examination | 25 | 1 | Medicare | 87.69 |
| H16.213 - Exposure keratoconjunctivitis, bilateral | 68761 - Punctal occlusion | 50, E2, E4 | 1 | Medicare | 230.13 |
| H16.213 - Exposure keratoconjunctivitis, bilateral | G8427 - Medications documented | Medicare | 0.00 | ||
| H16.213 - Exposure keratoconjunctivitis, bilateral | 1036F - Screened for tobacco use | Medicare | 0.00 |
SUBSEQUENT ENCOUNTER – DAY 28
| Diagnosis Code | Procedure Code | Modifier | Quantity | Payor | Amount Allowed |
| H16.213 - Exposure keratoconjunctivitis, bilateral | 68761 - Punctal occulsion | 50, E2, E4 | 1 | Medicare | 230.13 |
| H16.213 - Exposure keratoconjunctivitis, bilateral | G8427 - Medications documented | Medicare | 0.00 | ||
| H16.213 - Exposure keratoconjunctivitis, bilateral | 1036F - Screened for tobacco use | Medicare | 0.00 | ||
| TOTAL FEES FOR ALL VISITS | $818.21 |
H16.213
Exposure keratoconjuncivitis,
bilateral
H02.231
Paralytic lagophthalmos,
right upper eyelid
H02.234
Paralytic lagophthalmos,
left upper eyelid
370.34
Exposure keratoconjunctivitis
92285
External ocular photography
92071
Bandage contact lens
68761
Punctal occlusion




 Print | Share
Print | Share