Case Report ID: 5
Title:
Iatrogenic Endotheliopathy After Cataract Surgery
Category:
Cataract surgery is a common out-patient surgical procedure. Complications at some level are common, although most are simply the result of inflammation from tissue manipulation and are minimal problems. Postoperative corneal edema is one of the more common complications of cataract surgery. Most edema is mild, transient and has little to no impact on vision.
One of the most important aspects of postoperative corneal edema is obtainined a thorough knowledge of the patient’s corneal health during the preoperative evaluation. Detailed slit lamp examination and evaluation with specular microscopy should arm the doctor performing the preoperative evaluation with sufficient information to properly counsel the patient regarding the potential for chronic postoperative edema.
Case Report
- A 72-year-old black woman presents to the office one month following a reported uneventful cataract surgery on the right eye
- The patient reported no pain but stated “vision was very foggy”
Conclusion
This case presents the management of an unexpected, excessive postoperative corneal edema following uneventful cataract surgery. In most cases, the edema is self-limiting but therapeutic intervention can significantly hasten resolution of the edema.
History of Present Illness
- Associated Signs and Symptoms: none
- Location: vision is worse in the right eye
- Duration: since cataract surgery one month prior
- Quality: n/a
- Context: vision was poor immediately after surgery and has not improved
- Severity: moderate to severe decrease in vision
- Timing: vision decrease is stable
- Modifiers: none
Review of Systems
The patients medical history was unremarkable. She was using all her postoperative medications in her right eye as prescribed:
- Omnipred t.i.d.
- Nevanac t.i.d.
- Moxeza t.i.d.
Past, Family and Social History
Non-contributory.
Uncorrected Distance Visual Acuity
- 20/40 in the right eye
- 20/25 in the left eye
Normal Examination Findings
- Mental status
- General medical observation
- Pupils
- Adnexal examination
- Ophthalmoscopy
Not Performed on Today’s Examination
- Basic sensorimotor examination
- Gross visual fields
- External examination
Intraocular Pressure Measurements
- 16 mm Hg in the right eye
- 14 mm Hg in the left eye
External Ocular Examination with Biomicroscopy
- Mild loss of stromal transparency in the right eye
- Stable temporal corneal incision
- Centered posterior chamber lens
Clinical Diagnosis
The clinical diagnosis is a determination based on the knowledge obtained from the patient’s medical history and from the results of the eye examination alone, without the benefit of diagnostic tests or procedures.
The patient’s clinical diagnosis is postoperative corneal edema secondary to cataract surgery based on the following clinical findings:
- Recent history of cataract surgery right eye
- Unexpected decreased visual acuity in right eye
- Presence of mild stromal corneal edema
Treatment Plan
To gather the information required to properly counsel a patient regarding postoperative corneal edema, a diagnostic and treatment program is initiated.
- Determination of different types of diagnoses
- Selection of one or more treatment options
The diagnosis of postoperative corneal edema following cataract surgery with reduction in functional vision is relatively straightforward. There are multiple potential etiologies for chronic postoperative corneal edema. These include:
1. Primary,excessive inflammatory response to the surgery
2. Elevated postoperative intraocular pressure
3. Pre-existing corneal endothelial disease
- Fuchs’ endothelial dystrtophy
- Corneal guttata
- Abnormal rate of polymegethism
- Presence of pleomorphism
- Abnormal reduction in endothelial cell density
4. Iatrogenic corneal endotheliopathy
- Direct surgical trauma
- Endothelium touched by instruments
- Endothelium touched by IOL
- Physical damage from irrigating solutions
- Physical damage from ultrasound vibrations
5. Toxic syndromes
6. Intraocular lens syndrome
7. Inflammation from retained lens fragments
8. Detachment of Descemet’s membrane
9. Chemical injury from improperly prepared or expired solutions or from compounds retained on instrumentation
Risk factors for iatrogenic corneal endotheliopathy include preexisting endothelial disease, diabetes, glaucoma, shallow anterior chamber, and previous intraocular surgery. Every effort should be made to determine an exact etiology as treatment options will vary depending upon the cause. If a doctor other than the surgeon is performing the postoperative evaluation, the surgeon should communicate any peri-operative complications that could result in chronic postoperative corneal edema.
Ordering Diagnostic Tests
The following diagnostic tests can help determine the degree of functional vision limitation that is related to postoperative corneal edema and provide information necessary to properly develop a treatment plan and counsel the patient.
- Refraction
- Specular endothelial microscopy
- Corneal topography
- Corneal pachymetry
The decision to order and perform additional testing is totally based on the concept of medical necessity which can only be determined by the examining optometrist or ophthalmologist.
Refraction
- Measuring visual acuity is a method of evaluating functional vision loss
- Corneal edema can produce a loss of visual acuity as well as loss of quality of vision
- No improvement in vision could be obtained after subjective refraction
In many cases, the clinical appearance of the cornea is enough evidence to explain the decreased vision. In these cases, a subjective refraction is unnecessary. Pinhole testing or an automated refractor reading can help make this decision.
Specular Microscopy
Specular microscopy can both confirm the nature of the edema and quantify the degree of endothelial damage. When compared to the non-operated eye, it can also be helpful in confirming whether the cornea was likely at risk or not (although this is likely to be known from a comprehensive preoperative evaluation).
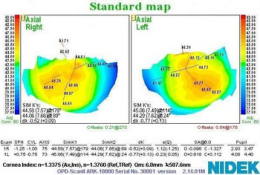
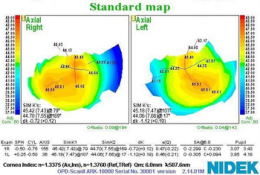
Corneal Topography
Computerized corneal topography is an examination technique that allows you to analyze the physical features and shape of the anterior cornea. It combines the traditional principle of keratoscopy with the data anlysis that is available from modern computers. Important functions of corneal topography include the following:
- Earlier and more accurate diagnosis of corneal disease
- Assist the doctor in determining the appropriate treatment plan
- Preoperative surgical risk assessment
- Postoperative surgical management
All of the diagnostic test results produced a new physical diagnosis of corneal endotheliopathy. Because the patient had no evidence of a compromised corneal endothelium prior to the surgery, the induced endotheliopathy would be classified as iatrogenic.
According to Current Procedural Terminology, when eye doctors perform ophthalmological examinations, the complexity of medical decision-making is not separated from the examining techniques used. As a guideline to assist eye doctors in enhancing their medical decision-making skills, consider that the complexity of medical decision-making involves three components.
The first component concerns the number of possible diagnoses and treatment options that must be considered. The diagnosis of the presence of iatrogenic corneal endotheliopathy is low complexity. Determining the clinical significance of the endotheliopathy can be more complex and involves a thorough understanding and evaluation of the entire eye and vision system. With multiple treatment options, most dependent on identifying the causative factor, the complexity in evaluating a patient with iatrogenic corneal endotheliopathy in mostly in the determination of the proper treatment option.
The second component concerns the amount and complexity of medical records and diagnostic tests that have to be obtained, reviewed and analyzed. In addition to evaluating the elements of the eye in a normal postoperative evaluation, this visit required the review and analysis of a subjective refraction, a specular microscopy evaluation, and a corneal topography evaluation.
Third, the complexity of medical decision-making is affected by the risk of significant complications and/or morbidity associated with iatrogenic corneal endotheliopathy and the risks involved in any treatment options. This patient’s condition was classified as a moderate problem where the risk of significant, irreversible vision loss without treatment was low. However, medical decision-making is complicated by the wide range of treatment options available.
Treatment Guidelines
Iatrogenic corneal endotheliopathy presents with a wide range of treatment options that can range from no treatment to multiple, concurrent treatments. If the endotheliopathy is mild and not causing significant reduction in functional vision, no direct other than monitoring the condition is warranted. Beyond no treatment, the degree of intervention is dependent on the severity of the endotheliopathy and the severity of vision impairment.
Many authorities initiate additional anti-inflammatory medications or increase dosage beyond the normal postoperative dosage of topical steroids. While inflammation is a common component of the postoperative stress on the endothelium leading to exaggerated corneal edema, unless it is a significant component, increasing steroid dosage should have no impact on the condition. Another caution in increasing the steroid dosage is the potential for increased intraocular pressure which will often add to the edema process or at a minimum slow down resolution.
If the intraocular pressure is either elevated or normally over 15-16 mm Hg, reducing the intraocular pressure can reduce the pressure gradient against the endothelium and significantly aid in reducing stromal edema. Medications that target reduction of aqueous production are preferred.
If the edema has spread through the cornea to include the epithelium, topical hyperosmotics may be of some assistance in reducing edema. Hyperosmotics will have a mild effect on stromal edema. If prescribed, hyperosmotic ointments produce less irritation and significantly greater contact time. Copius use of lubricants and application of a bandage contact lens can also help manage the edema when there is epithelial involvement.
In cases of significant endothelial damage, the corneal edema may not resolve and surgical repair of the endothelium is necessary.
Treatment Program
The patient was counseled regarding the nature of her disease and the treatment program explained to her. Topical steroid dosing was increased to q2h until the next progress evaluation. A progress evaluation was scheduled for 72 hours.
Based on the patient history, the nature of the presenting problem, and my own clinical judgement this patient needed an evaluation of the complete visual system.
- Perform the eye examination that is medically necessary
- Provide the diagnostic tests or services that are medically necessary
- Properly document the services provided
- Code from the documentation
- Report the services to the payor
Physicians Quality Reporting System
PQRS Measure 226: Patient screened for tobacco use and identified as a non-user of tobacco – CPT code 1036F
This measure applies to patients 18 years and older. The measure should be reported on the day of the examination and can be used with any diagnosis code.
PQRS Measure 130: Current Medications with Name, Dosage, Frequency and Route Documented – CPT code G8427
This measure applies to patients 18 years and older. The measure should be reported on the day of the examination and can be used with any diagnosis code.
Multiple Procedure Payment Reduction
Effective January 1, 2013, there is a small reduction in payment from Medicare if certain multiple procedures are billed on the same day. The fee for the technical component of the diagnostic test for the second and subsequent tests will be reduced by 20%. The second diagnostic test and subsequent tests should be reported with a -51 modifier. Professional services such as gonioscopy, extended ophthalmoscopy and provocative glaucoma testing are excluded from this policy. Visual evoked potential testing is excluded from this policy.
Modifier 51
This modifier is used to identify the secondary procedure or when multiple procedures are performed on the same day by the same provider. List the major primary procedure first and append the modifier to the subsequent procedure. The primary procedure is the one with the highest dollar value.
INITIAL ENCOUNTER — DAY 1
| Diagnosis Code | Procedure Code | Modifier | Quantity | Payor | Amount Allowed |
| Z96.1 - Presence of intraocular lens | 92012 - Medical eye examination | 1 | Medicare | 87.69 | |
| Z96.1 - Presence of intraocular lens | 92286 - Specular microscopy | 1 | Medicare | 39.06 | |
| H52.213 - Irregular astigmatism, bilateral | 92025 - Corneal topography | 51 | 1 | Medicare | 35.08 |
| Z96.1 - Presence of intraocular lens | 1036F - Patient screened for tobacco use | 1 | Medicare | 0 | |
| Z96.1 - Presence of intraocular lens | G8427 - Current medications documented | 1 | Medicare | 0 | |
| Total | $161.83 |
SUBSEQUENT ENCOUNTER — ONE MONTH
| Diagnosis Code | Procedure Code | Modifier | Quantity | Payor | Amount Allowed |
| Z96.1 - Presence of intraocular lens | 92012 - Medical eye examination | 1 | Medicare | 87.69 | |
| Z96.1 - Presence of intraocular lens | 92286 - Specular microscopy | 1 | Medicare | 39.06 | |
| H52.213 - Irregular astigmatism, bilateral | 92025 - Corneal topography | 51 | 1 | Medicare | 35.08 |
| Z96.1 - Presence of intraocular lens | 1036F - Patient screened for tobacco use | 1 | Medicare | 0 | |
| Z96.1 - Presence of intraocular lens | G8427 - Current medications documented | 1 | Medicare | 0 | |
| Total | $161.83 |
H18.51
Endothelial corneal dystrophy
371.57
Endothelial corneal dystrophy
92286
Specular endothelial microscopy
92285
External ocular photography
76514
Corneal pachymetry
92132
Anterior segment imaging
92025
Corneal topography




 Print | Share
Print | Share