Case Report ID: 20
Title:
Corneal Foreign Body Removal
Category:
Description:
Corneal foreign body occurs when foreign material becomes lodged on or in the corneal epithelium or stroma.
Foreign bodies may be classified by material and the most common types include the following:
- Metal
- Plastic
- Glass
- Organic material
Case Report
- A 43-year-old Hispanic male presented with a chief complaint of eye pain
- Case history described a peice of metal falling into the patient’s eye while working under a car
- The incident happened the previous afternoon
Conclusion
Corneal foreign body removal is a minor surgical procedure that falls within the scope of most primary care eye doctors.
History of Present Illness
- Associated Signs and Symptoms: photophobia, decreased vision, epiphora
- Location: left eye
- Duration: 20 hours
- Quality: throbbing pain
- Context : n/a
- Severity: moderate eye pain
- Timing: pain seems to be getting worse
- Modifiers: none
Reviews of Systems
The patient reported that he was in good health and taking no medications.
Past, Family and Social History
Non-contributory.
Uncorrected Distance Visual Acuity
- 20/20 in the right eye
- 20/50 in the left eye
Normal Examination Findings
- Mental status
- Pupils
- Ophthalmoscopy
Not Performed on Today’s Examination
- Gross visual fields
- Basic sensorimotor examination
General Medical Observation
- A well-nourished male in moderate distress secondary to eye pain
Intraocular Pressure Measurements
- 15 mm Hg in the right eye
- 13 mm Hg in the left eye
Adnexal Examination
- The evaluation if the eyelids was abnormal.
- Moderate edema of the upper left eyelid
- Protective ptosis of the upper left
External Ocular Examination with Biomicroscopy
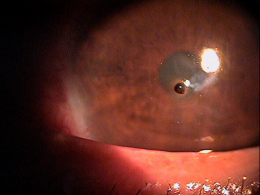
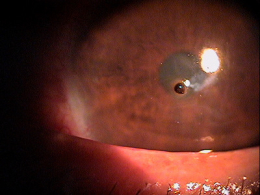
- Metal foreign body embedded in the corneal epithelium
- Secondary ocular inflammation
Clinical Diagnosis
The clinical diagnosis is a determination based on the knowledge obtained from the patient’s medical history and from the results of the eye examination alone, without the benefit of diagnostic tests or procedures.
The patient’s clinical diagnosis is metallic corneal foreign body based on the following clinical findings:
- Foreign body embedded in the cornea
- Patient history
Treatment Plan
To gather the clinical information required to remove the corneal foreign body, a diagnostic and treatment program is initiated.
- Determination of different types of diagnoses
- Selection of one or more treatment options
After a clinical diagnosis has been determined, the diagnostic process continues with a process that involves the identification and exclusion of differential diagnoses.
The differential diagnostic process allows the doctor to distinguish betwen two or more diseases with similar signs and symptoms by systematically comparing their signs and symptoms. If the foreign body is readily visible, the differential diagnosis is non-existent. There are other concerns of co-morbidity that should be considered. These include:
Risk of penetration
- Globe penetration is the most significant concern when a patient presents with a history of ocular trauma. This would be of greater concern when the history includes exposure to a high speed projectile or trauma from a sharp object
Risk of infection
- Due to the acute presentation with most corneal trauma, a secondary infection on initial presentation would be exceptionally rare. In the unusual case of delayed reporting, infection must be a concern. If the trauma involves organic or plant material, the risk of a delayed fungal infection must be considered
Risk of recurrent corneal erosion
- The risk of recurrent corneal erosion is highest when the initial trauma was from organic sources and/or when the initial wound is not cared for in the proper manner
Risk of scarring/loss of vision
- If the initial trauma is within the visual axis and extends past the anterior basement membrane, the risk of scarring is high
Ordering Diagnostic Tests
When additional clinical information is needed to complete the differential diagnostic process or to assist in the treatment program, diagnostic tests or services are ordered. The performance of these tests and/or services leads to the completion of the differential diagnostic process while simultaneously initiating the treatment program.
Based on a clinical diagnosis of corneal foreign body, the following diagnostic test was ordered at the conclusion of the eye examination.
- External ocular photography
External Ocular Photography
In any case of ocular trauma that could result in functional vision loss, photodocumentation of the involved tissue could be warranted.
- Documents the damage to the eye from the initial foreign body
- Documents the normal or abnormal response to the trauma
- Documents any postoperative complications
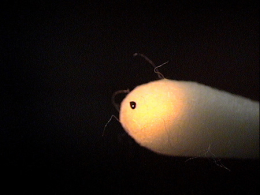
Rust Ring Removal with Alger Brush
|
When treating corneal damage, it is imperative that the doctor create a tissue situation where the healing response will be most rapid and the tissue will return to normal or near normal condition depending on the severity of the initial trauma (minimal scarring and proper epithelial adhesion). If the edges of the wound are smoothed with a diamond burr and the bed of the wound cleared of any debris, the likelihood of rapid healing is maximized and the risk of future corneal erosion is minimized.
With metallic foreign bodies, it is common if not expected to have a certain degree of rust in the underlying tissue layers. While most of the rust can be removed on initial presentation, the doctor can easily consider leaving some of the rust behind in lieu of invading deeper corneal layers which can result in scarring. Over time, the residual rust migrates forward and can be more easily removed.
According to Current Procedural Terminology, when eye doctors perform ophthalmological examinations, the complexity of medical decision-making is not separated from the examining techniques used. However, as a tool to assist eye doctors in enhancing their medical decision-making skills, consider that the complexity of medical decision-making in this case report involves three components.
Diagnosis Guidelines
The first component concerns the number of possible diagnoses and treatment options that must be considered. The diagnosis of a corneal foreign body is relatively straight forward. The actual treatment requires surgical expertise but the postoperative management is again fairly straight forward.
The second component concerns the amount and complexity of medical records and diagnostic tests that have to be obtained, reviewed and analyzed. In addition to an eye examination, this visit required the review and analysis of external photodocumentation.
Third, the complexity of medical decision-making is affected by the risk of significant complications and/or morbidity associated with a corneal foreign body and intra-operative and postoperative complications of the surgical treatment. Although corneal foreign bodies usually respond to treatment with minimal postoperative complications, failure to treat lesions in the proper manner can result in scarring and loss of vision, recurrent corneal erosion and/or secondary infection.
Treatment Options
Treatment of a corneal foreign body begins with removal of the foreign particle, but, only after assessing the eye for possible penetration. Most all corneal foreign bodies can be removed behind a slit lamp or in free space using additional magnification as needed with loops or spectacle magnifiers. Superficial foreign bodies are easily removed with spuds, bent needles, surgical sponges or sometimes with simple direct irrigation. Removal of the material is only half the job.
Metallic Foreign Body Removal
|
 |
Prophylactic, broad spectrum topical antibiotics are recommended until the epithelium has completely healed. Polytrim drops, erythromycin ointment and other kerato-friendly antibiotics are good considerations in lieu of the most current mega-antibiotic. Bandage contact lenses provide enhanced patient comfort and promote faster healing. Unless the wound area is large, a bandage contact lens and oral NSAIDs are sufficient for pain control. In cases of more tissue damage, narcotic pain medications can be prescribed but should not be necessary more than a day or two.
To ensure rapid healing and prevent future complications, the wound must be treated just like any other wound on the body. If the edges are ragged or edematous, a tapered healing edge can be created with a diamond burr. The same burr can be used to remove any microscopic particles from the bed of the wound and smooth the basement membrane. Even with removal of additional tissue, a well-cared for wound will heal much faster and almost eliminate the risk of future recurrent erosion.
Treatment Program
The patient was provided with surgical consent prior to removing the foreign body. After two drops of tetracaine, the material was easily dislodged with a bent needle and much of the rust present removed as well. The edges of the wound were smoothed with a rotating diamond burr. One drop of 1% cyclogyl was instilled. A bandage lens was applied and polytrim ophthalmic drops prescribed t.i.d. until instructed otherwise. The patient was seen the following day and more rust was easily removed with an alger brush. Another bandage lens was applied and the patient examined in two days at which time there was 100% epithelial cover. The patient was asked to return in three days for the next progress examination.
Based on patient history, the nature of the presenting problem, and my own clinical judgement this patient did not need an evaluation of the complete visual system.
- Perform the eye examination that is medically necessary
- Provide the diagnostic tests or services that are medically necessary
- Properly document the services provided
- Code from the documentation
- Report the services to the payor
| Diagnosis Code | Procedure Code | Modifier | Quantity | Payor | Amount Allowed |
| H57.12 - Ocular pain, left eye | 92002 - Medical eye examination | 25 | 1 | Self | 90.00 |
| T15.02XA - Foreign body in cornea, left eye, initial encounter | 65222 - Corneal foreign body removal | 1 | Self | 125.00 | |
| Total | $215.00 |
The fees presented are made up and do not represent any allowable fee or any fee recommendation to you.
Coding Alerts
Some medical insurance companies do not pay for an eye examination on the same day a minor surgical procedure is performed, even if the -25 modifier is appended to the examination. In these cases, report the surgical procedure only.
Although you could report the bandage contact lens as a separate service with CPT code 92071, the lens that was applied on the initial visit was included in the surgical service.
Foreign body in cornea, right eye
initial encounter
T15.01XD
Foreign body in cornea, right eye
subsequent encounter
T15.01X5
Foreign body in cornea, right eye
sequela
T15.02XA
Foreign body in cornea, left eye
initial encounter
T15.02XD
Foreign body in cornea, left eye
subsequent encounter
T15.02X5
Foreign body in cornea, left eye
sequela
930.0
Foreign body in cornea
92285
External ocular photography
65222
Corneal foreign body removal
92071
Bandage contact lens




 Print | Share
Print | Share