Case Report ID: 4
Title:
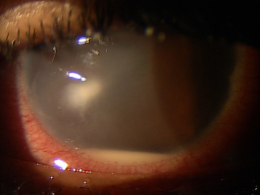
Corneal Delle Secondary to Conjunctival Chemosis
Category:
Description:
A corneal delle is a form of exposure keratoconjunctivitis. It represents an area of localized corneal thinning that usually appears as a small depression in the corneal periphery. The natural history of corneal delle formation is characterized by the following clinical events:
- Delle is produced when the corneal stroma loses an excessive amount of water
- Loss of water leads to stromal dehydration and reduced stromal thickness
- Loss of water is caused by improper wetting of the corneal surface by the tear film
- Poor wetting is usually caused by an elevated mass on the conjunctiva directly adjacent to the limbus
- The elevated mass (conjunctival chemosis) prevents the eyelid from wetting the corneal surface with the blink
Case Report
- An 18-year-old Hispanic man presented to the office with a chief complaint of eye pain
- Case history described acute ocular discomfort that began upon awakening 3-4 hours earlier
- The patient had an unremarkable eye examination five months earlier
Conclusion
A large corneal delle can look threatening. However, once the lesion is correctly diagnosed, simple corneal rehydration with artificial tears will usually resolve the condition.
History of Present lllness
- Associated Signs and Symptoms: epiphora with exposure to bright light
- Location: right eye
- Duration: four hours
- Quality: described as a foreign body sensation
- Context: constant
- Severity: moderate eye pain
- Timing: eye pain was getting worse
- Modifiers: none
Temporal history revealed no prior symptoms, clinical signs or initiating insults that might have caused the eye pain. He had some vague complaints of non-specific irritation he described as a dry or gritty sensation. He had previously worn contact lenses but they had not been used in several months.
Review of Systems
- The patient reported that he was in good health and taking no medications
Past, Family and Social History
- Non-contributory
Best Corrected Visual Acuity
- 20/20 in the right eye
- 20/20 in the left eye
Normal Examination Findings
- Mental status
- Pupils
- External examination
Not Performed on Today’s Examination
- Gross visual fields
- Basic sensorimotor examination
- Ophthalmoscopy
Intraocular Pressure Measurements
- 16mm Hg in the right eye
- 18mm Hg in the left eye
General Medical Observation
- The patient presented as a well-nourished male in mild distress secondary to his eye pain
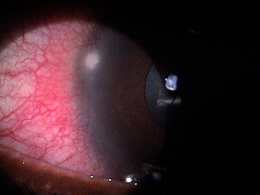
Adnexal Examination
- Upper right eyelid demonstrated a very mild ptosis
- Upper right eyelid red and swollen
External Ocular Examination with Biomicroscopy
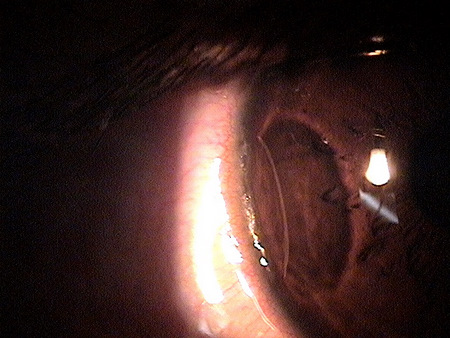
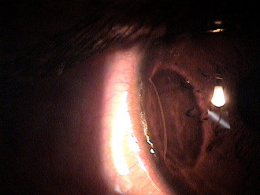
- Begin the biomicroscopic examination with an overview of the cornea using low magnification
- Use a diffuse illumination technique for the initial assessment
- Evaluate corneal delle using a narrow slit beam to assessment the level of corneal depression
Clinical Diagnosis
Clinical diagnoses are determined based on the knowledge obtained from the patient’s medical history and from the results of the eye examination alone, without the benefit of diagnostic tests or procedures.
The patient’s clinical diagnoses are corneal delle and acute allergic conjunctivitis based on the following clinical findings:
- Abnormal appearance of the right eyelid
- Abnormal appearance of the right cornea
- Abnormal appearance of the right conjunctiva
- Nature of the presenting problem
Treatment Plan
To gather the clinical information required to a peripheral corneal delle and acute allergic conjunctivitis, a diagnostic and treatment program is initiated.
- Determination of different types of diagnoses
- Selection of one or more treatment options
After a clinical diagnosis has been determined, the diagnostic process continues with a process that involves the identification and exclusion of differential diagnoses.
The differential diagnostic process allows the doctor to distinguish between two or more diseases with similar signs and symptoms by systematically comparing their signs and symptoms. Potential conditions with similar presentations to corneal delle could include the following:
- Contact lens-induced peripheral corneal ulcer
- Early microbial keratitis
- Marginal keratitis
- Corneal phlyctenulosis
Ordering Diagnostic Tests
When additional clinical information is needed to complete the differential diagnostic process or to assist in the treatment program, diagnostic tests or services are ordered. The performance of these tests and/or services leads to the completion of the differential diagnostic process while simultaneously initiating the treatment program.
Based on a clinical diagnosis of corneal delle secondary to acute allergic conjunctivitis, the following diagnostic tests were ordered at the conclusion of the eye examination.
- External ocular photography
- Anterior segment imaging
- Corneal pachymetry
External Ocular Photography
Any case of compromised tissue could pose a threat to visual function could justify the medical necessity of photodocumentation. In this case, the compromised cornea posed risks of infection, perforation, and a loss of vision. Photodocumentation of the cornea provides a baseline to monitor disease regression and the efficacy of treatment.
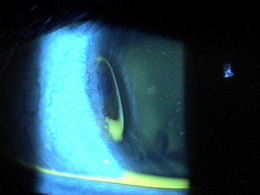
Anterior Segment Imaging
- Scanning laser imaging can provide high-resolution documentation of the corneal tissue
- Tools in the Visante OCT enable non-contact measurement of corneal thickness to support the evaluation of ocular health
 |
Peripheral Corneal Delle
|
Physical Diagnosis
Completion of the differential diagnosis process either returns you to the original clinical diagnosis or it produces a more substantiated physical diagnosis. This component of the diagnostic and treatment program, the determination of a physical diagnosis, is accomplished by studying the physical manifestations of health and illness revealed in the eye examination, the patient’s complete medical history, and supported by various diagnostic tests and procedures.
This component of the diagnostic and treatment program, the determination of a physical diagnosis, is accomplished by studying the physical manifestations of health and illness revealed in the eye examination, the patient’s complete medical history, and supported by various diagnostic tests and procedures.
The diagnostic tests results produced a more substantiated physical diagnosis of corneal delle secondary to allergic conjunctival edema.
This patient presents with a four hour history of eye pain.
According to Current Procedural Terminology, when eye doctors perform ophthalmological examinations, the complexity of medical decision-making is not separated from the examining techniques used. However, as a tool to assist eye doctors in enhancing their medical decision-making skills, consider that the complexity of medical decision-making in this case report involves three components.
Diagnosis Guidelines
The first component concerns the number of possible diagnoses and treatment options that must be considered. The diagnosis and treatment of a corneal delle is predicated on making the proper diagnosis and on understanding the natural history of corneal delle formation.
The second component concerns the amount and complexity of medical records and diagnostic tests that have to be obtained, reviewed and analyzed. In addition to an eye examination, this visit required the review and analysis of an anterior segment imaging examination and external photodocumentation.
Treatment Guidelines
Third, the complexity of medical decision-making is affected by the risk of significant complications and/or morbidity associated with corneal delle and allergic conjunctival edema and the risks involved in any treatment options. Although corneal dellen usually respond to minimal treatment, failure to treat lesions can result in ocular irritation, epithelial breakdown and secondary infection.
Treatment Options
To begin the treatment of a corneal delle, the eye doctor must rehydrate the cornea. This can be accomplished by prescribing artificial tears, lubricating ointments, bandage contact lenses or punctal occlusion. Any initiating insults should be treated concurrently. In his patient, treatment of the acute conjunctivitis was required to eliminate the chemosis that produced the corneal delle.
Treatment was initiated in the office. First, one drop Naphcon A was instilled into the right eye. Naphcon A is a vasoconstrictor/antihistamine. Ten minutes after the first drop was instilled, one drop of Pataday ophthalmic solution (Alcon Laboratories, Inc.) was instilled into the right eye. Pataday is an antihistamine/mast cell stabilizer that prevents the allergic response by blocking the H1 receptors and by stopping the cascade of pro-inflammatory chemical mediators. After another 10 minutes, a drop of unpreserved Systane artificial tears (Alcon Laboratories, Inc.) was instilled in the right eye.
Tobradex ophthalmic ointment (Alcon Laboratories, Inc.) was then prescribed b.i.d. right eye and Systane artificial tears t.i.d. right eye until the patient returned to the clinic. The patient was scheduled for a follow-up examination in two days.
Some authorities do not recommend antimicrobial prophylaxis as the epithelium is intact.
Based on patient history, the nature of the presenting problem and my own clinical judgment, this patient did not need an evaluation of the complete visual system.
- Perform the eye examination that is medically necessary
- Provide the diagnostic tests or services that are medically necessary
- Properly document the services provided
- Code from the documentation
- Report the services to the payor
| Diagnosis Code | Procedure Code | Modifier | Quantity | Payor | Amount Allowed |
| H16.211 - Exposure keratoconjunctivitis, right eye | 92012 - Medical eye examination | 1 | United Healthcare | 69.92 | |
| H16.211 - Exposure keratoconjunctivitis, right eye | 92285 - External ocular photography | 1 | United Healthcare | 41.42 | |
| H16.211 - Exposure keratoconjunctivitis, right eye | 92312 - Anterior segment imaging | 1 | United Healthcare | 40.66 | |
| Total | $152.00 |
Coding Alert
Some medical insurance companies consider anterior segment imaging to be “experimental or investigational” and do not consider the service to be medically necessary.
H16.211
Exposure keratoconjunctivitis,
right eye
370.34
Exposure keratoconjunctivitis
92285
External ocular photography
92132
Anterior segment imaging
76513
Anterior segment ultrasound
92015
Refraction
92071
Bandage contact lens




 Print | Share
Print | Share