Case Report ID: 45
Title
Branch Retinal Vein Occlusion
Category
Other Retinal Diseases (2)
Description
This case presents the diagnosis and treatment of branch retinal vein occlusion and it’s complications.
A branch retinal vein occlusion (BRVO) is a common intraretinal vascular event. It is caused by the occlusion of one of the branches of the central retinal vein, and is usually located distal to the central retinal vein’s bifurcation. Although most branch vein occlusions occur in patients with systemic vascular disease, the events may occur spontaneously and without cause.
Case Report
- A 66-year-old black woman returned to the office after 45 months
- The patient was lost to follow-up and was under the care of a local general ophthalmologist during the the interval
- The patient had been examined 3 months earlier by the ophthalmologist and wanted to return to our office for future care
Conclusion
This case highlights that there is sometimes no preferred practice guidelines to follow and that different eye doctors take care of patients different ways.
History of Present Illness
- Associated Signs and Symptoms: none
Review of Systems
The patient reported that she was in reasonably good health……..
Past, Family and Social History
Non-contributory.
Best-corrected distance visual acuity
- 20/200 in the right eye
- 20/20- in the left eye
Intraocular Pressure Measurements
- 12 mm Hg in the right eye
- 14 mm Hg in the left eye
Normal Examination Findings
- Mental status
- General medical observation
- Gross visual fields
- Basic sensorimotor examination
- External examination
- Adnexal examination
- External ocular examination with biomicroscopy
- Ophthalmoscopy
 |
 |
Clinical Diagnosis
The clinical diagnosis is a determination based on the knowledge obtained from the patient’s medical history and from the results of the eye examination alone, without the benefit of diagnostic tests or procedures.
The patient’s clinical diagnosis is a branch retinal vein occlusion (BRVO) based on her medical history and the clinical appearance of the condition.
Treatment Plan
To gather the clinical information required to treat branch retinal vein occlusion (BRVO), the following diagnostic program could be considered, with emphasis on OCT testing first and visual field analysis second:
- Macula OCT scan
- Threshold visual field examination
- Fundus photography
- Gonioscopy
Differential Diagnoses
Ocular Ischemic Syndrome (Carotid Occlusive Disease) — Patient will have dilated and irregular veins, but they will not be tortuous like in CRVO. Neovascularization is present in a third of patients, but disc edema and hemorrhage are not common. Retinal hemorrhages are found in the mid-periphery of the retina. There will be a history of transient ischemic attacks, amaurosis fugax and orbital pain. Intraocular pressures are is usually low.
Diabetic Retinopathy — The hemorrhages and microaneurysms are concentrated in the posterior pole and exudates are more common. It is usually bilateral.
Papilledema — There will be bilateral disc swelling with flame-shaped hemorrhages around the disc, but not into the peripheral retina. Etiology is caused from increased intracranial pressure rather from a vascular etiology.
Radiation Retinopathy — There is a history of radiation therapy. Patients will have disc swelling and retinal neovascularization, and cotton wool spots.
Ordering Diagnostic Tests
Based on the clinical diagnosis of BRVO, the following diagnostic tests and procedures could be considered at the conclusion of the eye examination.
- Refraction
- Extended ophthalmoscopy
- Fundus photography
- Gonioscopy
- Visual field examination
- Color vision examination
- Electroretinography
- Review of systems
- Laboratory analysis
The decision to order and perform additional testing is totally based on the concept of medical necessity which can only be determined by the examining optometrist or ophthalmologist.
Refraction
- Measurement of visual function / visual acuity
- Visual acuity of 20/400 or worse with correction along with signs of an afferent pupillary defect and visual field constriction are signs of an ischemic BRVO.
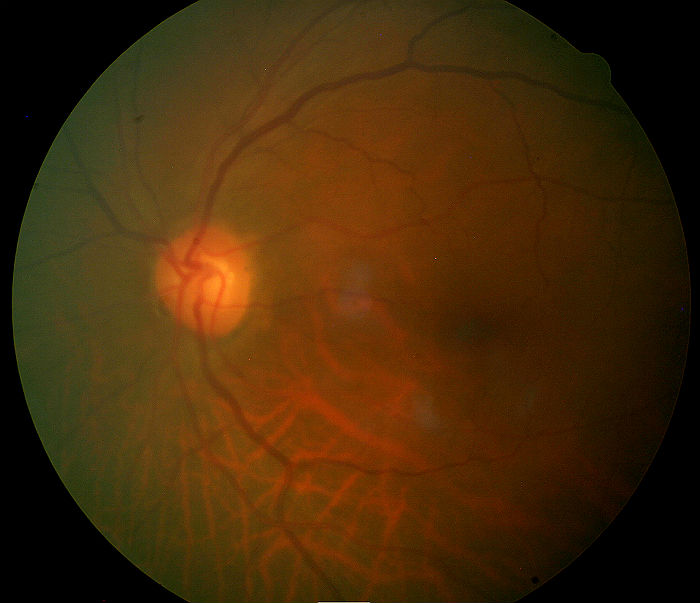
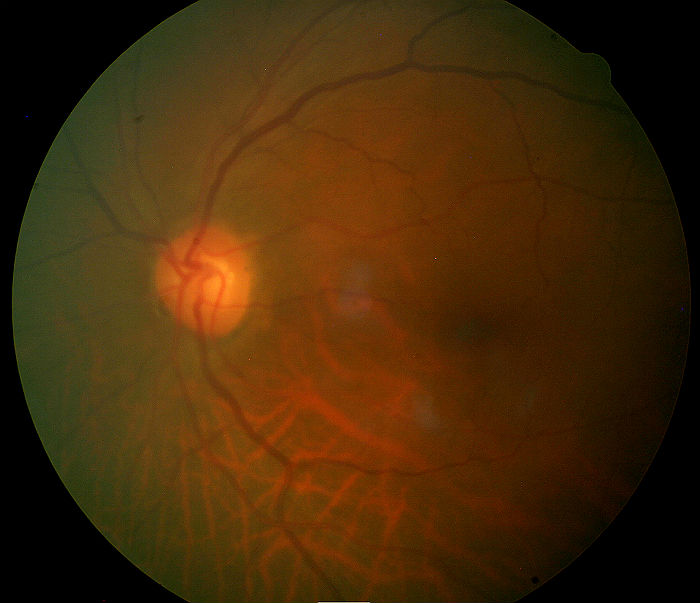
Fundus Photography
- To evaluate the optic nerve, macula and the retina
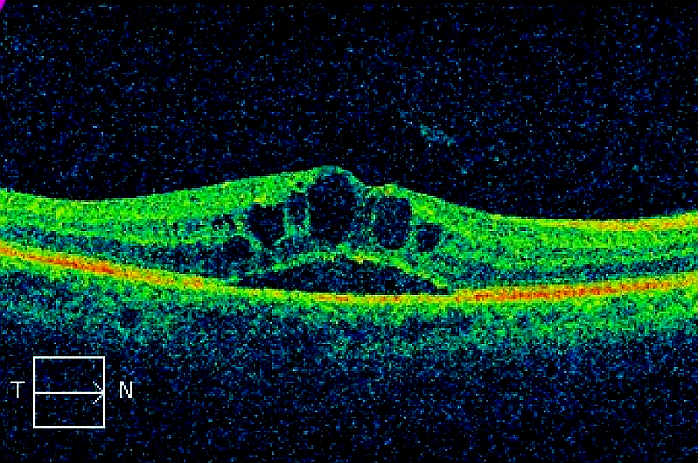
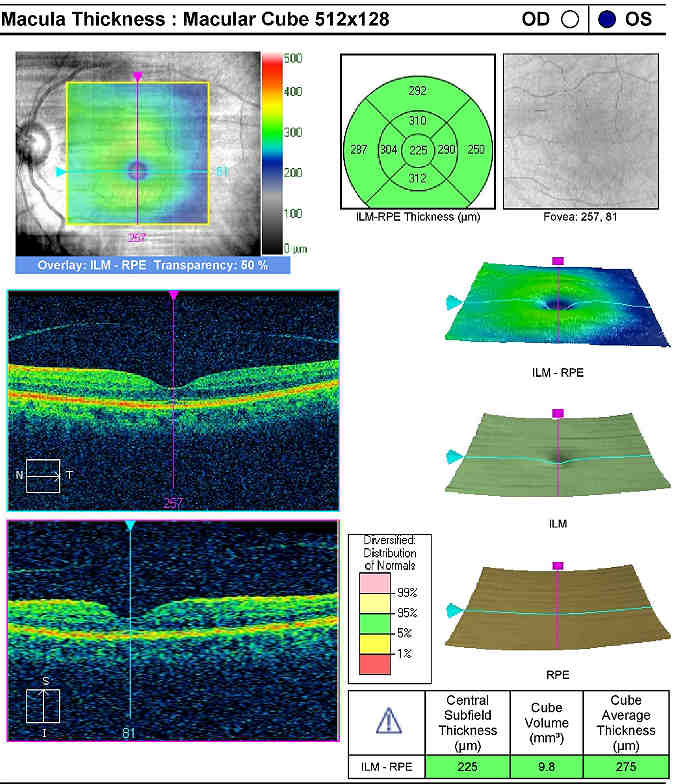
Retinal Laser Scan — Nerve Fiber Layer
- Measuring retinal thickness and detailed evaluation of the retinal anatomy is a means to evaluate overall retinal health
- The procedure can be accomplished with the Cirrus OCT manufactured by Zeiss Meditec
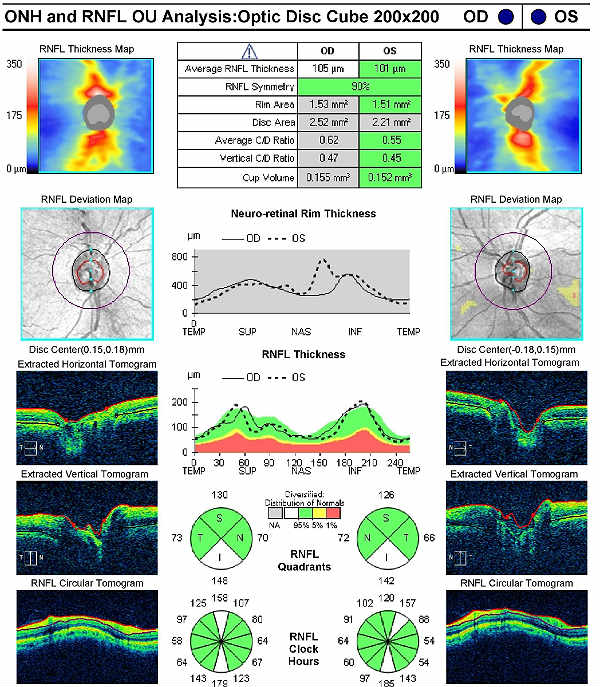 |
Right Eye
Left Eye
Both Eyes
|
Gonioscopy
Any patient with a history of ischemic eye disease should receive a gonioscopic examination of the anterior chamber angle to look for any of the following:
- Fibrovascular membranes
- Neovascular blood vessels
- Angle-closure
Systemic Evaluation
Eye doctors should consider a systemic evaluation in cases of branch retinal vein occlusion. A typical investigative protocol would include the following tests:
Blood Work
- Complete blood count (CBC)
- Westergren sedimentation rate (ESR)
- Lipid profile
- Fasting blood sugar/HbA1C
- Fasting treponemal antibody absorption test (FTA-Abs)
- Reactive plasma reagin (RPR)
- Homocysteine
- Protein S and C
- Lupus anticoagulant
- SickleDex
- Rheumatoid factor
- Purified protein derivative (PPD)
- Lyme titer
- Angiotensin converting enzyme (ACE)
- Antinuclear antibody (ANA)
Ancillary Testing
- Carotid Doppler
- Electrocardiogram (EKG)
- Chest X-ray
Treatment Guidelines
No known effective medical treatment is available for either the prevention of or the treatment of branch retinal vein occlusion (BRVO). Identifying and treating the systemic medical problems is the best treatment to reduce further complications from BRVO.
Vein occlusions are often associated with systemic disease, so co-manage these patients with an internist. Since the exact pathogenesis of BRVO is unknown, various medical modes of treatment are available with varying success in preventing complications and in preserving vision.
The following treatments are advocated:
- Aspirin
- Anti-inflammatory agents
- Isovolemic hemodilution
- Plasmapheresis
- Systemic anticoagulation with warfin, heparin and alteplase
- Fibrinolytic agents
- Systemic corticosteroids
- Local anticoagulation with intravitreal injection of alteplase
Although fluorescein angiography is the gold standard in assessing retinal vascular disease, it is not indicated initially for BRVO patients because the fresh hemorrhage will block transmission and reveal no useful information. In the later course of the occlusion, fluorescein angiography will give information about retinal capillary perfusion and whether or not the occlusion is ischemic and therefore more likely to develop neovascularization.
Treatment Program
Observation for spontaneous resolution is an option in eyes with 20/40 vision or better. Even in the presence of mild macular edema, some patients may decline intravitreal anti-VEGF injections or laser surgery. In patients where observation is chosen as the initial treatment option, follow-up examinations may be performed at 3-month intervals. Non-surgical treatment involves close monitoring of the condition both on a home and clinical basis to maximize the earliest detection of further vision deterioration. This is best accomplished by home Amsler grid testing and repeat ophthlalmoscopic evaluations including OCT analysis.
Based on patient history, the nature of the presenting problem and my own clinical judgment, this patient needed an evaluation of the complete visual system.
- Perform the eye examination that is medically necessary
- Provide the diagnostic tests or services that are medically necessary
- Properly document the services provided
- Code from the documentation
- Report the services to the payor
Physicians Quality Reporting System
PQRS Measure 226: Patient screened for tobacco use and identified as a non-user of tobacco – CPT code 1036F
This measure applies to patients 18 years and older. The measure should be reported on the day of the examination and can be used with any diagnosis code.
PQRS Measure 130: Current Medicatons with Name, Dosage, Frequency and Route Documented – CPT code G8427
This measure applies to patients 18 years and older. The measure should be reported on the day of the examination and can be used with any diagnosis code.
Multiple Procedure Payment Reduction
Effective January 1, 2013, there is a small reduction in payment from Medicare if certain multiple procedures are billed on the same day. The fee for the technical component of the diagnostic test for the second and subsequent tests will be reduced by 20%. The second diagnostic test and subsequent tests should be reported with a -51 modifier. Professional services such as gonioscopy, extended ophthalmoscopy and provocative glaucoma testing are excluded from this policy. Visual evoked potential testing is excluded from this policy.
Modifier 51
This modifier is used to identify the secondary procedure or when multiple procedures are performed on the same day by the same provider. List the major primary procedure first and append the modifier to the subsequent procedures. The primary procedure is the one with the highest dollar value.
Modifier 59
This modifier is used to identify a distinct procedural service for the same patient, on the same day, by the same provider. Documentation must support one of the following not ordinarily encountered or performed on the same day by the same doctor. A different diagnosis code is not necessary to use the -59 modifier.
- Different procedure or surgery
- Different session or patient encounter
- Separate incision or excision
- Separate lesion
According to the Centers for Medicare and Medicaid Services, modifier -59 should not be used to bypass a National Correct Coding Initiative edit. In this case, optical coherence tomography was necessary to document the cystoid macular edema.
| Diagnosis Code | Procedure Code | Modifier | Quantity | Payor | Amount Allowed |
| H34.831 - Branch retinal vein occlusion, right eye | 92004 - Medical eye examination | 1 | Medicare | 152.61 | |
| H34.831 - Branch retinal vein occlusion, right eye | 92250 - Fundus photography | 1 | Medicare | 80.74 | |
| H40.11X1 - Primary open-angle glaucoma, mild stage | 92283 - Visual field examination | 51 | 1 | Medicare | 72.38 |
| H35.351 - Cystoid maculae degeneration, right eye | 92134 - Macula OCT scan | 51, 59 | 1 | Medicare | 44.31 |
| H34.831 - Branch retinal vein occlusion, right eye | 1036F - Patient screened for tobacco use | 1 | Medicare | 0.00 | |
| H34.831 - Branch retinal vein occlusion, right eye | G8427 - Current medication documented | 1 | Medicare | 0.00 | |
| Total | 350.04 |
H34.831
Branch retinal vein occlusion,
right eye
362.36
Branch retinal vein occlusion
92134
Macular OCT scan
92250
Fundus photography
92020
Gonioscopy
92083
Visual field examination
92225
Extended ophthalmoscopy
92283
Extended color vision examination
92275
Electroretinography




 Print | Share
Print | Share