Case Report ID: 11
Title:
Anterior Uveitis
Category:
Anterior Segment Disease (3)
Description:
This case presents the diagnosis and treatment of anterior uveitis.
Anterior uveitis represents an inflammation of the uveal tissues, primarily the iris and the ciliary body. This inflammation may be associated with underlying systemic disease or autoimmunity, or it may occur as a direct result of ocular trauma.
Anterior uveitis is classified by its anatomical location:
- Iritis – Inflammation primarily involving the iris
- Iridocyclitis – Inflammation involving the iris and the ciliary body
This differentiation is often academic and difficult to make as the inflammation typically will involve both structures to some degree.
Case Report
- A 43-year-old Hispanic man presented for an emergency examination with a complaint of red eye
- Case history revealed that the only visual complaint was difficulty when reading and driving
- This was the second episode of red eye in the past 14 months, although the initial episode involved the other eye
Conclusion
The patient has recurrent iritis. The course of the disease is characterized by repeated episodes of iritis separated by periods of inactivity without treatment lasting at least 3 months. Best practice guidelines for recurrent iritis include a Uveitis Evaluation to investigate the etiology of the presentation.
History of Present Illness
- Associated Signs and Symptoms: mild pain with globe palpation
- Location: left eye
- Duration: 3 days
- Quality: described as a dull ache
- Context: constant
- Severity: moderate eye pain
- Timing: eye pain was getting worse
- Modifiers: none
Review of Systems
- The patient reported that he was in good health and taking no medications
- He did report chronic lower back pain but felt this was more associated with his job as a construction worker
Past, Family and Social History
- The patient had experienced an identical red eye episode 14 months earlier
Uncorrected Distance Visual Acuity
- 20/20 in the right eye
- 20/50 in the left eye
Normal Examination Findings
- Mental status
- External examination
- Ophthalmoscopy
Not Performed on Today’s Examination
- Gross visual fields
- Basic sensorimotor examination
General Medical Observation
- A well-nourished male in mild distress secondary to eye pain
Intraocular Pressure Measurements
- 13 mm Hg in the right eye
- 10 mm Hg in the left eye
Low intraocular pressure is normal in anterior uveitis because of a reduction in aqueous production from the ciliary epithelium. As the disease progresses, the pressure may actually go up due to accumulation of inflammatory debris in the trabeculum.
Clinical Diagnosis
The clinical diagnosis is a determination based on the knowledge obtained from the patient’s medical history and from the results of the eye examination alone, without the benefit of diagnostic tests or procedures.
The patient’s clinical diagnosis is acute anterior uveitis based on the previous ocular history and the following clinical findings:
- Unilateral circumcorneal hyperemia
- Aqueous cells in the anterior chamber
- Aqueous flare in the anterior chamber
- Aqueous fibrinous exudate in the anterior chamber
- Posterior synechiae in the anterior chamber
- Low intraocular pressure in the left eye
Treatment Plan
To gather the information required to treat uveitis, a diagnostic and treatment program is initiated.
- Determination of a possible etiology for the acute anterior uveitis
- Selection of one or more treatment options
Uveitis is a disease where the doctor must make the appropriate differential diagnosis to properly recommend steps for patient management. After a clinical diagnosis has been determined, the diagnostic process continues with a process that involves the identification and exclusion of differential diagnoses. The differential diagnosis process allows the eye doctor to distinguish between two or more diseases with similar signs and symptoms by systematically comparing their signs and symptoms.
Differential Diagnoses
The first differential diagnosis that needs to be determined in this patient is anterior uveitis vs. some other general red eye presentation. The list of possible diseases would include any pathology that produces an acute red eye with ocular pain.
The following diseases share some of the clinical signs and symptoms of anterior uveitis and the most significant differences include:
Posterior uveitis with inflammation spreading to the anterior chamber
- More likely to have significant decreased vision
- Less likely to have significant pain response
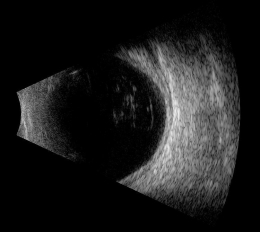 |
B-Scan Ultrasound
|
Corneal trauma
- History of ocular trauma
- Visible epithelial damage
Contact lens-induced red eye
- History of contact lens wear (often abusive)
- Corneal edema
- Corneal infiltrates
- Visible damage to corneal epithelium
Endophthalmitis
- Recent history of ocular surgery or potential ocular penetration
- Severe pain
- Severely reduced vision
- Hypopyon
- Vitritis
Acute angle closure
- Elevated IOP
- Severe pain
- Corneal edema
- Narrow / closed angle
This patient did not present with characteristics common to the other differential possibilities.
Ordering Diagnostic Tests
When additional clinical information is needed to complete the differential diagnostic process, diagnostic tests and procedures are ordered. The performance of these tests and procedures leads to the completion of the differential diagnostic process while simultaneously initiating the treatment program. Based on the clinical diagnosis of anterior uveitis, the following diagnostic tests and procedures could be considered at the conclusion of the eye examination.
- Refraction
- Extended ophthalmoscopy
- External ocular photography
- Specular endothelial microscopy
- Review of systems
- Laboratory analysis
The decision to order and perform additional testing is totally based on the concept of medical necessity which can only be determined by the examining optometrist or ophthalmologist.
Refraction
- Measuring visual acuity is a method of evaluating functional vision loss
- Anterior uveitis, in both the acute and chronic phases, can produce a loss of visual acuity
Extended Ophthalmoscopy
Extended ophthalmoscopy is indicated when a more detailed examination and documentation of the vitreous and retinal structures is indicated than a doctor would conduct in routine examination of the interior globe. Routine ophthalmoscopy is part of general ophthalmologic services and not reported separately. However, extended ophthalmosocpy is reported separately as an additional, billable diagnostic procedure.
Uveitis presentations, especially when there is potential for systemic disease as a co-morbidity, requires a detailed evaluation of the vitreous and retinal structures to look for vitreous cells, exudative material over the ora (snowbanking), cellular material in the vitreous (snowballs), vascular sheathing, peripheral neovascularization and retinal detachment. In this patient, no vitreous or retinal changes were noted even with extended observation of the retina.
In many cases, the degree of presenting photophobia may warrant delaying a more detailed internal evaluation to a follow-up visit, but this evaluation should never be eliminated from the diagnostic evaluation.
External Ocular Photography
Photodocumentation is considered medically necessary when it provides the doctor with a useful tool for assistance in making the clinical diagnosis or assists in monitoring the disease progression or effectiveness of therapeutic intervention. Anterior uveitis, especially with tissue changes demonstrating disease chronicity and potential for secondary complications, is a sight threatening disorder. Photodocumentation of the current tissue changes could easily be considered as medically necessary.
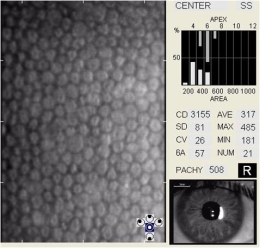
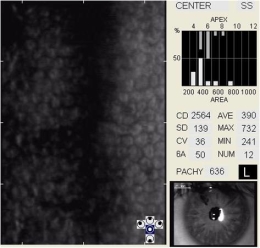
Specular Endothelial Microscopy
Iridocyclitis can result in endothelial cell loss and reduced endothelial function. The condition is called inflammation-induced corneal endotheliopathy and is characterized by the following clinical features:
- Specular microscopy reveals well-demarcated, dark structures usually located at endothelial cell intersections
- These dark structures are thought to represent invading white blood cells (e.g., inflammatory cells)
- Migration of inflammatory cells into the cornea from the anterior chamber produces a sloughing of the endothelium
- More aggressive and/or earlier treatment of any anterior segment inflammation with topical steroids may help with prevention of inflammation-induced endotheliopathy
Uveitis Evaluation / Laboratory Analysis
Eye doctors should not be too quick to suggest a comprehensive systemic evaluation unless truly warranted. Next to trauma, idiopathic etiology is the most common explanation for an acute anterior uveitis. The medical advisability of ordering or referring for a systemic evaluation in patients with anterior uveitis is dependent on several factors including:
- Associated symptoms revealed in a comprehensive review of systems
- History of recurrences
- Presence of clinical findings suggestive of disease chronicity
In this case, the patient reported potential systemic symptoms associated with systemic inflammatory disease (rheumatoid, ankylosing spondylitis), a reported history or recurrent and significant associated tissue changes in the anterior chamber.
A basic uveitis work up could include any or all of the following studies, depending on the level of suspicion each analysis could be associated with.
Primary care eye doctors should communicate as specifically as possible regarding their suspicion of systemic involvement in a patient presenting with anterior uveitis. This can and should be as detailed as recommending specific laboratory analysis based on the suspected systemic disease driving the inflammatory process.
In this presentation, based on the patient’s age, ethnicity, gender and systemic symptoms, a high suspicion existed for ankylosing spondylitis or rheumatoid arthritis.
All of the diagnostic test results confirmed the clinical diagnosis of acute anterior uveitis. The exact etiology could not be determined based on these findings and could only be confirmed through a systemic evaluation.
According to Current Procedural Terminology, when eye doctors perform ophthalmological examinations, the complexity of medical decision-making is not separated from the examining techniques used. As a guideline to assist eye doctors in enhancing their medical decision-making skills, consider that the complexity of medical decision-making involves three components.
The first component concerns the number of possible diagnoses and treatment options that must be considered. Anterior uveitis is a complex disease with multiple potential differentials and potential systemic associations.
The second component concerns the amount and complexity of medical records and diagnostic tests that have to be obtained, reviewed and analyzed. In addition to an eye examination, this visit required the review and analysis of a subjective refraction, extended ophthalmoscopy, external ocular photography and specular endothelial microscopy. Medical decision-making also involved coordination of care with general medicine related to the potential for systemic explanations for the ocular disease.
Third, the complexity of medical decision-making is affected by the risk of significant complications and/or morbidity associated with anterior uveitis and the risks involved in any treatment options. This patient’s anterior uveitis was classified as a significant problem where the risk of total vision loss without treatment was significant and there was significant potential for other systemic co-morbidities. In addition, multiple treatment potentials and coordination of care are essential elements of patients presenting with sight threatening disorders commonly associated with systemic disease.
Treatment Guidelines
Treatment of anterior uveitis is directed at first controlling the underlying ocular inflammation. While the potential for systemic disease association is high, the first concern is minimizing continued ocular damage, preventing or managing any potential secondary disease processes and minimizing the potential for vision loss.
Specific to the diagnosis, the clinical picture points to a clear-cut uveitis presentation. Topical medications can be used to reduce inflammation, attempt to break the posterior synechiae and reduce the factors creating the synechia and risk for uveitic glaucoma. However, topical treamtment should never be delayed pending the systemic evaluation.
Topical steroids are the first and most important component of treating uveitis. Prednisolone acetate 1% is the preferred medication. Initial dosing should be aggressive, usually q1-2h at least for the first 24-48 hours. Alternatively. Durezol (difluprednate) has been shown to produce anti-inflammatory effects equal to prednisolone acetate but at lower dosages and can also be considered. There are many reports of increased problems with steroid response with Durezol. Any steroid with less documented potency should be avoided in the management of even milder uveitis. If the inflammation is not subsiding after several weeks of aggressive topical therapy, oral prednisone or subconjunctival triamcinolone can be considered.
Cycloplegic agents should be considered with moderate-to-severe uveitis. While some feel the cycloplegic effect will decrease ocular pain, the main reason for aggressive cycloplegia is to reduce the potential for posterior synechiae formation. Homatropine 5% or scopolamine b.i.d are excellent choices for synechiae prevention. In a case where posterior synechiae already exist, an attempt can be made to pharmacologically break the synechiae. Homatropine 5% and phenylepherine 10%, both t.i.d., act on both iris dilating muscles creating the best chance of breaking the irido-lenticular adhesions.
Phenylepherine 10% would be contraindicated in patients with cardiovascular disease. Success in pharmacologically breaking synechiae is not guaranteed and many presentations will ultimately require a laser synechialysis. When warranted, a referral for systemic evaluation can be considered.
Treatment Program
After obtaining the patient’s informed consent to treat his recurrent anterior uveitis, prednisolone acetate 1% q2h and homatropine 5% t.i.d. was prescribed. A follow-up visit was scheduled for 24 hours.
Because recurrent anterior uveitis is a vision-threatening disease, many optometrists and ophthalmologists believe that a comprehensive eye examination is required to evaluate the patient. However, because gross visual fields and/or a basic sensorimotor evaluation were not medically necessary on this visit, a comprehensive level service should not be performed or reported.
- Perform the eye examination that is medically necessary
- Provide the diagnostic tests or services that are medically necessary
- Properly document the services provided
- Code from the documentation
- Report the services to the payor
| Diagnosis Code | Procedure Code | Modifier | Quantity | Payor | Amount Allowed |
| H20.022 - Recurrent acute iridocyclitis, left eye | 92012 - Medical eye examination | 1 | United Healthcare | 69.92 | |
| H20.022 - Recurrent acute iridocyclitis, left eye | 92225 - Extended ophthalmoscopy | 1 | United Healthcare | 27.74 | |
| H20.022 - Recurrent acute iridocyclitis, left eye | 92285 - External ocular photography | 1 | United Healthcare | 29.38 | |
| H18.232 - Secondary corneal edema, left eye | 92286 - Specular microscopy | 1 | United Healthcare | 121.04 | |
| Total | $248.08 |
H20.022
Recurrent acute iridocyclitis, left eye
364.01
Primary iridocyclitis
92015
Refraction
92020
Gonioscopy
92285
External ocular photography
92286
Specular endothelial microscopy
76514
Corneal pachymetry
92134
Retinal laser scan|
92132
Anterior segment imaging
92225
Extended ophthalmoscopy




 Print | Share
Print | Share