ICD-10 Diagnosis Codes:
T15.01XA — Foreign body in cornea, right eye,
initial encounter
T15.01XD — Foreign body in cornea, right eye,
subsequent encounter
T15.01X5 — Foreign body in cornea, right eye,
sequela
T15.02XA — Foreign body in cornea, left eye,
initial encounter
T15.02XD — Foreign body in cornea, left eye,
subsequent encounter
T15.02X5 — Foreign body in cornea, left eye,
sequela
Title
Corneal Foreign Body
Category
Foreign Body On External Eye
Description
Corneal foreign body occurs when foreign material becomes lodged on or in the corneal epithelium or stroma.
Structural Damage to the Eye
- Inflammatory cascade begins with damage to the corneal epithelium
- Anterior chamber reaction begins with liberation of white blood cells
- Inflamamtory mediators produce dilation of conjunctival blood vessels
- Mechanical trauma produces edema of the eyelids
- Conjunctival edema develops
- Corneal edema develops
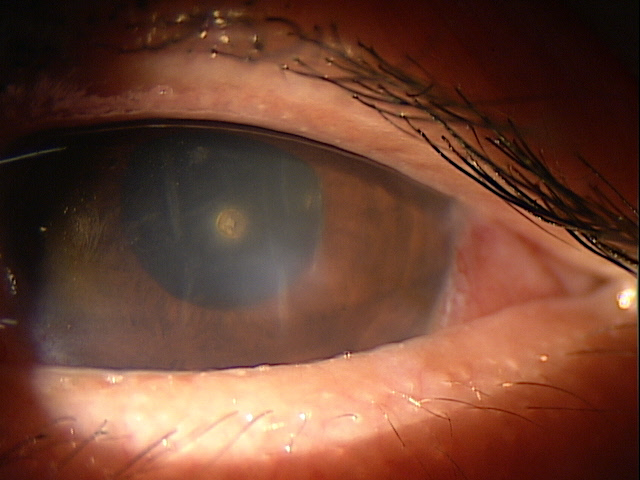 |
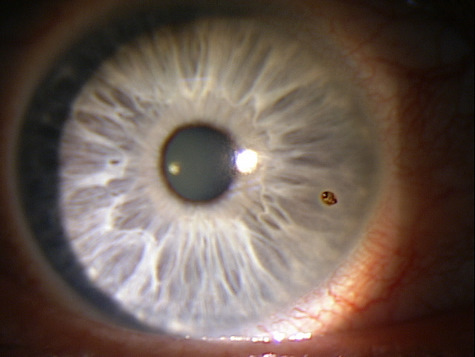
Corneal Foreign Body — Metallic
|
Functional Damage to the Eye
- None
- Temporary loss of vision from corneal edema
- Permanent loss of vision from corneal scarring
There are several goals that need to be met in the diagnostic evaluation of a patient with a corneal foreign body:
- Determine the circumstances of the injury (e.g., using power tools, working under a car, hammering metal, etc.)
- Determine the characteristics of the foreign body (e.g., size of object, speed of object, force of object, etc.)
- Assess the eye for possible penetration by the foreign body
- Relieve pain and discomfort
- Prescribe a treatment program the minimizes the risk of infection, recurrent corneal erosion, and corneal scarring
Patient History
Patients will usually present with a history of ocular trauma. Symptoms range from none to mild foreign body sensation to severe pain. Any of the following abnormal clinical signs or symptoms may be present:
- Ocular pain
- Conjunctival redness
- Blepharospasm
- Swelling of the eyelids
- Tearing
- Photophobia
- Protective pseudoptosis
- Decreased visual acuity
Adnexal Examination
- Document any pseudoptosis of the upper eyelid
- Document any edema of the eyelids
External Ocular Examination with Biomicroscopy
- Evert the upper eyelid and inspect the conjunctival fornices for multiple foreign bodies
- Document the presence or absence of an anterior chamber reaction
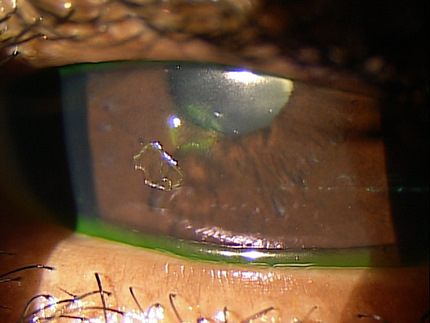
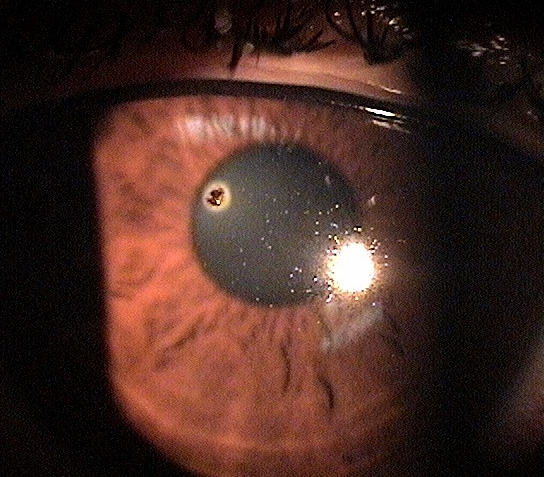
- Determine the size, shape, location and depth of the foreign body
Ophthalmoscopy
- If the history includes exposure to a high-speed projectile, dilate the eye and examine the posterior segment for an intraocular foreign body
DIAGNOSTIC TESTS
External Ocular Photography
- To document the size, shape, location and depth of the foreign body
- To document the delivery of medical/surgical treatment
- To document the response treatment
Anterior Segment Ultrasound
- To identify or exclude an intraocular foreign body in the anterior segment (if a high-speed projectile is involved)
B-Scan Ophthalmic Ultrasound
- To identify or exclude an intraocular foreign body in the posterior segment (if a high-speed projectile is involved)
CT Scan of the Orbit
- To identify or exclude an intraorbital foreign body (if a high-speed projectile is involved)
There is no standard classification system for corneal foreign bodies. In a general sense, they can be classified by the type of material (e.g., glass, plastic, metal, wood, etc.) and/or by the depth of the object.
- Superficial corneal foreign bodies are those that do not penetrate Bowman’s membrane
- Deep corneal foreign bodies are those that penetrate past Bowman’s membrane
If the corneal foreign body is readily visible, the differential diagnosis is non-existent. Although there are no differential diagnoses, other concerns of co-morbidity should be considered.
Intraocular Foreign Body
- Indentify or exclude when the history indicates the possibility of penetration
Intraorbital Foreign Body
- Identify or exclude when the history indicates the possibility of penetration
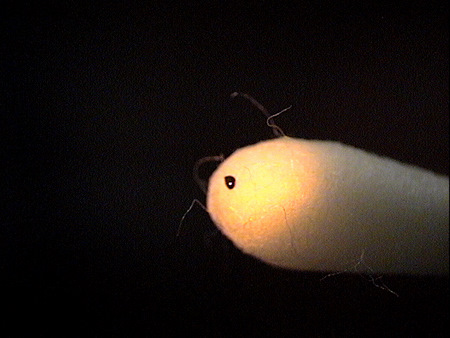
Treatment of a corneal foreign body begins with removal of the foreign particle, but, only after assessing the eye for possible penetration. Most all corneal foreign bodies can be removed behind a slit lamp or in free space using additional magnification as needed with loops or spectacle magnifiers. Superficial foreign bodies are easily removed with spuds, bent needles, surgical sponges or sometimes with simple direct irrigation. Removal of the material is only half the job.
Prophylactic, broad spectrum topical antibiotics are recommended until the epithelium has completely healed. Polytrim drops, erythromycin ointment and other kerato-friendly antibiotics are good considerations in lieu of the most current mega-antibiotic. Bandage contact lenses provide enhanced patient comfort and promote faster healing. Unless the wound area is large, a bandage contact lens and oral NSAIDs are sufficient for pain control. In cases of more tissue damage, narcotic pain medications can be prescribed but should not be necessary more than a day or two.
To ensure rapid healing and prevent future complications, the wound must be treated just like any other wound on the body. If the edges are ragged or edematous, a tapered healing edge can be created with a diamond burr. The same burr can be used to remove any microscopic particles from the bed of the wound and smooth the basement membrane. Even with removal of additional tissue, a well-cared for wound will heal much faster and almost eliminate the risk of future recurrent erosion.
4. Ajamian PC. Bust that rust! RevOptom. 2012 Jan 15; (1): 72.
930.0
Corneal foreign body
92285
External ocular photography
65222
Corneal foreign body removal
92071
Bandage contact lens




 Print | Share
Print | Share