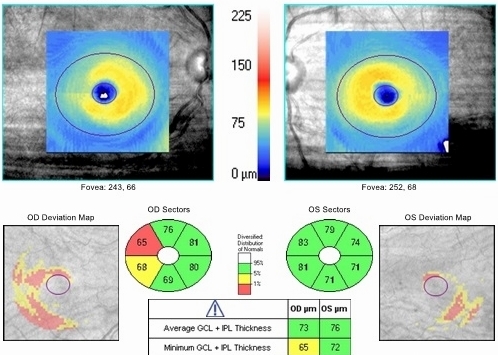
Ganglion cell analysis with Cirrus OCT reveals
plaquenil-induced toxic maculopathy
ICD-10 Diagnosis Codes:
H35.381–Toxic Maculopathy, right eye
H35.382–Toxic Maculopathy, left eye
H35.383–Toxic Maculopathy, bilateral
Title
Toxic Maculopathy Of Retina
Category
Other Retinal Disorders
Description
Medications like plaquenil and chloroquine can induce degenerative changes in the ganglion cells and photoreceptor cells of the retina.
Toxic maculopathy is a form of retinal toxicity that is associated with antimalarial agents such as plaquenil and chloroquine. Both medications are commonly used to treat patients with systemic autoimmune diseases that include the following:
- Lupus
- Sarcoidosis
- Sjogren’s syndrome
- Rheumatoid arthritis
- Post-Lyme disease arthritis
 |
Long-term use of high-risk medications
Recent studies estimate that about 1% of patients develop toxic maculopathy after 5 years of treatment with plaquenil or chloroquine.
|
Risk Factors Associated with Plaquenil-Induced Maculopathy
|
 |
The pathogenic effect of plaquenil is the induction of lysosomal dysfunction in photoreceptors and retinal pigment epithelium (RPE) cells. A lysosome is a membrane-bound organelle found in the cytoplasm of most cells and it contains hydrolytic enzymes that function in intracellular digestive processes. When hydrolytic enzymes are released into the cytoplasm, they cause self-digestion of the cell.
In the normal retina, the retinal pigment epithelium digests the tips of the photorectors by lysosomal action. The digestive process produces yellow-brown fatty pigment granules called lipofuscin. When the photoreceptor tips are digested by lysosomes, a small amount of lipofuscin remains and accumulates in the retinal pigment epithelium cells.
Because excess accumulation of lipofuscin can damage healthy cells, it is removed from the retina through metabolic disposal mechanisms. In patients with plaquenil-induced toxic maculopathy, the release of lysosome is abnormal and this produces an imbalance between lipofuscin formation and disposal.
Structural Damage to the Eye
- Hydroxychloroquine (plaquenil) and chloroquine have an affinity for pigmented ocular structures and binds to melanin in the RPE
- With prolonged exposure, plaquenil accumulates in the retina and disrupts lysosomal function in the retinal pigment epithelium cells
- Lysosomal dysfunction creates abnormal retinal metabolism
- Abnormal metabolism leads to increased phagocytosis of photoreceptor outer segments
- Photoreceptor damage is characterized by defects in the photoreceptor integrity line that are detectable with spectral-domain OCT
- Early clinical signs include perifoveal ganglion cell damage that is characterized by localized thinning of the outer nuclear layer
- Damaged retinal pigment epithelium cells accumulate lipofuscin that is detectable with fundus autofluorescence imaging
- Pigmentary stippling of the retinal pigment epithelium is visible with ophthalmoscopy as the disease progresses
- Cone photoreceptor fallout may result in the loss of the foveal reflex
- Disease progression produces a subtle bull’s eye maculopathy pattern characterized by a central foveal island of pigment surrounded by a depigmented zone of retinal pigment epithelium atrophy which is itself encircled by a hyperpigmented ring
- End-stage disease is characterized by a severe loss of retinal pigment epithelium cells and an obvious bull’s-eye maculopathy pattern
Functional Damage to the Eye
- Multifocal electroretinography is the most sensitive test for early detection of plaquenil-induced functional vision loss
- Early functional vision loss can also be detected with a 10-2 threshold visual field
- Loss of visual acuity is found in the late stages of the disease
- Abnormal color vision is found in the late stages of the disease
- Metamorphopsia on Amsler grid testing is found in the late stages of the disease
The American Academy of Ophthalmology recommends a baseline eye examination within one year of beginning plaquenil to establish a reference and rule out retinal disease that may contraindicate initiation of therapy. After that, annual surveillance examinations should begin after five years unless the patient has risk factors for toxic maculopathy.
The goal of a diagnostic evaluation in a patient taking plaquenil is to accomplish the following:
1. Educate the patient regarding the ocular risks of plaquenil therapy
2. Determine the cumulative dose of plaquenil taken by the patient
3. Determine if the patient has reached the threshold for increased risk of plaquenil-induced toxic maculopathy
4. Determine if the patient has plaquenil-induced toxic maculopathy
- Evaluation with spectral domain OCT testing
- Evaluation with a 10-2 threshold visual field examination
- Evaluation with fundus autofluorescence imaging (FAF)
- Evaluation with electroretinogram (ERG)
5. Determine the frequency of surveillance examinations
For example, if a patient has taken 250 milligrams of plaquenil per day for three years, the cumualtive dose is 273,750 milligrams. This equals 273.75 grams of plaquenil and is below the 1,000 gram threshold for developing toxic maculopathy. Another patient may present with a history of taking 400 milligrams of plaquenil per day for fifteen years. In this patient, the cumulative dose is 2,190,000 milligrams of plaquenil. This equals 2,190 grams of plaquenil and is above the 1,000 gram threshold for developing toxic maculopathy.
The first patient may be screened every few years for toxic maculopathy while the second patient should be examined every six to twelve months.
Patient History
- Patients are usually asymptomatic early in the natural history of the disease
- Generalized visual disturbances may occur as the disease progresses
Clinical Appearance of the Cornea
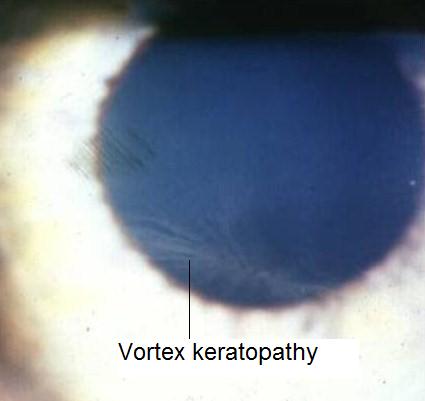 |
Plaquenil-Induced Vortex Keratopathy
|
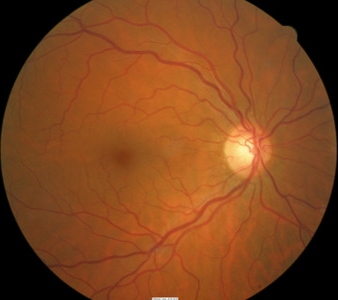
Clinical Appearance of the Retina
- No clinical signs may be visible with ophthalmoscopy in the premaculopathy stage of the disease
- Mild pigmentary stippling of the retinal pigment epithelium may be visible in the early stages of the disease
- Fine granular macular pigmentation may be visible in the early stages of the disease
- Loss of the foveal reflex may appear in early-to-moderate disease
- Formation of concentric zones of hyperpigmentation and depigmentation (e.g., bull’s eye maculopathy) in moderate-to-severe disease
- Optic atrophy in end-stage disease
- Arteriolar attenuation in end-stage disease
DIAGNOSTIC TESTS
Retinal Scanning Laser — Macula
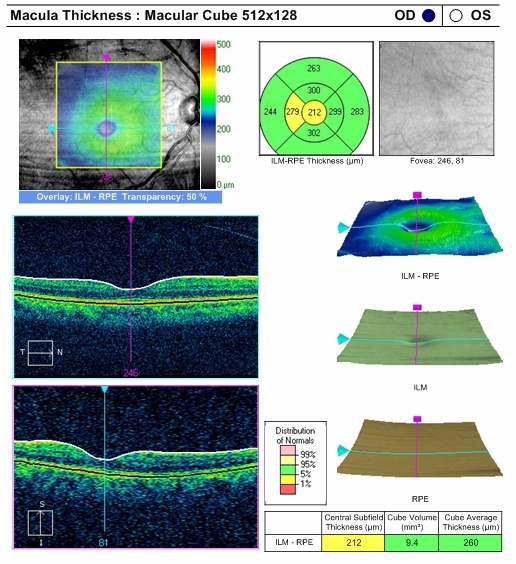
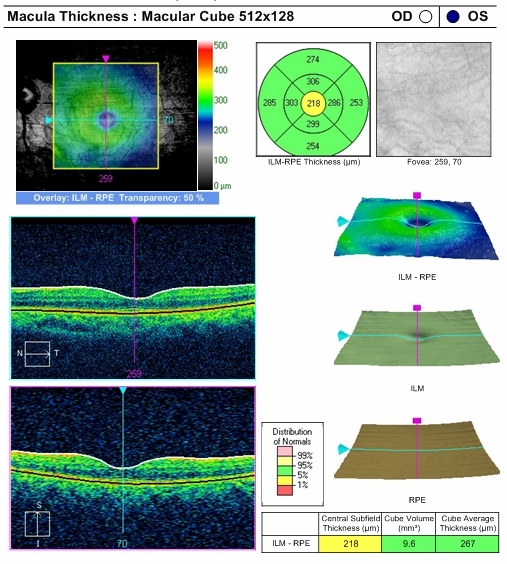
To gather the clinical information required to screen for early detection of plaquenil-induced toxic maculopathy, emphasis is placed on spectral domain OCT testing, particularly ganglion cell analysis.
- Parafoveal thinning may be seen on the macular thickness map imaged with Cirrus OCT
- Right eye reveal a mild decrease in retinal thickness, temporally
- Loss of ganglion cells reduces the height of the “volcano”
- Loss of photoreceptors
- Left eye reveals normal retinal thickness
- Clinically significant asymmetry
 |
 |
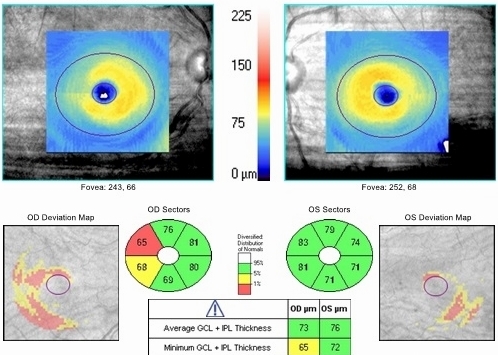 |
Ganglion Cell Complex Analysis
Left Eye
Both Eyes
|
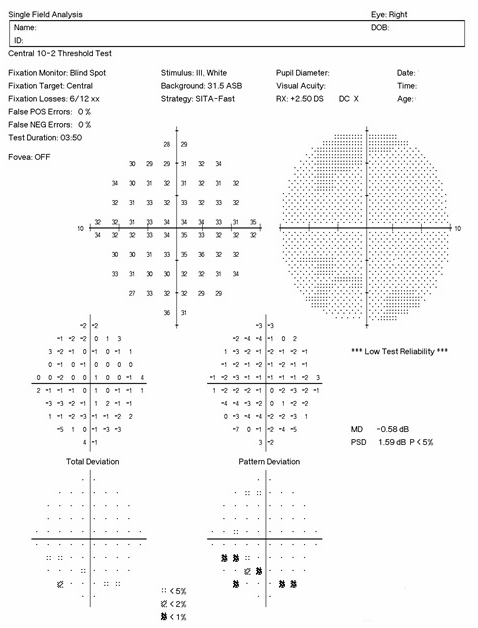
Visual Field Examination
There are several caveats to remember when performing 10-2 visual field examinations on patients taking plaquenil:
- Parafoveal loss of retinal sensitivity may appear before changes are visualized on fundus examination
- Attention should be given to the “Pattern Deviation” to help determine the clinical significance of the test results
- Promptly repeat the examination when central or paracentral visual field defects are observed to determine whether the defects are reproducible
- When visual fields are performed independently, even the most subtle changes or those of uncertain significance should be take seriously are an indication for objective testing
 |
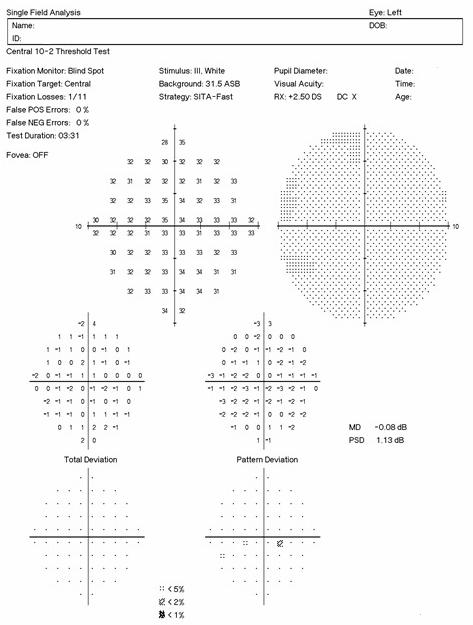 |
Positive findings on 10-2 visual field testing are represented by scattered paracentral scotomas.
- Right eye reveals scattered paracentral scotomas inferiorly
- Left eye’s visual field examination is normal
- Clinically significant asymmetry
Electroretinography
Electroretinography (ERG) testing evaluates the integrity of the retina. Although multifocal electroretinography is the most sensitive diagnostic test for detecting plaquenil-induced retinal function loss, other specialized ERG tests can provide clinically useful information about macular and ganglion cell function.
Interpreting Steady-State Electroretinograph
1. Waveform Shape/Morphology
- There should be 3 distinct sinusoidal humps in each trace
2. Waveform Magnitude
- The threshold of the ERG response should be 1.2 uV or greater
3. Magnitude D
- If the Mag D is 40% or more lower than the waveform magnitude, the ERG response suggests the presence of pathology
4. Contrast sensitivity testing protocol is more diagnostic for glaucoma.
5. Concentric stimulus fields testing protocol is more diagnostic for macular disease.
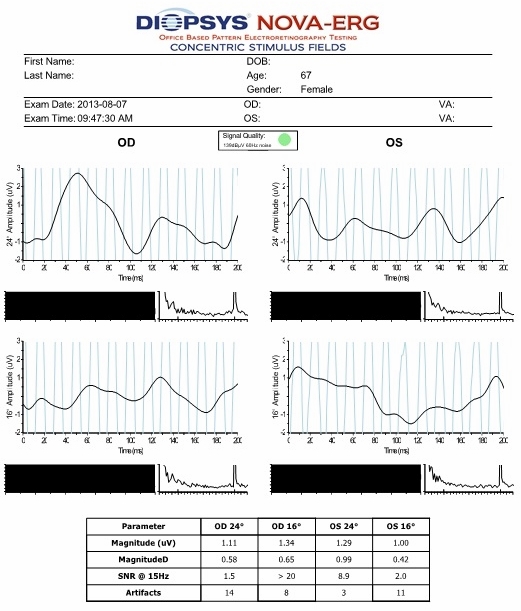 |
Right Eye
Waveform morphology is abnormal
Magnitude of the pERG response is abnormal
Magnitude D is normal
|
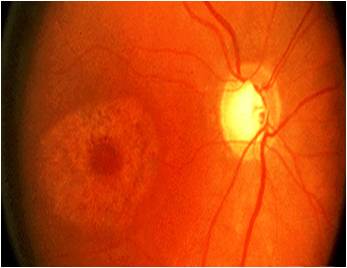
Fundus Photography
Hybrid retinal cameras perform fundus autofluorescence imaging to detect damaged retinal pigment epithelial cells. The damaged cells accumulate lipofuscin and plaquenil-induced toxic maculopathy is characterized by a pericentral ring of increased fundus autofluorescence in the macula.
Plaquenil-induced toxic maculopathy can be divided into the following stages:
Premaculopathy
- Normal visual acuity
- Mild subjective visual disturbances
- Fundus examination may reveal mild pigmentary stippling of the retinal pigment epithelium
Early maculopathy
- Mild reduction in visual acuity
- Mild subjective visual disturbanced
- Fundus examination reveals a subtle bull’s eye maculopathy pattern
Moderate maculopathy
- Moderate reduction in visual acuity
- Fundus examination reveals an obvious bull’s eye maculopathy pattern
Severe maculopathy
- Marked reduction in visual acuity
- Fundus examination reveals widespread retinal pigment epithelium atrophy
End-stage maculopathy
- Severe reduction in visual acuity
- Marked atrophy of the retinal pigment epithelium
- Unmasking of the large choroidal blood vessels
- Optic nerve atrophy
- Attenuated retinal arterioles
- Pigment clumping in the peripheral retina
The following disease share some of the clinical signs and symptoms of plaquenil-induced toxic maculopathy:
- Dry age-related macular degeneration
- Wet age-related macular degeneration
- Best’s disease
- Central cerous chorioretinopathy
- Stargartd’s disease
- Dominant cone dystrophy
- Fabry’s disease
- Amiodarone therapy
Cessation of plaquenil is the standard-of-care treatment for plaquenil-induced toxic maculopathy.
If the patient has Possible Early Toxicity:
- Cessation of plaquenil if possible or follow-up at 3 to 6 month intervals until there is further evidence to rule out toxicity
If the patient has Probable Toxicity:
- Cessation of plaquenil if possible or follow-up at 3 month intervals
If the patient has Clearly Evident Toxicity:
- Cessation of plaquenil unless the drug is needed so desperately for quality of life that severe vision loss or blindness is acceptable as an outcome
1. Abbasi O. Tewari A. Common Medications That May Be Toxic to the Retina. 11 June 2009. http://www.revophth.com/content/d/retina/c/22893/. Last accessed August 17, 2014.
2. Roque M. Chloroquine and Hydroxychloroquine Toxicity. Medscape/EMedicine. 26 Aug 2013. http://emedicine.medscape.com/article/1229016-overview. Last accessed August 17, 2014.
3. Chhablani J. Drug Induced Maculopathy: A Quick Look. EJournal of Ophthalmology. http://www.ejournalofophthalmology.com/ejo/ejo29.html. Last accessed August 17, 2014.
362.55
Toxic maculopathy of retina
92015
Refraction
92250
Fundus photography
92083
Visual field examination
92283
Color vision examination
92134
Retinal laser scan
92225
Extended ophthalmoscopy
92275
Electroretinography




 Print | Share
Print | Share