Macular pucker secondary to epiretinal membrane
ICD-10 Diagnosis Codes:
H35.371 — Puckering of macula, right eye
H35.372 — Puckering of macula, left eye
H35.373 — Puckering of macula, bilateral
Title
Macular Pucker
Category
Other Retinal Disorders
Description
Macular pucker occurs when a contracting epiretinal membrane distorts the underlying retina.
Corneal edema is a clinical sign of corneal disease. The condition is characterized by an increase in corneal thickness secondary to an abnormal accumulation of fluid. The excess fluid produces a swelling of the corneal tisssue and can result in a loss of stromal transparency that produces blurred vision or visual impairment.
Macular pucker is a clinico-anatomic description of structural damage to the retina caused by epimacular proliferation or vitreomacular traction.
- Epimacular proliferation is characterized by the formation of collagenous membranes on the surface of the retina
- As the membranes grow, they can develop contractile properties that produce traction forces on the surface of the macula
- Traction on the macula can result in traction maculopathies such as macular pucker, cellophane maculopathy, vitreomacular traction syndrome or macular hole
 |
Common Names for Epimacular Proliferation
|
The histopathological changes needed to create epiretinal membranes usually begins with a posterior vitreous detachment. In some people, it’s believed that the separation of the vitreous membrane from the retinal surface damages the retina structurally.
Structural Damage to the Eye
- Posterior vitreous detachment produces focal areas of damage on the inner retinal surface
- Immune system response to damaged areas results in inflammatory reaction on the inner retinal surface
- Glial cells from the neurosensory retina grow through breaks in the internal limiting membrane of the damaged retina
- Glial cells combine with inflammatory cells and collagen cells to form membranes
- Membranes form attachments to the inner retinal surface
- Membranes proliferate in the central retina and macula
- Membranes contract over time and create traction forces on retinal tissue
- Underlying retina becomes structurally damaged secondary to traction forces
Functional Damage to the Eye
- Traction on the macula produces decreased visual acuity based on the amount of force and its duration of action
- Vascular incompetence secondary to macular traction (especially in diabetic patients) results in progressive loss of acuity
- Diffuse macular edema usually results in decreased vision
- Foveal cysts usually results in decreased vision
- Macular detachment results in decreased vision
The main goal of the diagnostic evaluation in a patient with macular pucker is to accomplish the following:
- Evaluate epiretinal membrane density, thickness, and location in relation to the retina
- Determine the presence or absence of vascular incompetence secondary to the macular traction
- Determine the presence or absence of macular edema secondary to the traction
- Prescribe a treatment program to manage the traction maculopathy and prevent permanent vision loss
Patient History
The symptoms of traction maculopathy vary from no symptoms to severe visual impairment. Patients with early disease may report blurred vision, decreased vision, or mild visual distortion. More advanced presentations often produce metamorphopsia, micropsia, or other abnormal visual distortions of shape and size.
Patients with traction maculopathy usually present with the following range of decreased visual acuity.
- 20/25 acuity or better is present in 56-67% of patients
- 20/40 acuity or better is present in 75-85% of patients
- 20/400 acuity or worse is present in 2-5% of patients
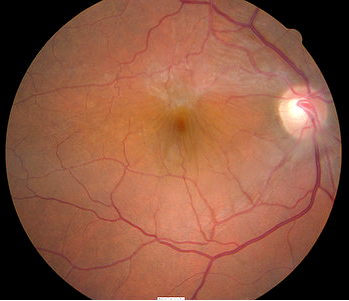
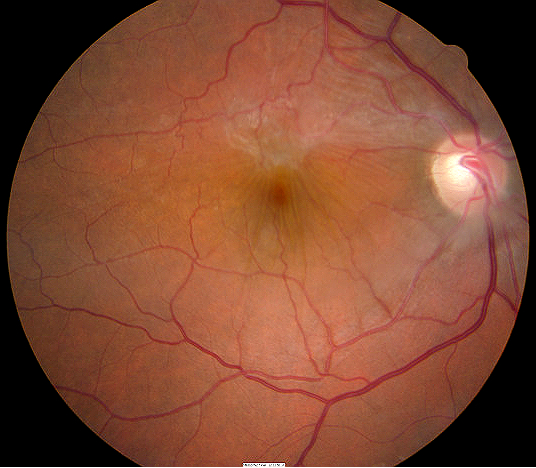
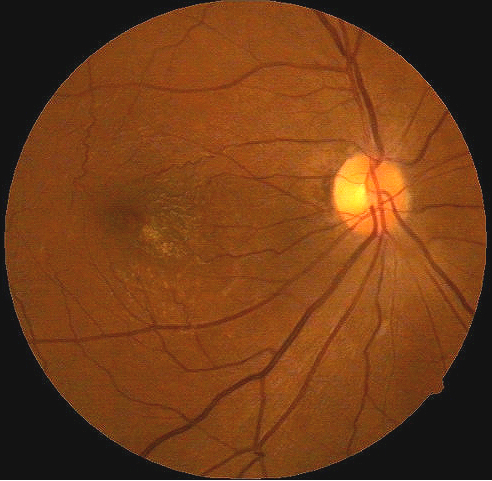
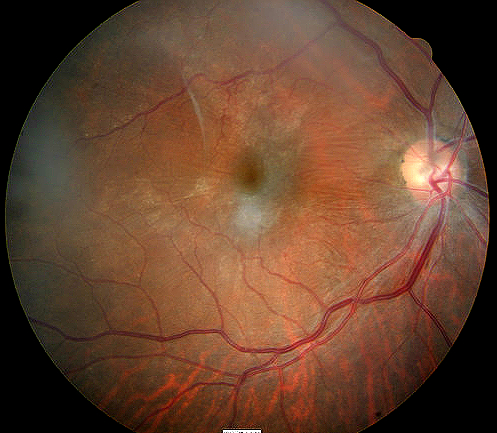
Clinical Appearance of the Retina
- A broad, glial epiretinal membrane adheres to the retinal surface and is anchored in the vascular arcades of the right eye
Macular pucker in in the right eye of a |
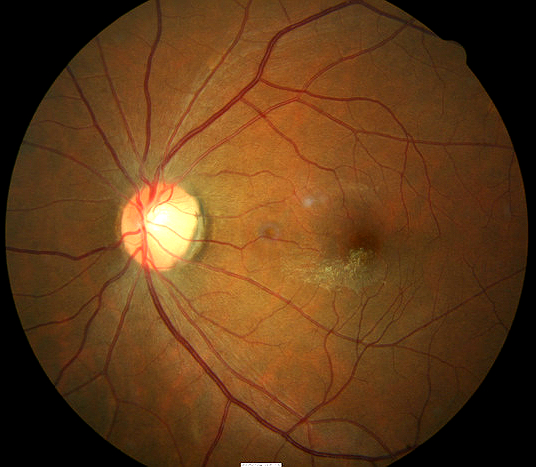
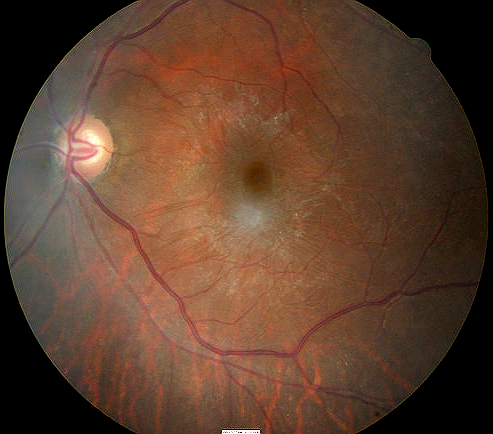
Norma macular appearance in the left eye of a |
DIAGNOSTIC TESTS
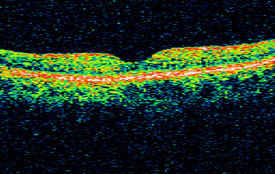
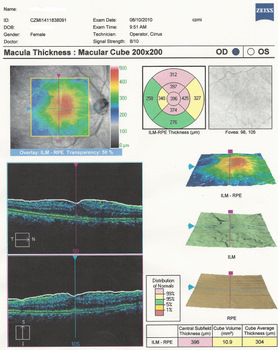
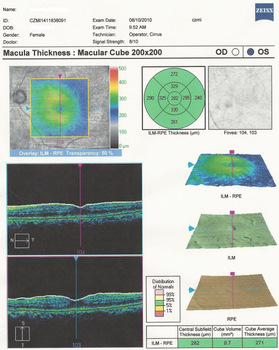
Retinal Laser Scan
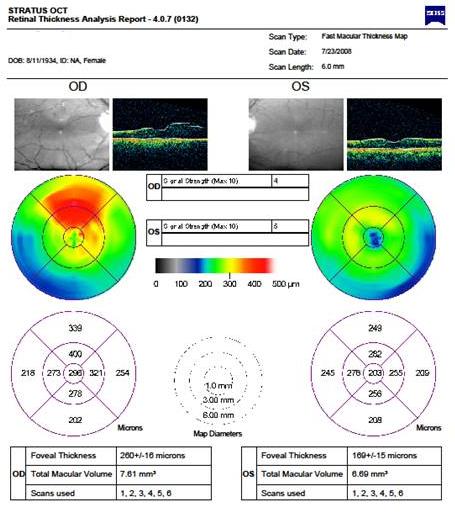 |
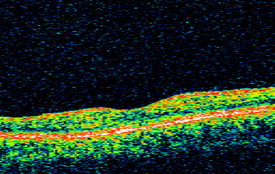
Optical Coherence Tomography
|
Classification of epiretinal membranes is based on the apperance of the membrane and the underlying retina and blood vessels.
 |
Grade 0 membranes
|
|
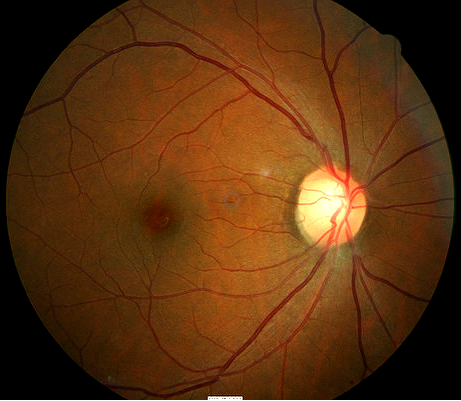
| Patient in the following images is a 42-year-old black woman
Grade 1 membranes
|
 |
|
 |
 |
|
Optical Coherence Tomography
|
 |
|
 |
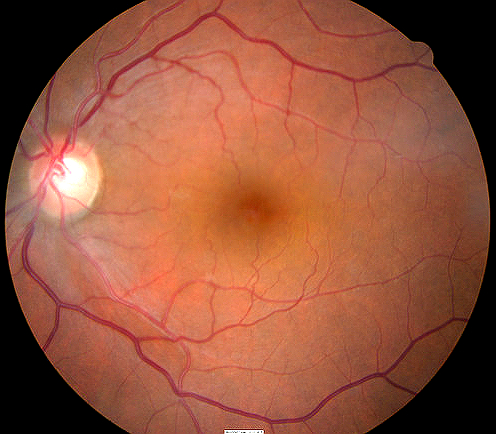
Patient in the following images is a 72-year-old black woman
Grade 2 membranes
|
|
Bilateral Presentation of Epiretinal Membrane
|
 |
|
 |
Optical Coherence Tomography
|
|
Optical Coherence Tomography
|
 |
Differential diagnoses would include other diseases that share the clinical signs of macular pucker. This would include diseases or conditions that produce abnormal vitreomacular interfaces
- Cystoid macula edema
- Posterior uveitis
- Retinal vascular occlusive disease
- Diabetic retinopathy
Palliative Treatment
- Observation in the early stages of the disease and when there is minimal traction on the macula
Pharmacologic Treatment
On January 1, 2013, the FDA approved JETREA (ocriplasmin) for the treatment of symptomatic vitreomacular adhesion. JETREA is a proteolytic enzyme delivered in a single 3.5mg/mL dose that alters the biochemistry of the vitreous to produce a pharmacologic vitreolysis.
JETREA Intravitreal Injection
- Liquefies vitreous
- Produces a separation between the vitreous cortex and the internal limiting membrane
- Resolution of vitremacular traction in 26% of treated group during Phase III clinical studies
Potential side effects include the following
- Intraocular inflammation
- Intraocular infection
- Intraocular hemorrhage
- Increased intraocular pressure
- Lens subluxation
- Floaters
- Retinal detachment
- Changes in color vision
Surgical Treatment
Pars Plana Vitrectomy with Membrane Peel
Potential side effects include the following
- Intraocular inflammation
- Intraocular infection
- Intraocular hemorrhage
- Retinal detachment
- Extended recovery period
1. Facts About Macular Pucker. National Eye Institute. Apr 2012. http://www.nei.nih.gov/health/pucker/pucker.asp. Last accessed August 17, 2014.
2. Joyce K. Gurwood A. A Look at VMT Syndrome. 15 Oct 2011. http://www.revoptom.com/content/c/30708/. Last accessed August 17, 2014.
3. Convertino J. Marcus S. Wong A. Did OCT Help Diagnose VMTS? RevOptom. 15 Jan 2007. http://www.revoptom.com/content/d/news_review/c/15537/. Last accessed August 12, 2014.
4. Vitreomacular traction syndrome. National Retina Institute. http://nationalretina.com/RetinalConditions/VitreomacularTractionSyndrome.aspx. Last accessed April 3, 2014.
5. Morris R, Witherspoon CD, Kuhn F, Nelson S, Priester B, Mayne R. Traction maculopathy. Retinology Today.
6. Vitreomacular traction. Williamson Eye Institute. http://www.williamsoneyeinstitute.com/retina-center/vitreomacular-traction. Last accessed April 3, 2014.
362.56
Macular puckering
92250
Fundus photography
92225
Extended ophthalmoscopy
92134
Macula OCT scan
92083
Visual field examination
92275
Electroretinography
92283
Color vision examination
Ocurrence
The prevalence of macular pucker is 2% of the population greater than 55-years-old.
Distribution
Macular pucker is not evenly distributed throughout the population. Its distribution increases with age.
Risk Factors
- Advancing age
- Vitreous detachment
- Retinal detachment
- Uveitis
- Diabetics with retinal complications




 Print | Share
Print | Share