
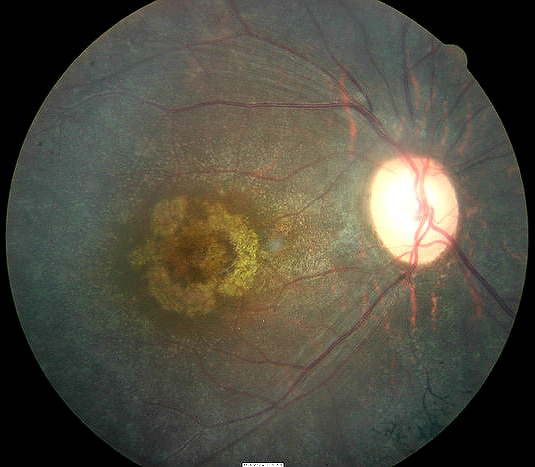
Subretinal hemorrhage in
exudative macular degeneration
ICD-10 Diagnosis Code:
H35.32–Age-related macular degeneration, exudative
Title
Exudative Senile Macular Degeneration of Retina
Category
Other Retinal Disorders
Description
Exudative senile macular degeneration or wet age-related macular degeneration is an aggressive condition that affects the macula region of the retina resulting in central vision loss.
Age-related macular degeneration describes any type of acquired maculopathy that affects people over 50-years old.
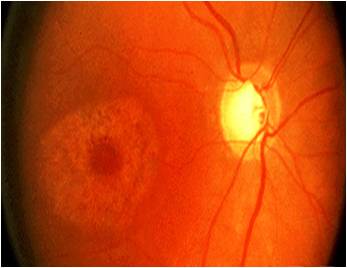
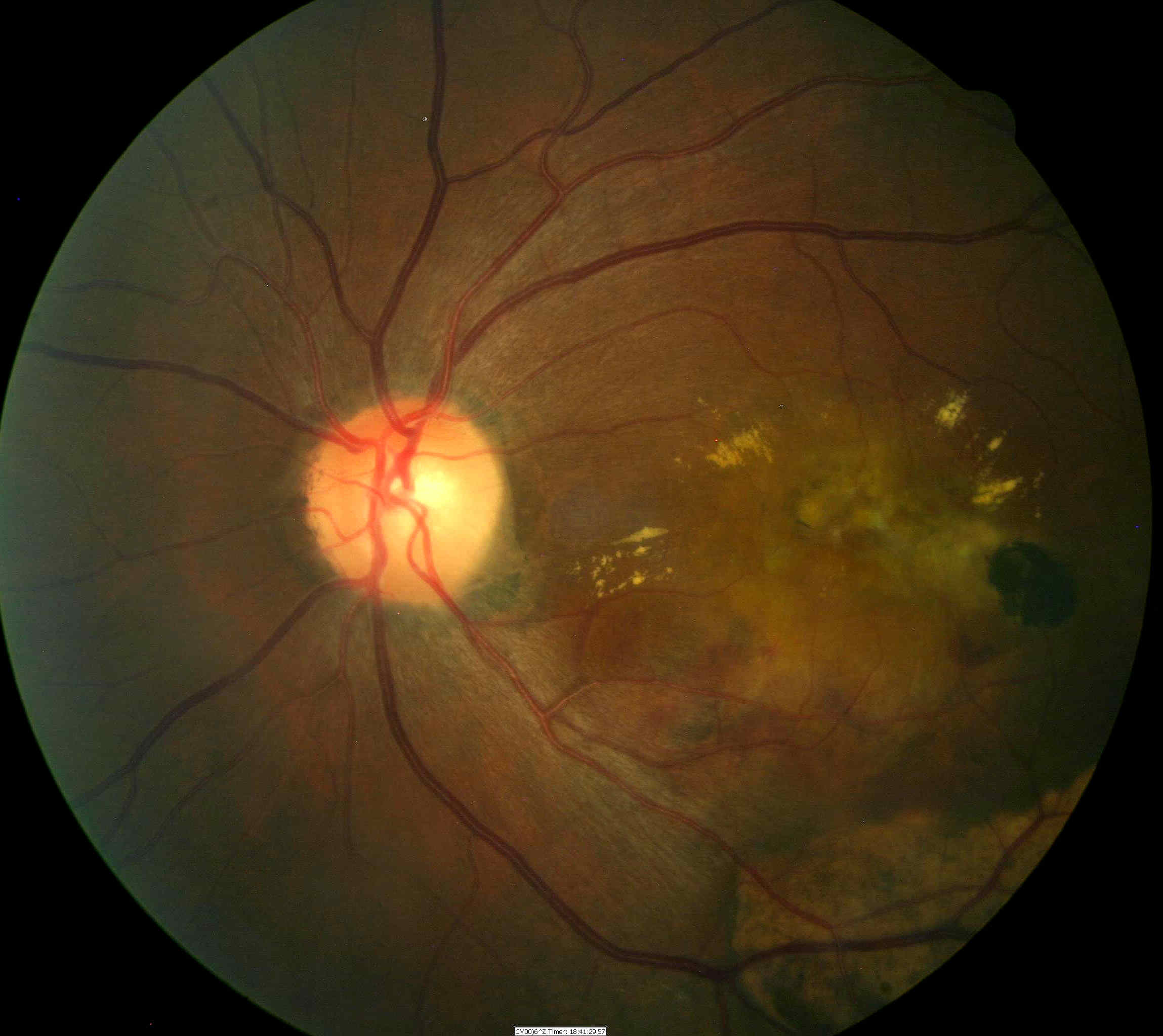
Wet Macular Degeneration: The exudative form of the disease is characterized by neovascularization under the macula. These abnormal blood vessels leak, bleed, and scar the retina, distorting or destroying central vision. Visual distortion tends to be unilateral and may progress to affect the other eye later. Vision loss may be rapid in the wet type of macular degeneration in comparison to the dry form.
Structural Damage to the Eye
- New blood vessels (e.g., neovascularization) of the macula and retina
- Retinal hemorrhages
Functional Damage to the Eye
- Sudden or gradual blurred or distorted central vision
- Patient reports difficulty seeing faces or doing normal task like reading
- Sudden or gradual decreased visual acuity
- Patients report straight lines appear crooked, wavy or distorted
- Objects appear smaller in one eye than the other
The main goal of the diagnostic evaluation in a patient with exudative macular degeneration is to accomplish the following:
- Evaluate the extent of structural changes such as exudates, edema or atrophy in the macula
- Determine the presence or absence of vascular abnormalities secondary to the macular degeneration
- Determine the presence or absence of atrophy secondary to the macular degeneration
- Prescribe a treatment program to treat the macular degeneration and slow the vision loss
Patient History
Patients present with symptoms of unilateral central vision loss which is usually gradual, but can be sudden if it is the wet form of macular degeneration. Most of the time, patients describe the vision loss as distortions of faces, lines or metamorphopsia.
| Ophthalmoscopic Examination
Ophthalmoscopy will reveal the following clinical signs:
|
 |
DIAGNOSTIC TESTS
Refraction
- Allows for the measurement of visual function and acuity
Fundus Photography
- Used to evaluate the structure of the macula and retina
- Help plan a treatment program for exudative macular degeneration
Extended Ophthalmoscopy
- Patients with miotic pupils and dense cataracts may not allow a good view of the internal structures with fundus photography
- Extended ophthalmoscopy may be an alternative to view internal structures
- Document any other associated structural changes to the macula and the retina
- Help plan a treatment program for the macular degeneration
Retinal Scanning Laser
- Document the location and extent of the macular degeneration at a structural level
- Document any other associated structural changes to the macula and the retinal
- Help plan a treatment program for the macular degeneration
Visual Field Examination
- Used to determine the extent of functional damage to vision in comparison to structural damage
The information provided by these tests are used for medical decision-making in the following manner:
- To document the progress of the macular degeneration
- To document the delivery of the medical treatment
- To document the response to treatment
Wet age-related macular degeneration is not separated into stages.
 |
Conditions that affect the Retinal Pigment Epithelium and Choriocapillaries
|
|
 |
Toxic Lesion
|
|
 |
Conditions that cause Choroidal Neovascularization
|
Other causes of subretinal hemorrhages
- Macroanerysms along the retinal arteriole
- Choroidal rupture
Other causes of subretinal fluid
- Central serous retinopathy
Laser Therapy
Exudative macular degeneration can be treated with laser surgery, however, this treatment is not a cure. The disease and loss of vision may progress despite treatment.
Laser surgery: A laser is used to destroy the fragile, leaky blood vessels. A small percentage of people with wet AMD can be treated with laser surgery. Laser surgery is more effective if the leaky blood vessels have developed away from the fovea. This procedure does destroy health tissue.
Pharmaceutical Agents
Exudative macular degeneration can be treated with photodynamic therapy and injections into the eye. These treatments are not a cure and the disease and loss of vision may progress despite treatment.
Photodynamic therapy: A drug called verteporfin (Visudyne) is administered intravenously. The drug is allowed to travel throughout the body. The drug is activated by a light and destroys the new blood vessels, which leads to a slower rate of vision decline. This drug does not destroy surrounding healthy tissue.
Injections: New drugs with anti-VEGF therapy is injected into the eye. Patients with exudative maculopathy have abnormally high levels of a specific growth factor in the eye that promotes the growth of new blood vessels. This drug treatment blocks the effects of the growth factor and can help slow down vision loss. In some cases, treatment can result in improved vision.
Newly approved and investigational drugs: There are now several newly approved and investigational drugs for macular degeneration in the United States. Most of these medications are given directly into the eye or around the eye, and include the following:
Pegaptanib (Macugen) was FDA approved in December 2004. It blocks VEGF and helps stabilize vision. Pegaptanib is beneficial in treating both classic and occult subfoveal choroidal neovascular membranes. The drug is administered by injection into the eye.
Ranibizumab (Lucentis, formerly called RhuFab) is a newly approved anti-VEGF for wet AMD by the FDA in 2006. It is administered inside the eye via the pars plana. Preliminary studies have shown improved vision in patients with many forms of wet age-related macular degeneration.
Triamcinolone acetonide is an intraocular injection of corticosteroids. It was FDA approved in November 2007 forTriesence (Alcon) and June 2008 for Trivaris (Allergan).
Bevacizumab (Avastin) is another anti-VEGF drug that is currently approved for cancer of the colon or rectum. It is being investigated for intravitreal use in the eye for the treatment of choroidal neovascularization and macular degeneration.
Squalamine lactate (Evizon) is an investigational anti-VEGF drug that is administered intravenously. This drug may have the potential in treating choroidal neovascular membrane formation.
Anecortave acetate (Retaane) is an investigational drug aimed at inhibiting the abnormal growth of blood vessels in macular degeneration. The drug is injected behind the eye rather than into the eye. Alcon discontinued investigations of this medication when statistical endpoints were not met in preliminary studies. The major difficulty was determining the exact dosage to the interior of the eye. Reformulations with better predictability promise improved results and further investigation.
Surgery
There are several investigative surgical treatments being used for exudative age-related macular degeneration lesions that may not qualify for laser treatment.
- Macular translocation to a healthier area of the eye
- Displacement of submacular blood using gas
- Removing membranes by surgery
1. Prall R. Exudative ARMD. Medscape/EMedicine. http://emedicine.medscape.com/article/1226030-overview. Last accessed August 17, 2014.
2. Olsen T. Knobloch W. Treatment of Exusdative Age-Related Macular Degeneration: Many Factors To Consider. National Library of Medicine. 1 Aug 2008. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2040182/. Last accessed August 17, 2014.
3. Fong D. Age-Related Macular Degeneration: Update For Primary Care. Am Fam Physician. 2000 May 15;61(10):3035-3042. http://www.aafp.org/afp/2000/0515/p3035.html. Last accessed August 17, 2014.
362.52
Exudative senile macular
degeneration of retina
92250
Fundus photography
92225
Extended ophthalmoscopy
92134
Macula OCT scan
92083
Visual field examination
92283
Color vision examination
92275
Electroretinography
Occurence
- The prevalence of age-related macular degeneration is almost 1.5% of the population over 40-years-old
- The prevalence increases drastically with age
- For example, 15% of caucasian women over the age of 80 will have age-related macular degeneration
Distribution
Age-related macular degeneration is not distributed evenly throughout the population.
- Women are at a greater risk than men
- Caucasians are more likely to loss vision from AMD than African Americans
Risk Factors
- Age
- Family history
- Gender
- Smoking
- Obesity
- High degree of myopia
- Lifelong exposure to sunlight
- Lighter iris color and light skin pigmentation
- Medications for osteoporosis may cause predisposition




 Print | Share
Print | Share