Full-thickness macular hole
ICD-10 Diagnosis Codes:
H35.341–Macular cyst, hole, or pseudohole, right eye
H35.342–Macular cyst, hole, or pseudohole, left eye
H35.343–Macular cyst, hole, or pseudohole, bilateral
Title
Macular Cyst Hole Or Pseudohole Of Retina
Category
Other Retinal Disorders
Description
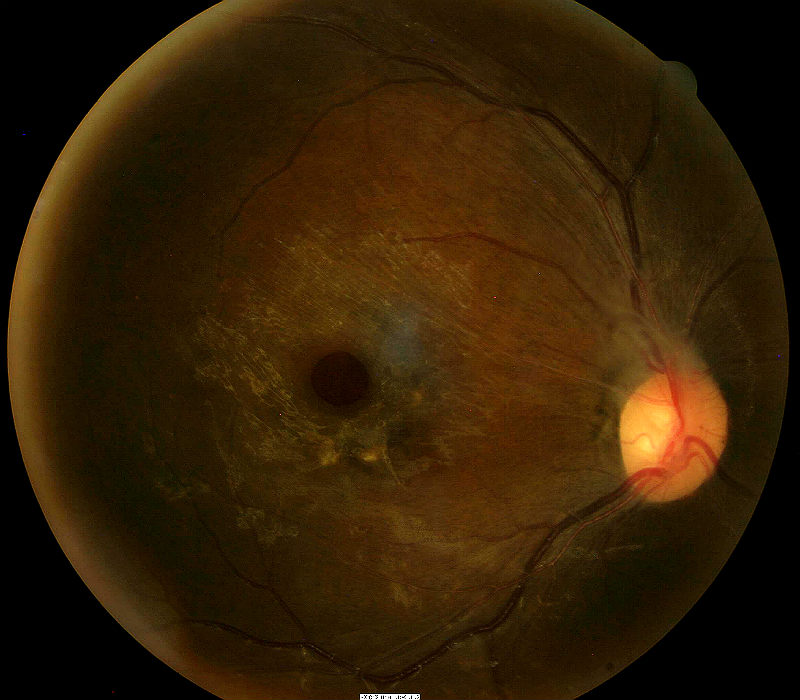
A macular hole is a defect of the foveal retina involving its full thickness from the internal limiting membrane (ILM) to the outer segment of the photoreceptor layer.
Pseudohole of retina is a clinico-anatomic description of structural damage to the retina caused by epimacularproliferation or vitreomacular traction.
- Epimacular proliferation is characterized by the formation of collagenous membranes on the surface of the retina
- As the membranes grow, they can develop contractile properties that produce traction forces on the surface of the macula
- Traction on the macula can result in traction maculopathies such as macular pucker, cellophane maculopathy, vitreomacular traction syndrome or macular hole
 |
Macular Hole Secondary to Epimacular Poliferation
|
The histopathological changes needed to create epiretinal membranes usually begins with a posterior vitreous detachment. In some people, it’s believed that the separation of the vitreous membrane from the retinal surface damages the retina structurally.
Structural Damage to the Eye
- Posterior vitreous detachment produces focal areas of damage on the inner retinal surface
- Immune system response to damaged areas results in inflammatory reaction on the inner retinal surface
- Glial cells from the neurosensory retina grow through breaks in the internal limiting membrane of the damaged retina
- Glial cells combine with inflammatory cells and collagen cells to form membranes
- Membranes form attachments to the inner retinal surface
- Membranes proliferate in the central retina and macula
- Membranes contract over time and create traction forces on retinal tissue
- Underlying retina becomes structurally damaged secondary to traction forces
Functional Damage to the Eye
- Traction on the macula produces decreased visual acuity based on the amount of force and its duration of action
- Vascular incompetence secondary to macular traction (especially in diabetic patients) results in progressive loss of acuity
- Diffuse macular edema usually results in decreased vision
- Foveal cysts usually results in decreased vision
- Macular detachment results in decreased vision
The main goal of the diagnostic evaluation in a patient with a macular cyst or macular hole is to accomplish the following:
- Evaluate epiretinal membrane density, thickness, and location in relation to the retina
- Determine the presence or absence of vascular incompetence secondary to the macular traction
- Determine the presence or absence of macular edema secondary to the traction
- Prescribe a treatment program to manage the traction maculopathy and prevent permanent vision loss
Patient History
The symptoms of a macular cyst or hole vary from no symptoms to severe visual impairment. Patients with early disease may report blurred vision, decreased vision, or mild visual distortion. More advanced presentations often produce metamorphopsia, micropsia, or other abnormal visual distortions of shape and size.
Patients with traction maculopathy usually present with the following range of decreased visual acuity.
- 20/25 acuity or better is present in 56-67% of patients
- 20/40 acuity or better is present in 75-85% of patients
- 20/400 acuity or worse is present in 2-5% of patients
Ophthalmoscopic Examination
Ophthalmoscopy will reveal the following clinical signs:
- Drusen
- Macular edema
- Subretinal fluid
- Retinal pigment epithelial clumping and/or loss
- Subretinal fibrosis (disciform scarring)
- Neovascularization and subretinal hemorrhage
DIAGNOSTIC TESTS
Refraction
- Allows for the measurement of visual function and acuity
Fundus Photography
- Used to evaluate the structure of the macula and retina
- Help plan a treatment program
Extended Ophthalmoscopy
- Patients with miotic pupils and dense cataracts may not allow a good view of the internal structures with fundus photography
- Extended ophthalmoscopy may be an alternative to view internal structures
- Document any other associated structural changes to the macula and the retina
- Help plan a treatment program
Retinal Scanning Laser
- Document the location and extent of the macular degeneration at a structural level
- Document any other associated structural changes to the macula and the retinal
- Help plan a treatment program
Visual Field Examination
- Used to determine the extent of functional damage to vision in comparison to structural damage
The information provided by these tests are used for medical decision-making in the following manner:
- To document the progress of the macular cyst or hole
- To document the delivery of the medical treatment
- To document the response to treatment
Johnson and Gass, in 1988, first described a classification system that focused on anteroposterior and tangential vitreous traction on the fovea as a primary underlying cause for idiopathic macular holes. Shrinkage of prefoveal cortical vitreous with persistent adherence of vitreous to the foveal region results in the causative traction.
Macular holes can be classified into their stages of development:
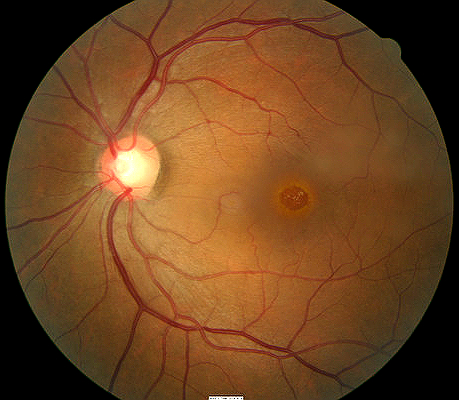
Stage 1a (foveal detachment; macular cyst): Tangential vitreous traction results in the elevation of the fovea marked by increased clinical prominence of xanthophyll pigment. This stage is occasionally referred to as the yellow dot stage and can also be seen in cases of central serous chorioretinopathy, cystoid macular edema, and solar retinopathy as depicted below.
Stage 1b: As the foveal retina elevates to the level of the perifoveal, the yellow dot of xanthophyll pigment changes to a donut shaped yellow ring. Persistent traction on the fovea leads to dehiscence of deeper retinal layers at the umbo.
Stage 2: This is the first stage when a full-thickness break in the retina exists. It is defined as a full-thickness macular hole less than 400 µm in size. The full-thickness defect may appear eccentric, and there may be a pseudo-operculum at this stage if there has been spontaneous vitreofoveolar separation. These opercula have been examined and found to be vitreous condensation and glial proliferation without harboring any retinal tissue.
Stage 3: A full-thickness macular hole in the retina exists. It is greater than 400 µm in size and is still with partial vitreomacular adhesion/traction.
Stage 4: A full-thickness macular hole exists in the presence of a complete separation of the vitreous from the macula and the optic disc. There is evidence, however, that, even in the presence of an apparent posterior vitreous detachment, a thin shell of residual cortical vitreous may still remain and contribute to the macular hole.
Differential diagnoses would include other diseases that share the clinical signs of macular pucker. This would include diseases or conditions that produce abnormal vitreomacular interfaces:
- Cystoid macula edema
- Posterior uveitis
- Retinal vascular occlusive disease
- Epimacular membrane
On January 1, 2013, the FDA approved JETREA (ocriplasmin) for the treatment of symptomatic vitreomacular adhesion. JETREA is a proteolytic enzyme delivered in a single 3.5mg/mL dose that alters the biochemistry of the vitreous to produce a pharmacologic vitreolysis.
Palliative Treatment
- Observation in the early stages of the disease and there is minimal pulling-effect upon the macula
Pharmacologic Treatment
On January 1, 2013, the FDA approved JETREA (ocriplasmin) for the treatment of symptomatic vitreomacular adhesion. JETREA is a proteolytic enzyme delivered in a single 3.5mg/mL dose that alters the biochemistry of the vitreous to produce a pharmacologic vitreolysis.
JETREA Intravitreal Injection
- Liquefies vitreous
- Produces a separation between the vitreous cortex and the internal limiting membrane
- Resolution of vitremacular traction in 26% of treated group during Phase III clinical studies
Potential side effects include the following:
- Intraocular inflammation
- Intraocular infection
- Intraocular hemorrhage
- Increased intraocular pressure
- Lens subluxation
- Floaters
- Retinal detachment
- Changes in color vision
Surgical Treatment
Pars Plana Vitrectomy with Membrane Peel
Potential side effects include the following:
- Intraocular inflammation
- Intraocular infection
- Intraocular hemorrhage
- Retinal detachment
- Extended recovery period
1. Theng K. Macular Hole. Medscape/EMedicine. 16 April 2014. http://emedicine.medscape.com/article/1224320-overview#showall. Last accessed January 18, 2015.
2. Convertino J. Marcus S. Wong A. Did OCT Help Diagnose VMTS? RevOptom. 15 Jan 2007. http://www.revoptom.com/content/d/news_review/c/15537/. Last accessed August 12, 2014.
3. Girach A. Pakola S. Vitreomacular Interface Diseases. Expert Rev Ophthalmol. 2012;7(4):311-323. http://www.medscape.com/viewarticle/772188. Last accessed January 20, 2015.
362.54
Macular cyst hole or
pseudohole of retina
92250
Fundus photography
92225
Extended ophthalmoscopy
92134
Macula OCT scan
92083
Visual field examination
92275
Electroretinography
92283
Color vision examination
Vitreomacular traction syndrome




 Print | Share
Print | Share