ICD-10 Diagnosis Code:
H18.59–Other hereditary corneal dystrophy
Title
Anterior Corneal Dystrophies
Category
Corneal Opacity And Other Disorders Of Cornea
Description
Epithelial basement membrane dystrophy (EBMD) is a degenerative condition of the anterior layer of the cornea.
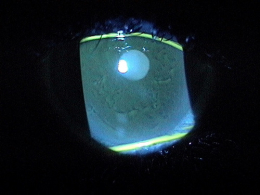
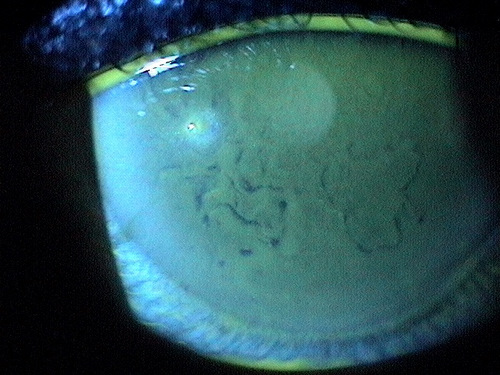
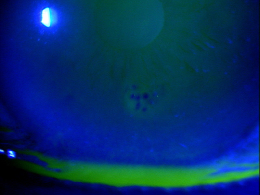
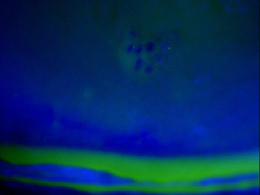
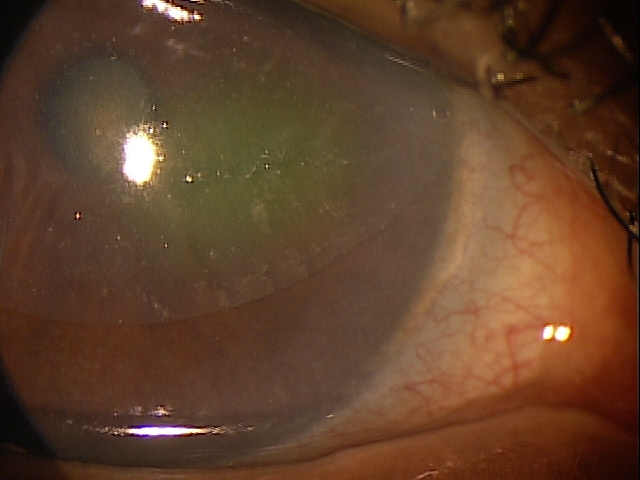
Epithelial basement membrane dystrophy (EBMD) is characterized by abnormal quantities of basement membrane and cytoplasmic debris that are misdirected into the corneal epithelium. Clinically, the abnormal deposits in EBMD appear as dot-like opacities, map-like patterns, or whorled fingerprint-like lines in the corneal epithelium. In many patients, the epithelial lesions change in appearance, location and number over time.
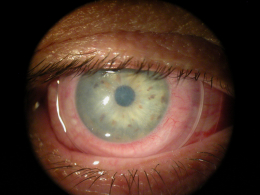
- Normal appearance under low magnification
- Corneal opacities in EBMD under high magnification
The anterior layer of the cornea is composed of the corneal epithelium and its underlying basement membrane. The basal cells of the corneal epithelium produce and adhere to the basement membrane via hemidesmosomes and basement membrane complexes.
Structural Damage to the Eye
In most patients, the disease causes no significant structural deficit to the cornea, no symptoms and no functional vision problems. In patients with clinically significant EBMD, the abnormal deposits of basement membrane can result in the loss of hemidesmosomes between Bowman’s layer and the basal epithelial cells. Over time, the loss of hemidesmosomes can lead to the following:
- Intermittent epithelial breakdown
- Irregular astigmatism
- Recurrent corneal erosions
Functional Damage to the Eye
- Decreased vision may result if any structural damage occurs in the axial region of the cornea
The main goal of the diagnostic evaluation in a patient with EBMD is to accomplish the following:
- Determine the presence of epithelial basement membrane dystrophy
- Releive ocular pain and discomfort
- Imrove visual acuity if applicable
- Prescribe a treatment program to treat the condition and prevent future complications
Patient History
Patient symptoms vary depending on the severity of the disease and mild conditions may produce no symptoms. Patients with EBMD may present with any of the following abnormal clinical signs and symptoms:
- Mild blurred vision
- Variable and fluctuating vision
- Ghosting or monocular diplopia
- Visual distortion
- Glare
- Photophobia
- Dry eye / Foreign body sensations
- Unstable refractions
- Recurrent corneal erosion (one of the worst complications of EBMD)
External Ocular Examination with Biomicroscopy
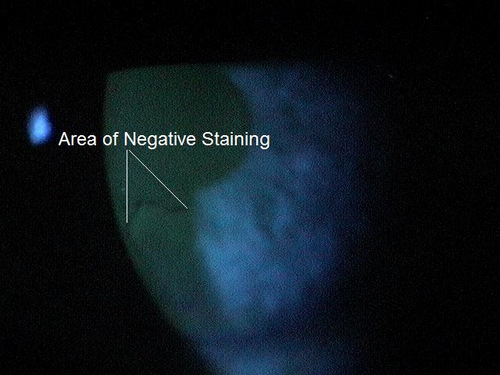
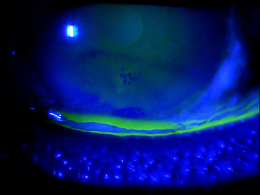
The abnormal basement membrane migrates into the corneal epithelium and produces focal areas of elevation. The elevated edges of the lesions have a scalloped shape and can produce tear film abnormalities that are visible with fluorescein and a cobalt blue light.
- The maps are irregulary shaped gray-white patches that may contain circular areas
- They vary in size from one millimeter to several millimeters in diameter and are best visualized with broad oblique slit-lamp illumination
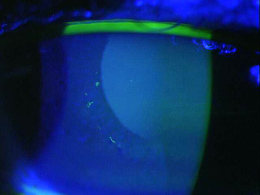
- The dots are gray-white opacities which can be round, comma-shaped or irregularly shaped
- They vary in size from 0.05 millimeter to 1 millimeter in size
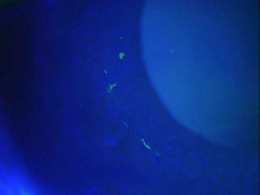
- The fingerprints are cluster of contoured concentric lines
- They vary in length from 0.25 millimeters to 4 millimeters
- Fingerprints are best visualized with retroillumination.
- Corneal blebs are a less common manifestation of map-dot-fingerprint dystrophy. They are localized areas of fibrillogranular material or thickened basement membrane and vary in size from 0.05 millimeters to 0.2 millimeters in diameter. Blebs are best visualized with retroillumination.
- In cases of active epithelial erosion, positive staining marks areas of epithlial breakdown. These patients will be the most symptomatic, often presenting with classic RCE morning symptoms.
In the vast majority of patients, EBMD is thought to be a degenerative disorder rather than a corneal dystrophy.
A small number of patients with EBMD have a true corneal dystrophy with a genetic inheritance pattern. According to the International Committee for Classification of Corneal Dystrophies (IC3D), epithelial basement membrane dystrophy is a Categoy 1 Corneal Dystrophy. In this type of dystrophy, the gene has been identified and mapped and specific mutations are known.
Differential diagnoses would include any diseases that present with corneal opacities or epithelial damage.
- Corneal abrasion
- Fuchs’ endothelial dystrophy
- Herpes simplex
- Herpes zoster
The first goal of treating patients with EBMD is to reduce complications.
Preventative Treatment
- Avoiding or minimizing contact lens wear in patients with preexisting epithelial disease
Pharmocologic Treatment
Hyperosmotics
- The goal of treatment is to improve visual acuity by deturgescence of the stroma or epithelium. Compliance with topical hyperosmotic solutions can be challenging due to the burning sensations they often produce. Nighttime application of hyperosmotic ointment is an excellent if not preferred treatment.
Artificial Tears (FreshKote Ophthalmic Solution)
- The goal of treatment is to remove excess water from the epithelium by utilizing the high oncotic pressure of the solution
Mechanical Treatment
- Bandage contact lenses – in patients with EBMD, overnight wear of soft contact lens can be used to decrease pain and improve visual acuity
Surgical Treatment
- Amniotic membrane placement
- Debridement/superficial keratectomy
- Debride the cornea with a blunt Kimura spatula
- Smoothing the basement membrane with a diamond burr
- Excimer laser phototherapeutic keratectomy
Amniotic Membrane Inserts
It should be noted that the underlying pathophysiology of EBMD lies in the basement membrance. Simple debridement of the epithelium does little to solve this problem, more likely just resetting the clock for future epithelial breakdown. Polishing the basement membrane with a diamond burr or photoablative removal of the defective basement membrane will produce far more effective and longer lasting benefits.
1. Bowling E. Russell GE. Shovlin JP. Sindt CW. Epithelial basement membrane dystrophy. RevOptom: The Cornea Atlas: 14.
371.52
Other anterior corneal dystrophies
92285
External ocular photography
92025
Corneal topography
92071
Bandage contact lens
68761
Punctal occlusion
65778
Amniotic membrane placement
Occurence
The prevalence of EBMD ranges from 2% – 4% of the population.
Distribution
EBMD is slightly more common in women.
Risk Factors
- Advancing age
- Previous ocular injury
- Previous ocular surgery
- Dry eye syndrome
- Corneal edema
- Chronic eye disease




 Print | Share
Print | Share