ICD-10 Diagnosis Codes:
H52.211–Irregular astigmatism, right eye
H52.212–Irregular astigmatism, left eye
H52.213–Irregular astigmatism, bilateral
Title
Irregular Astigmatism
Category
Disorder Of Refraction
Description
A refractive state in which refraction in different meridians conforms to no geometrical plan.
Irregular astigmatism is the clinico-anatomic description for a deviation along the refractive light path. It is usually due to surface corneal astigmatism but some forms of irregular astigmatismhave a lenticular source.
Irregular Surface Corneal Astigmatism
|
 |
Low levels of primary idiopathic irregular astigmatism are common in the general population. In patients with a toric refractive error, approximately 40% of normal corneas have some degree of primary idiopathic irregular astigmatism.
Primary idiopathic irregular astigmatism can also be noncorneal. This condition, known as ocular residual astigmatism, is caused by internal refractive surface irregularity or media irregularity. The most common cause is lenticular astigmatism which produces irregular astigmatism of the entire refractive light pathway.
Secondary irregular astigmatism is the result of some type of initiating insult to the cornea or crystalline lens.
Structural Damage to the Eye
Secondary irregular astigmatism can be caused by any of the following:
- Corneal surgery
- Corneal degenerations
- Corneal dystrophies
- Corneal infections
- Trauma
Functional Damage to the Eye
- Decreased vision
The main goal of the diagnostic evaluation in a patient with irregular astigmatism is to accomplish the following:
- To establish the diagnosis of irregular astigmatism
- To determine WHY there is an irregularity of the cornea
- To establish appropriate therapy
- To prevent complications
- To educate patients and involve them in managing it
To obtain the information required to determine a clinical diagnosis of irregular astigmatism and to prescribe a treatment plan, the following service components of a medical eye examination should be performed:
- Patient history
- General medical observation
- Adnexal examination
- External ocular examination with biomicroscopy
Patient History
Patients with irregular astigmatism may present with any of the following abnormal clinical signs and/or symptoms:
- Blurred vision
- Fluctuating vision
- Scarring of the cornea
- Corneal thinning
External Ocular Examination with Biomicroscopy
Patients with irregular astigmatism may present with abnormal clinical signs in any of the following anatomical areas:
- Trauma
- Chalazion
- Pterygium
- Limbal/corneal distrophies
- Keratorefractive surgeries
- Contact lens warpage/overwear
Irregular Astigmatism is classified into two different groups:
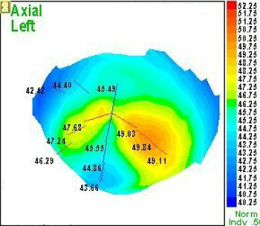
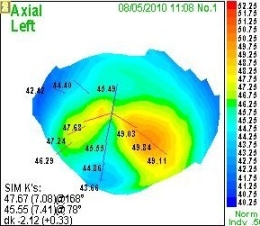
- Irregular astigmatism with defined pattern (Macroirregular, or regularly irregular astigmatism): There is a steep or flat area of at least 2 mm of diameter, which is the primary cause of the astigmatism.
- Irregular astigmatism with undefined pattern (Microirregular, or irregularly irregular astigmatism): Multiple irregularities; big and small, steep and flat, and profile maps are almost impossible to calculate.
Irregular astigmatism can be differentiated based on its source:
- Corneal surface irregular astigmatism
- Lenticular irregular astigmatism
Corrective Lenses
Rigid gas permeable contact lenses
Irregular astigmatism correction with RGP lenses allows for significant improvement in visual acuity as compared with standard spectacles correction. For this reason, RGP contact lens management is the first option in some corneal pathologies with irregular cornea, such as keratoconus. However, other pathologies, such as Herpex keratitis and other conditions, may produce irregular astigmatisms or irregular cornea. Cases are observed after surgical procedures (corneal keratoplastia, corneal refractive surgery complications and others) and corneal trauma.
Refractive Surgery
Photorecractive keratectomy (PRK)
The outer layer of the cornea, or epithelium, is a soft, rapidly regrowing layer in contact with the tear film that can completely replace itself from limbal stem cells within a few days with no loss of clarity. The deeper layers of the cornea, as opposed to the outer epithelium, are laid down early in life and have very limited regenerative capacity. The deeper layers, if reshaped by a laser or cut by a microtome, will remain that way permanently with only limited healing or remodelling. With PRK, the corneal epithelium is removed and discarded, allowing the cells to regenerate after the surgery. The procedure is distinct from LASIK (Laser-Assisted in-Situ Keratomileusis), a form of laser eye surgery where a permanent flap is created in the deeper layers of the cornea.
There are three types of PRK:
- Traditional PRK — Uses Amoils Brush or a ‘Hockey Stick’ to remove the corneal epithelium before excimer laser ablation.
- Alcohol assisted PRK — Uses alcohol to loosen the corneal epithelium before its removal. This allows gentler surgery as it avoids the need for scrubbing or scraping to remove the corneal epithelium. This originated from LASEK, and essentially is LASEK but with removal of the corneal epithelial layer at the end of surgery.
- Transepithelial PRK — Uses an excimer laser to remove the corneal epithelium. A one step, no touch technique is used where the excimer laser performs both epithelial removal and corneal reshaping sequentially. This procedure has been shown to result in less pain and faster healing of the corneal surface than alcohol assisted PRK.
Laser-Assisted in situ Keratomileusis (LASIK)
Commonly referred to as laser eye surgery or laser vision correction, is a type of refractive surgery for the correction of myopia, hypermetropia, and astigmatism. The LASIK surgery is performed by an ophthalmologist who uses a laser or microkeratome to reshape the eye’s cornea in order to improve visual acuity.
PRK Versus LASIK
PRK does not create a permanent flap in the deeper corneal layers, while LASIK involves a mechanical microtome using a metal blade or a femtosecond laser microtome to create a ‘flap’ out of the outer cornea. As such, the cornea’s structural integrity is less altered by PRK. The LASIK process covers the laser treated area with the flap of tissue which is from 100 to 180 micrometres thick. This flap can mute the nuances of the laser ablation, whereas PRK performs the laser ablation at the outer surface of the cornea. The use of the anti-metabolite mitomycin, which is referred as M-LASEK, can minimize the risk of post-operative haze in persons requiring larger PRK corrections, although the medication can worsen the dry eye that occurs after surgery in some patients. Unlike LASIK, PRK does not involve a knife, microtome, or cutting laser, but there may be more pain and slower visual recovery. Unlike LASIK, PRK does not have an increased risk of dislocated corneal flap, which may occur with trauma after LASIK.
Laser-Assisted Sub-Epithelial Keratectomy (LASEK)
Although PRK and LASEK use basically the same technique, there are minor differences between them. In PRK, epithelium is removed and the outermost layer below the epithelium is treated with laser. In LASEK, epithelium is not removed, but an alcoholic solution is used to cause the epithelial cells to weaken; the surgeon will fold the epithelial layer out of the laser treatment field, and fold it back in its original place after the cornea has been reshaped by the laser. If the epithelial flap is not strong enough to be laid back in its original place, it will be removed, and the LASEK procedure becomes a PRK procedure. Recent studies show that removing the epithelial flap results in less pain and faster epithelial recovery after LASEK. As a result, although alcohol is used to loosen the epithelium, surgeons are routinely discarding the epithelium, thus converting LASEK into alcohol assisted PRK surgery.
1. Hardten D. A Rational Approach to Irregular Astigmatism. Review of Ophthalmology. 9 Sept 2011. http://www.revophth.com/content/d/refractive_surgery/c/29984/. Last accessed August 10, 2014.
2. Wang M. Irregular Astigmatism. Wang Vision Institute. 12 Nov 2007. http://www.wangvisioninstitute.com/forms/drWang_Irregular_astigmatism.pdf. Last accessed November 16, 2014.
367.22
Irregular astigmatism
92025
Corneal topography
76514
Corneal pachymetry




 Print | Share
Print | Share