ICD-10 Diagnosis Code:
H18.59–Posterior polymorphous dystrophy
Title
Posterior Polymorphous Dystrophy
Category
Corneal Opacity And Other Disorders Of Cornea
Description
A form of corneal dystrophy characterized by a metaplasia of endothelial cells.
Posterior polymorphous dystrophy is an uncommon corneal endothelial dystrophy that is typically congenital. However, it can also be recessive and have a later onset. It usually occurs bilaterally, but often asymmetrically.
Posterior polymorphous dystrophy in most cases is inherited as a autosomal dominant, bilateral and asymmetric disease. In this condition, the corneal endothelium is often multilayered and has several other characteristics of the corneal epithelium:
- Multilaminal pattern
- Desmosomal junctions
- Microvillus projections
- Cynplasmic keratin
- Sparse Mitochonoria
- Rapid growth in tissue culture
Structural Damage to the Eye
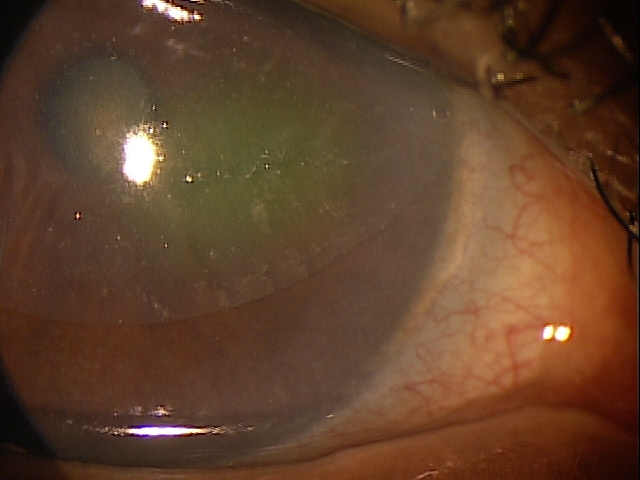
Endothelial Metaplasia
- Band-like lesions at the level of Descemet’s membrane
- Posterior corneal vesicular lesions
- Islands of abnormal endothelial cells surrounded by normal-appearing cells
Iridocorneal Adhesions
- Fine, broad-based adhesions seen only on gonioscopy
- Large adhesions associated with a glass-like membrane seen on biomicroscopy
Functional Damage to the Eye
- None (asymptomatic)
- Photophobia
- Decreased vision
The main goal of the diagnostic evaluation in a patient with posterior polymorphous dystrophy is to accomplish the following:
- Make correct diagnosis
- Rule out secondary glaucoma
- Rule out corneal edema
- Prescribe a treatment program
Patient History
The severity of the symptoms depends upon the intensity of the presentation. In severe cases, ocular pain associated with epithelial edema may be present.
- None
- Sensitivity to light
- Fluctuation vision
- Decreased vision
- Foreign body sensation
- Eye pain
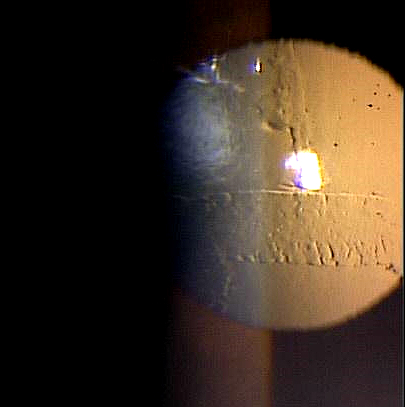
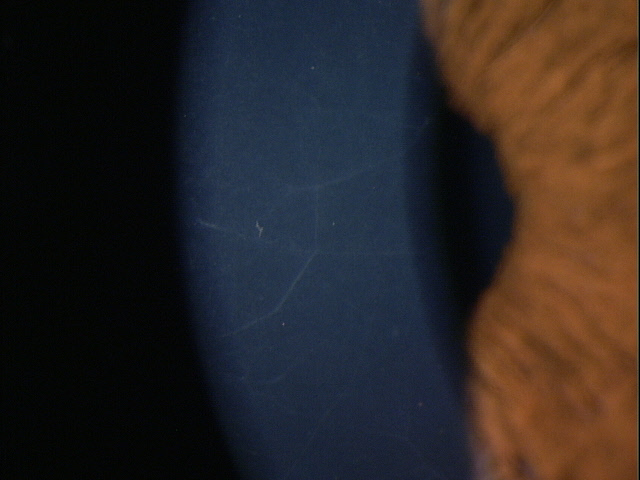
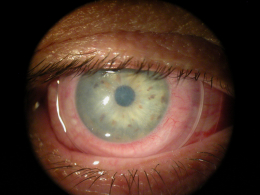
Clinical Appearance of the Cornea
DIAGNOSTIC TESTS
External Ocular Photography
- To document the progress or lack of progress of posterior polymorphous dystrophy
- To document the delivery of treatment of posterior polymorphous dystrophy
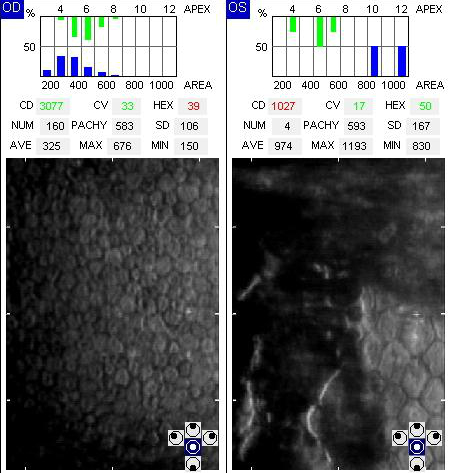
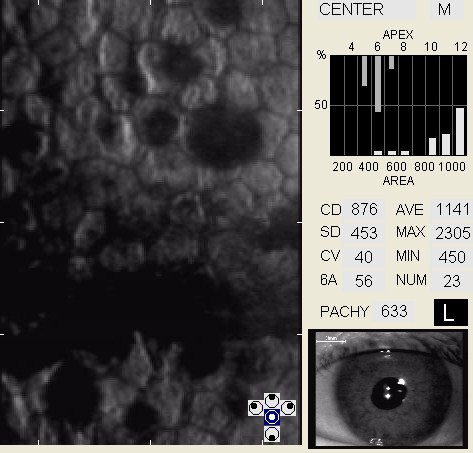
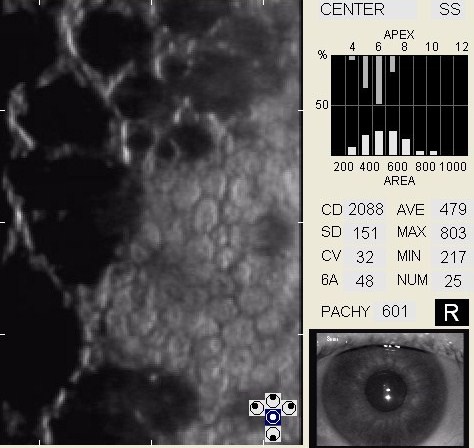
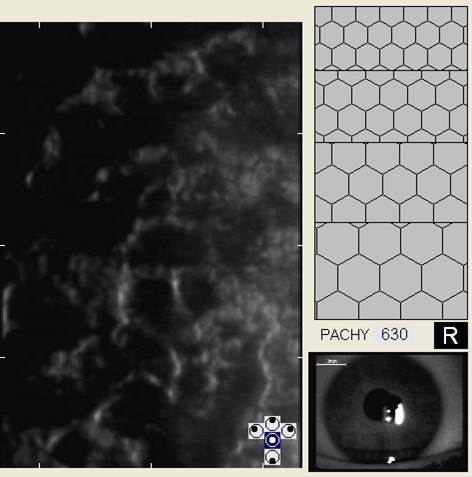
Specular Endothelial Microscopy
- To document the progress or lack of progress of corneal edema
- To document the delivery and response to medical treatment
- To help plan a treatment program
- To document the progress or lack of progress of a corneal endotheliopathy
- To visualize and analyze the corneal endothelium
Corneal Topopgraphy
- Document the shape and physical features of the anterior corneal surface
- Identification and follow-up for corneal disease causing irregular astigmatism
- To help plan a treatment program
- To document the progress or lack of progress of keratoconus
- To document the delivery of medical treatment
- To document the response to treatment
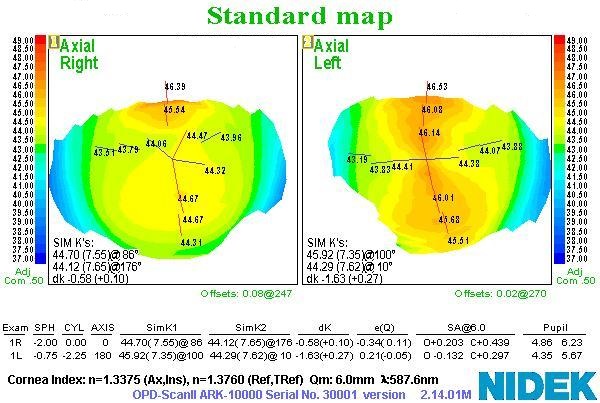 |
Surface Corneal Astigmatism
|
There is no classification system for posterior polymorphous dystrophy.
The first goal of treating patients with posterior polymorphous dystrophy is to reduce complications.
Preventative Treatment
- Avoiding or minimizing contact lens wear in patients with preexisting epithelial disease
Pharmocologic Treatment
Hyperosmotics
- The goal of treatment is to improve visual acuity by deturgescence of the stroma or epithelium. Compliance with topical hyperosmotic solutions can be challenging due to the burning sensations they often produce. Nighttime application of hyperosmotic ointment is an excellent if not preferred treatment.
Artificial Tears (FreshKote Ophthalmic Solution)
- The goal of treatment is to remove excess water from the epithelium by utilizing the high oncotic pressure of the solution
Mechanical Treatment
- Bandage contact lenses — in patients with posterior polymorphous dystrophy, overnight wear of soft contact lens can be used to decrease pain and improve visual acuity
Surgical Treatment
- Amniotic membrane allograft
- Debridement/superficial keratectomy
- Debride the cornea with a blunt Kimura spatula
- Smoothing the basement membrane with a diamond burr
- Excimer laser phototherapeutic keratectomy
Amniotic Membrane Inserts
It should be noted that the underlying pathophysiology of EBMD lies in the basement membrane. Simple debridement of the epithelium does little to solve this problem, more likely just resetting the clock for future epithelial breakdown. Polishing the basement membrane with a diamond burr or photoablative removal of the defective basement membrane will produce far more effective and longer lasting benefits.
1. Medscape. Posterior Polymorphous Corneal Dystrophy. Available at http://emedicine.medscape.com/article/1197057-overview. Accessed March 24, 2014.
2. Mejia LF, Aristizabal D, Palacio JM, Callie NL. Posterior polymorphous dystrophy and keratoconus: more than a casual association? J Emmetropia 2011; 2: 115-119.
3. Dohm K. Differential Diagnosis Key To Managing Posterior Polymorphous Dystrophy. Primary Care Optometry News. 2014 July; 19(7): 18. http://www.healio.com/optometry/retina-vitreous/news/print/primary-care-optometry-news/%7Bff8f8ff7-715b-4452-a9f3-7bce34c472fc%7D/differential-diagnosis-key-to-managing-posterior-polymorphous-dystrophy. Last accessed August 9, 2014.
371.58
Other posterior corneal dystrophies
92225
External ocular photography
92226
Specular endothelial microscopy
76514
Corneal pachymetry
92132
Anterior segment imaging
92020
Gonioscopy
92071
Bandage contact lens
65778
Amniotic membrane placement
Occurrence
- Age of onset is difficult to determine
- Some patients may present at birth with congenital disease, exhibiting advanced disease with corneal edema
- Presentation in adulthood is indicative of a more stable disease state with a decreased probability of progression to corneal decompensation
- Most patients with significant symptoms present at age 25-50 years
Distribution
- Prevalence in the general population is unknown
Risk Factors
- Keratoconus
- Alport syndrome
- Family history




 Print | Share
Print | Share