ICD-10 Diagnosis Codes:
H16.431–Localized vascularization of cornea, right eye
H16.432–Localized vascularization of cornea, left eye
H16.433–Localized vascularization of cornea, bilateral
H16.441–Deep vascularization of cornea, right eye
H16.442–Deep vascularization of cornea, left eye
H16.443–Deep vascularization of cornea, bilateral
Title
Localized Vascularization of Cornea
Category
Keratitis
Description
Corneal neovascularization is the growth of new blood vessels into the cornea.
Corneal neovascularization is a known complication of wearing contact lenses and both superficial and deep corneal neovascularization are reported with the use of hydrogel, PMMA, and rigid gas-permeable contact lenses.
The following clinical circumstances are also associated with the development of corneal neovascularization:
- Ocular injury
- Chemical burn to the eye
- Corneal degenerations
- Uveitis
- Glaucoma
- Total retinal detachment
- Pthisis bulbi
The histopathological changes needed to produce corneal neovascularization begin when epithelial trauma or chronic hypoxia causes stimulation of angiogenic factors by local epithelial cells, keratocytes and infiltrating leukocytes.
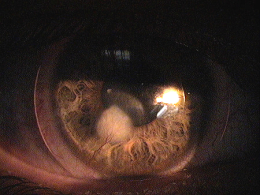
Contact Lens-Induced Corneal Neovascularization
These angiogenic factors stimulate a localized degradation of the basement membrane of the peri-limbal blood vessels as they abut the cornea. At the the apex of the vascular loop, the vascular endothelial cells start to migrate and proliferate to form new blood vessels that proliferate into the cornea.
 |
Structural Damage to the Eye
|
|
Functional Damage to the Eye
|
 |
The main goal of the diagnostic evaluation is a patient with corneal neovascularization is to accomplish the following:
- Determine the underlying etiology of the corneal neovascularization
- Classify the disease
- Prescribe a treatment program to eliminate or reduce to neovascularization
- Prescribe a treatment program to prevent future occurrences
Patient History
Patients with corneal neovascularization may present with any of the following clinical signs and symptoms:
- None
- Chronic eye redness
- Contact lens intolerance
- Decreased vision
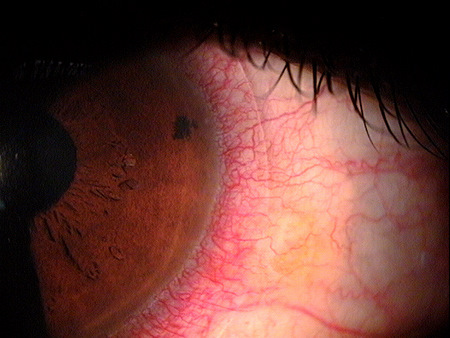 |
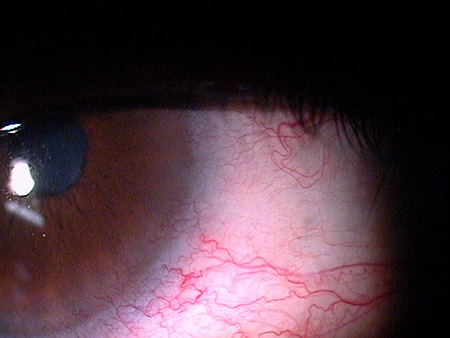
Clinical Appearance of the Bulbar Conjuctiva
|
|
Clinical Appearance of the Bulbar Conjuctiva
|
 |
|
 |
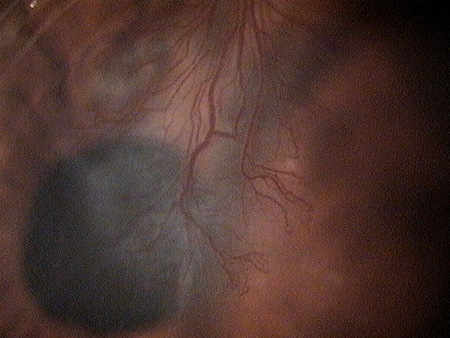
Clinical Appearance of the Cornea
|
Corneal neovascularization is classified as superficial or deep based on its location in the corneal stroma.
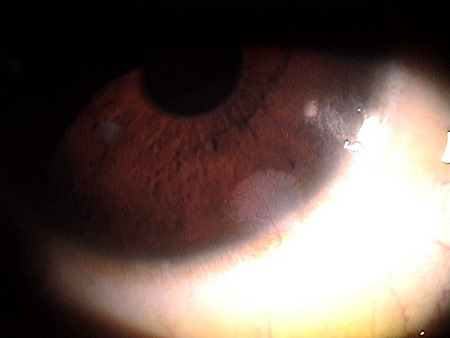 |
Superficial Corneal Neovascularization
|
|
Deep Corneal Neovascularization
|
 |
This would include any other eye diseases where corneal neovascularization is a clinical sign of the disease but is a manifestation of the primary eye disease.
- Interstitial keratitis
- Herpes simplex keratitis
- Herpes zoster
The key to treating corneal neovascularization is to address the underlying condition that causes the stimulation of angiogenic factors in the cornea.
Phamacologic Treatment
- Topical steroids can be used for active neovascularization
Mechanical Treatment
- Discontinue contact lens wear
- Change cornea-contact lens relationship
Surgical Treatment
- Diathermy of large feeder vessels and corneal laser photocoagulation are surgical options to treat pannus
- Limbal grafting is a treatment option for severe chemical injuries and limbal epithelial loss
1. Bowling EL. Vital stains in cornea and contact lens practice. Review of Cornea and Contact Lenses. 2005 Jan/Feb: 25-28.
2. Silbert JA. Is it an ulcer or an infiltrate? RevOptom. 2007 June 15; (6): 91-101.
3. Edwards K, Brian G, Stretton S, Stapleton F, Willcox MD, Sankaridurg PR, Sweeney DF, Holden BA. Microbial Keratitis and Silicone Hydrogel Lenses. Contact Lens Spectrum. 2004 Jan: 38-42.
4. Snyder C. Solution Interaction with the Ocular Surface: The Significance in Making the Grade. Clinical & Refractive Optometry. 2005; 16(5): 134-140.
5. Raizman M. Maintaining Corneal Barrier Integrity. 2007 Oct 15; (10): 5-6.
6. Karpecki PM. Much Ado About Staining. RevOptom. 2006 Nov 15; (11): 135-136.
7. Bowling E. Russell GE. Shovlin JP. Sindt CW. Corneal neovascularization. RevOptom: The Corneal Atlas.
2009 Jan. 10.
370.61
Localized vascularization of cornea
370.63
Deep vascularization of cornea
92285
External ocular photography
92286
Specular endothelial microscopy
Occurrence
- The prevalence of corneal neovascularization is 1% – 20% of the population
Distribution
- Corneal neovascularization is distributed evenly throughout the population
Risk Factors
- Contact lens wear
- Overnight contact lens wear
- Low oxygen transmission contact lenses
- High myopia
- Ocular surface disease
- Ocular injury
- Systemic conditions that affect the ocular surface (i.e., acne rosacea, Sjogren syndrome, immune system dysfunctions)




 Print | Share
Print | Share