ICD-10 Diagnosis Codes:
H18.11–Bullous keratopathy, right eye
H18.12–Bullous keratopathy, left eye
H18.13–Bullous keratopathy, bilateral
Title
Bullous Keratopathy
Category
Corneal Opacity And Other Disorders Of Cornea
Description
Bullous keratopathy is a clinical sign of epithelial edema.
Bullous keratopathy occurs as the result of severe and prolonged corneal edema. The condition occurs when an influx of fluid into the cornea overwhelms the corneas ability to remove the excess fluid. As fluid accumulates in the more anterior layers of the cornea, blisters and epithelial bullae develop.
Bullous keratopathy may occur in any of the following conditions:
- Fuchs’ endothelial dystrophy
- Posterior polymorphous endothelial dystrophy
Most commonly, bullous keratopathy occurs as a unintended consequence of intraocular surgeries:
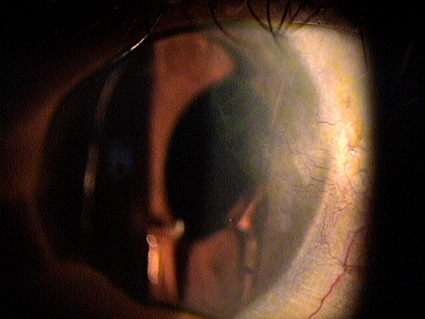
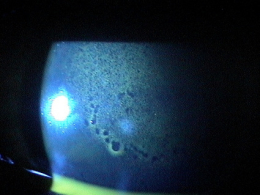
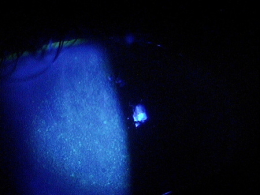
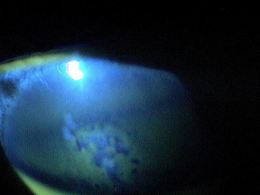
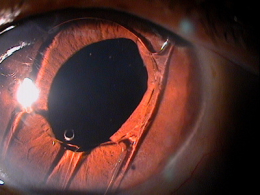
- Pseudophakic bullous keratopathy in a 70-year-old male
Structural Damage to the Eye
The layers of the cornea are optically transparent so that the entire structure can transmit visible light. When viewed in cross-section, the cornea is a basic structure of two covering layers with a central collagen stroma. The outer covering layer is called the anterior cornea. It is composed of the corneal epithelium and a basement membrane called Bowman’s membrane. This layer functions as a semi-permeable membrane that keeps pathogens out of the eye but allows nutrients from the pre-ocular tear film to nourish the anterior cornea.
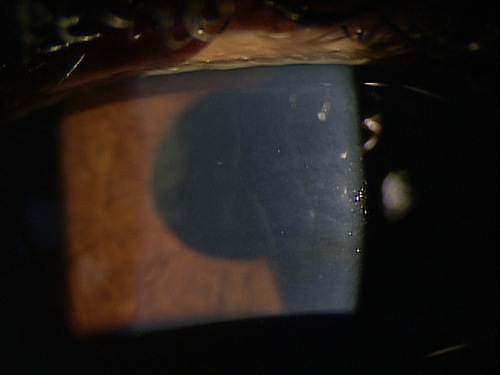
The middle layer of the cornea is called the stroma. This layer comprises over 90% of the cornea’s thickness and is composed of tightly packed collagen fibrils in an orderly lamellar arrangement. The spacing and arrangement of the fibrils makes the corneal stroma optically transparent. To maintain optical transparency, the stroma must be maintained in a state of relative deturgescence and the normal level of stromal hydration is 78% water. The inability to maintain stromal deturgescenece can result in corneal edema and a loss of stromal transparency.
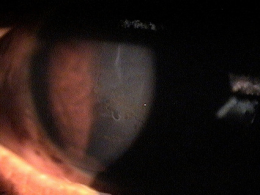
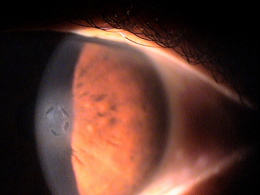
The inner covering layer is called the posterior cornea. It is composed of the corneal endothelium and Descemet’s membrane. This layer fuctions as a semi-permeable membrane that controls fluid and solute transport across the posterior surface of the cornea. Because of the strength and flexibility of Descemet’s membrane, the posterior cornea also serves as a barrier against injury.
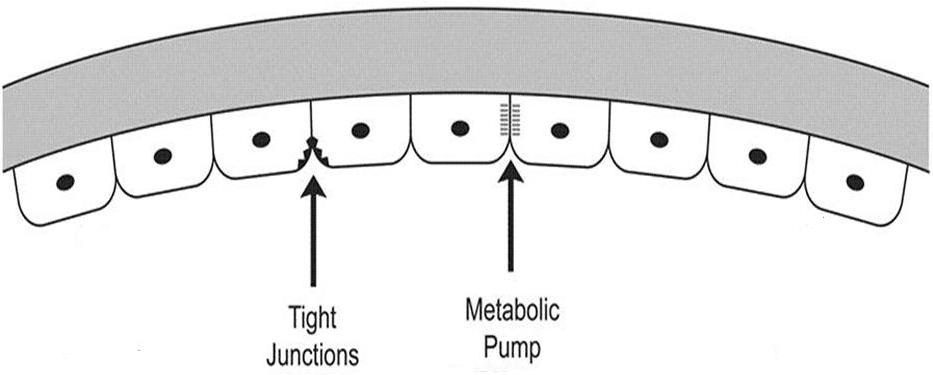 |
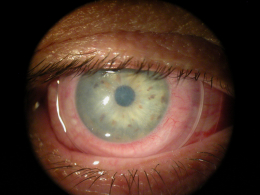
Posterior Cornea
|
|
| Structural Damage to the Eye
|
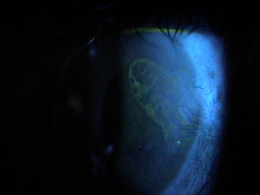
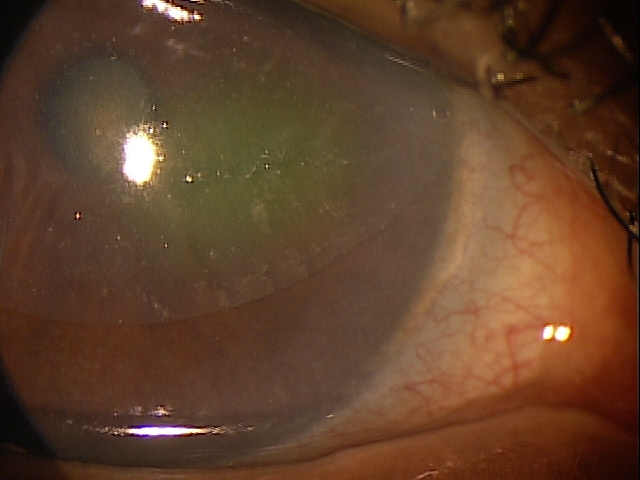
Stromal Edema
|
|
Functional Damage to the Eye
- Decreased visual acuity secondary to epithelial edema
- Epithelial edema produces irregularities in the corneal refractive surface
- At night, with the eye closed, epithelial edema worsens due to a hypertonic environment
- Decreased vision is usually worse in the morning hours
- In advanced stages, bullae (water blister) formation can cause significant ocular pain when they burst
The main goal of the diagnostic evaluation in a patient with bullous keratopathy is to accomplish the following:
- Determine the underlying condition producing the bullous keratopathy
- Relieve ocular discomfort
- Prevent complications that occur with epithelial defects (i.e., infection, uveitis)
- Improve visual acuity
Patient History
Patients will usually present with the following symptoms and/or clinical history:
- Blurred vision
- Eye pain
- Foreign body sensation
- Sensitivity to bright light
- Epiphora
- History of pre-existing corneal disease
- History of previous ocular surgery (especially cataract surgery)
External Ocular Examination with Biomicroscopy
- Loss of stromal transparency
- Folds in Descemet’s membrane
- Obvious thickening of the cornea
- Epithelial blisters and bullae
- Loss of corneal luster
DIAGNOSTIC TESTS
External Ocular Photography
- To document the progress or lack of progress of bullous keratopathy
- To help plan a treatment program
- To document the delivery of the medical treatment
- To document the response to treatment
Because bullous keratopathy can be caused by various eye diseases and conditions and the disease may be classified according to its cause.
Primary Bullous Keratopathy
- Fuchs’ endothelial dystrophy
- Posterior polymorphous dystrophy
- Iridocorneal endothelial syndrome
- Acute increase in intraocular pressure
- Corneal hydrops
- Ocular inflammation
- Herpes simplex or zoster keratitis
Secondary Bullous Keratopathy (most common)
Iatrogenic corneal endotheliopathy
- Pseudophakic bullous keratopathy
- Aphakic bullous keratopathy
Contact lens syndromes (rare)
Ocular injury
None. Possibly very advanced recurrent corneal erosion but an erosion typically does not produce large bullae and erosions have more intermittent symptoms.
Because corneal edema can be caused by various eye diseases and conditions, the condition is treated according to the cause. The first goal of treating patients with corneal edema is to reduce the edema and the associated symptoms of blurred vision and ocular discomfort. Second, best practices treatment guidelines indicate treatment of the underlying condition producing the corneal edema.
Preventative Treatment
- Avoiding or minimizing contact lens wear in patients with preexisting endothelial disease
- Careful consideration of cataract surgery in patients with preexisting endothelial disease
- Patient counseling may include anything from discouraging surgery until visual function is very impaired to consideration of combined procedures to address both the corneal and lenticular issues
Pharmocologic Treatment
Hyperosmotics
- The goal of treatment is to improve visual acuity by deturgescence of the stroma or epithelium. Clinicians should not put too much faith in the efficacy of hyperosmotics in managing bullous keratopathy as they are often “fighting an uphill battle”
- As hyperosmotics are most effective only in the presence of epithelial edema, their use should usually be confined only to cases where the edema has spread to the anterior cornea
Artificial Tears (FreshKote Ophthalmic Solution)
- The goal of treatment is to remove excess water from the epithelium by utilizing the high oncotic pressure of the solution
- Once again, in more advanced cases, this preparation will have little to no effect
Topical Steroids
- Since low grade ocular inflammation is associated with chronic corneal edema, topical steroids can be used in patients with both uveitis and secondary corneal edema
Topical Glaucoma Medications
- Reducing intraocular pressure can be the most effective management tool in treating bullous keratopathy
- Unless IOP is already very low, lowering IOP to a level in the low teens decreases the osmotic demand on the endothelium, giving the endothelium the best chance to maintain proper corneal hydration
- Aqueous suppressants are the primary choice and prostaglandin compounds should be avoided
- A few studies cite a potential stress factor carbonic anhydrase inhibitors play on the corneal endothelium and therefore conclude they are contraindicated in managing endothelial and stromal edema (The conclusions of these studies is debated)
Topical Antibiotic Medications
- Epithelial defects can predispose the cornea to infection
Mechanical Treatment
Bandage Contact Lenses
- In patients with epithelial edema, overnight wear of soft contact lens can be used to decrease pain and improve visual acuity
- In some patients who are not candidates for or refuse surgery for advanced bullous keratopathy, prolonged use of bandage lenses can be very effective at managing extreme epithelial edema and resultant bullae formation
Surgical Treatment
- Endothelial transplant
- Penetrating keratoplasty
- Amniotic membrane placement
Amniotic Membrane Inserts:
1. Aquavella JV. Keratopathy, Pseudophakic Bullous. http://www.emedicine.com/oph/topic107.htm. Last accessed March 30, 2014.
2. Heiting G. Fuchs’ corneal dystrophy: 7 things you should know. http://www.allaboutvision.com/conditions/fuchs-corneal-dystrophy.htm. Last accessed March 30, 2014.
3. Corneal diseases. http://www.innvista.com/health/ailments/eye-ailments/corneal-diseases/. Last accessed March 30, 2014.
4. Ajamian PC. Warning: corneal edema ahead. RevOptom. July 2009;146(7): http://www.reviewofoptometry.com/content/d/cataract___and___refractive_surgery/c/14568/. Last accessed March 30, 2014.
5. Raizman M. Maintaining corneal barrier integrity. RevOptom. Oct 2007; 144(10).
6. Lindstrom RL. Corneal complications after cataract surgery. http://www.ophthalmic.hyperguides.com/tutorials/cataract/corneal/tutorial.asp. Last accessed March 29, 2014.
371.23
Bullous keratopathy
92225
External ocular photography
92286
Specular endothelial microscopy
76514
Corneal pachymetry
92025
Corneal topography
92312
Anterior segment imaging
92071
Bandage contact lens
65778
Amniotic membrane placement
76513
Anterior segment ultrasound




 Print | Share
Print | Share