ICD-10 Diagnosis Codes:
H16.251–Phlyctenular keratoconjunctivitis, right eye
H16.252–Phlyctenular keratoconjunctivitis, left eye
H16.253–Phlyctenular keratoconjunctivitis, bilateral
Title
Phlyctenular Keratoconjunctivitis
Category
Keratitis
Description
Phlyctenular keratoconjunctivitis is an inflammation of the cornea and conjunctiva caused by microbial antigens.
Phlyctenlar keratoconjunctivitis is a form of bacterial hypersensitivity-mediated corneal disease. Phlyctenular keratoconjunctivits is also called phlyctenulosis and other possible etiologies include tuberculosis and Chlamydia.
In most patients, the condition is the result of a reaction with staphylococcal cell wall antigen (i.e., adverse reaction to toxic proteins found on the ocular surface in chronic blepharoconjunctivitis).
The histopathological changes in phlyctenular keratoconjunctivitis begin with the body’s immune response to the microbial antigens. First, accumulations of lymphoid tissue form nodules on the bulbar conjunctiva known as phlyctenules. Then, the conjunctiva surrounding the phlyctenules becomes hyperemic.
Conjunctival phlyctenules may persist for several weeks and are usually self-limiting. However, they may ulcerate as the disease progresses but usually they heal without scarring. In more severe presentations, the conjunctival phlyctenules migrate into the cornea and are then called corneal phlyctenules.
Functional Damage to the Eye
- Decreased visual acuity can occur as a result of the compromised corneal epithelium
The main goal of the diagnostic evaluation in a patient with phlyctenular keratoconjunctivitis is to accomplish the following:
- To establish the diagnosis of phlyctenular keratoconjunctivitis
- To determine any inciting etiologies
- To prescribe appropriate therapy
- To prevent complications
To obtain the information required to determine a clinical diagnosis of phlyctenulosis and prescribe a treatment program, the following service components of a medical eye examination should be performed:
- Patient history
- General medical observation
- Adnexal examination
- External ocular examination with biomicroscopy
In children and young adults, a purified protein derivative (PPD) tuberculin skin test should be considered in the diagnostic evaluation. If tuberculosis is supsected or if the PPD is positive, a chest X-ray is advised.
Patient History
Patients with phlyctenulosis may present with any of the following symptoms:
- Watery eyes
- Red eyes
- Ocular discomfort
- Photophobia
- Eye pain
- Blepharospam
- History of previous episodes
- History of styes or chalazion
External Ocular Examination with Biomicroscopy
Patients with phlyctenulosis may present with abnormal clinical signs in any of the following anatomical areas:
- Tear film
- Conjunctiva
- Cornea
 |
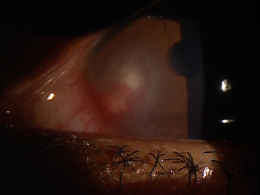
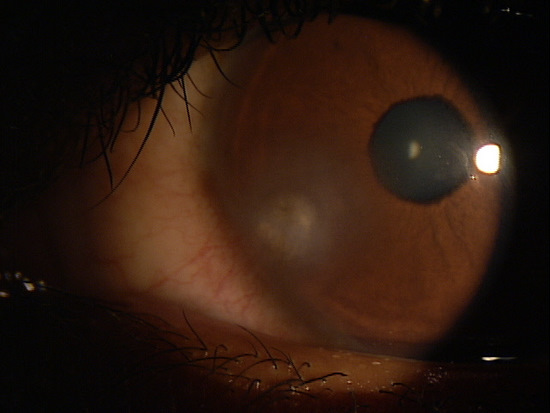
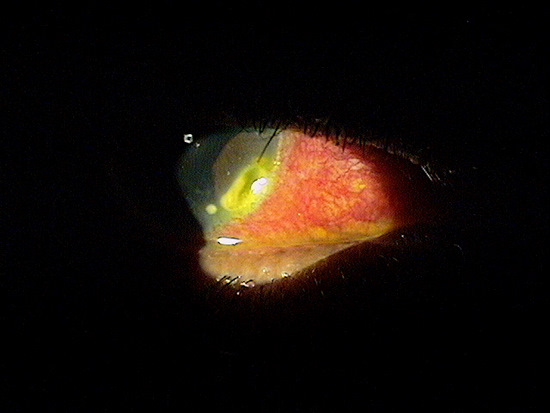
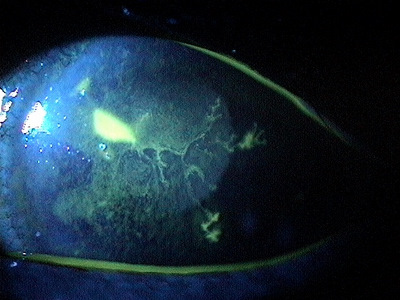
Clinical Apperance of the Cornea
|
|
 |
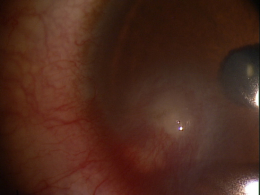
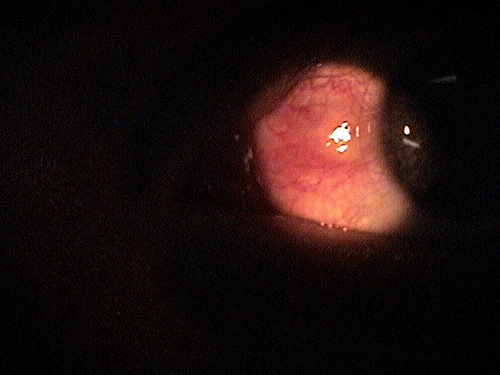
Clinical Appearance of the Cornea
|
|
 |
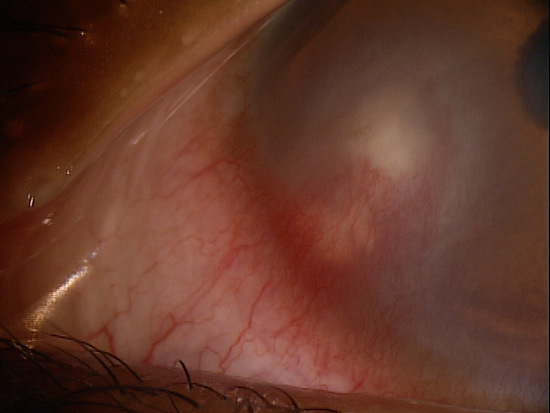
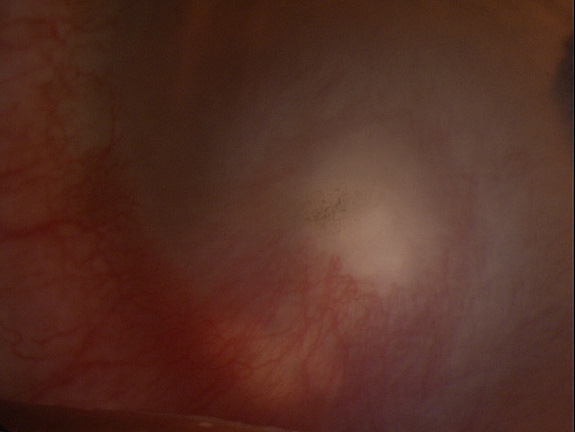
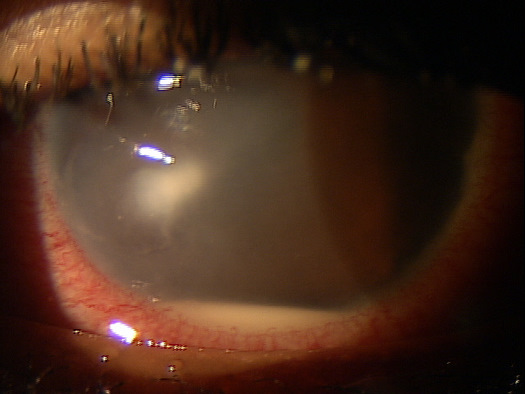
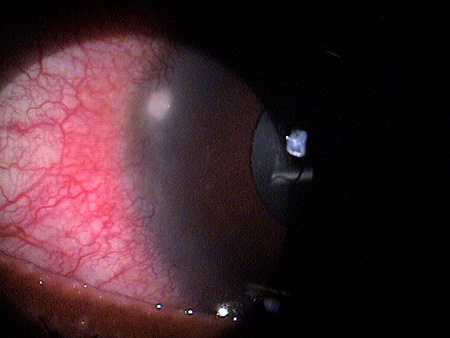
Clinical Appearance of the Cornea
|
There is no classification system for phlytenular keratoconjunctivitis.
 |
Inflamed Pinguecula
|
|
 |
Infectious Keratitis
|
|
 |
Sterile Peripheral Corneal Infiltrate
|
|
 |
Marginal Corneal Ulcer
|
|
 |
Herpes Simplex Keratitis
|
|
 |
Vernal Conjunctivitis
|
Since phlyctenular keratoconjunctivitis is a hypersensitivity reaction to microbial toxins commonly seen with chronic staphloccocal blepharoconjunctivitis, treatment options must include treating these inciting conditions.
Palliative Treatment
- Lid hygeine regimen
- Artificial tears for comfort
Pharmacologic Treatment: Topical Medications
- Steroids in the presence of conjunctival involvement (i.e. Pred Forte q.i.d)
- Antibiotic in the presence of bacterial corneal ulcer (i.e. fluoroquinolones q.i.d)
- Antibiotic ointment (i.e. Erythromycin or Bacitracin qhs)
- Cycloplegic in severe corneal involvement
- Homatropine 2% or 5% t.i.d. – q.i.d.
- Scopolamine 0.25% b.i.d. – q.i.d.
Pharmacologic Treatment: Oral Medications
- Oral antibiotic (i.e. Doxcycline 100 mg p.o. q.d. to b.i.d or Erythromycin 250 mg p.o. q.d. to b.i.d.)
Systemic Treatment
- If the PPD or chest X-ray is positive for TB, refer the patient for further management of the the systemic cause
1. Bowling EL. Vital stains in cornea and contact lens practice. Review of Cornea and Contact Lenses. 2005 Jan/Feb: 25-28.
2. Silbert JA. Is it an ulcer or an infiltrate? RevOptom. 2007 June 15; (6): 91-101.
3. Edwards K, Brian G, Stretton S, Stapleton F, Willcox MD, Sankaridurg PR, Sweeney DF, Holden BA. Microbial Keratitis and Silicone Hydrogel Lenses. Contact Lens Spectrum. 2004 Jan: 38-42.
4. Snyder C. Solution Interaction with the Ocular Surface: The Significance in Making the Grade. Clinical & Refractive Optometry. 2005; 16(5): 134-140.
5. Raizman M. Maintaining Corneal Barrier Integrity. 2007 Oct 15; (10): 5-6.
6. Karpecki PM. Much Ado About Staining. RevOptom. 2006 Nov 15; (11): 135-136.
7. Bowling E. Russell GE. Shovlin JP. Sindt CW. Phlyctenular keratoconjunctivitis. RevOptom: The Cornea Atlas. 2009 Jan: 19.
370.31
Phlyctenular keratoconjunctivitis
92285
External ocular photography
92286
Specular endothelial microscopy




 Print | Share
Print | Share