ICD-10 Diagnosis Codes:
H16.041–Marginal corneal ulcer, right eye
H16.042–Marginal corneal ulcer, left eye
H16.043–Marginal corneal ulcer, bilateral
Title
Marginal Corneal Ulcer
Category
Keratitis
Description
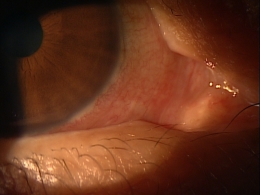
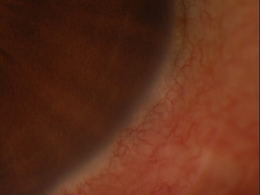
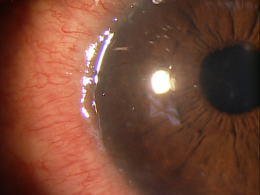
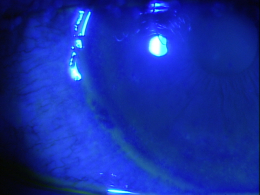
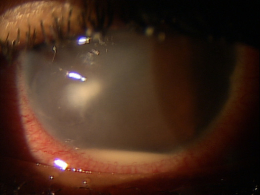
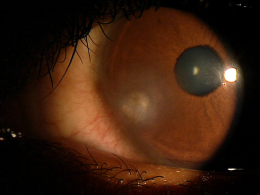
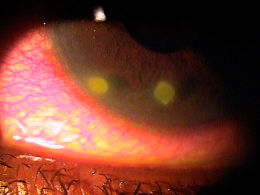
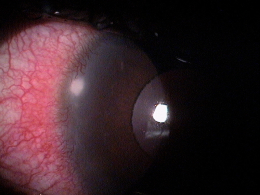
Marginal keratitis is an inflammatory reaction in the cornea characterized by subepithelial marginal infiltrates, ocular redness, increased lacrimation, photophobia and ocular discomfort.
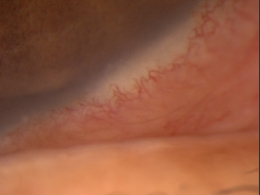
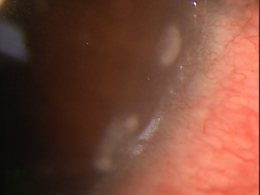
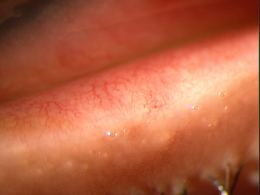
Marginal ulcers can be infectious or non-infectious and infectious ulcers are usually caused by bacteria. The condition is characterized by the appearance of small, gray-white circumlimbal lesions. These infiltrative lesions are separated from the limbus by about 1 mm of clear cornea and they may have overlying epithelial defects.
The focus of this disease glossary is non-infectious marginal ulcers and their presence could be related to any of the following:
- Contact lens wear
- Bacterial by-products from untreated blepharitis
- Autoimmune disease
- Other toxic stimuli
Non-infectious marginal keratitis is an immune system response to corneal damage.
Structural Damage to the Eye
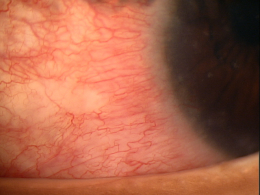
- Localized vasodilation at the limbus secondary to the release of pro-inflammatory cytokines from the cornea
- White blood cells (neutrophils) are recruited into the cornea from the dilated limbal blood vessels
- Marginal infiltrates form from the collection of white blood cells
- The neutrophils release proteases that damage the corneal epithelium
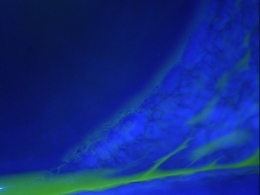
- The resulting micro-ulcer produces overlying corneal staining with vital dyes
- A healed marginal ulcer may leave a scar in the corneal stroma
Functional Damage to the Eye
- None
- Blurred vision secondary to corneal edema
- Fluctuating vision secondary to corneal edema
- Loss of vision secondary to stromal scarring
The goal of the diagnostic evaluation in a patient with marginal keratitis is to accomplish the following:
1. Determine if the lesion is an infectious corneal ulcer or a sterile corneal infiltrate.
- Increased ocular pain, discharge, epithelial staining and a significant anterior chamber reaction are more associated with infectious ulcers
- Decreased infiltrate size, multiple lesions and arcuate locations on the cornea are more associated with sterile corneal infiltrates
2. Prescribe a treatment program.
- Topical antibiotic eyedrops
- Topical steroid eyedrops
- Topical antibiotic/steroid ointment
- Oral antibiotics
- Eyelid hygiene
- Neutraceuticals
Patient History
- Asymptomatic
- Red eyes
- Minor ocular irritation
- Eye pain
- Decreased vision
- Fluctuating vision
External Ocular Examination with Biomicroscopy
- Evaluate the corneal stroma for an infiltrative response
- Look for overlying corneal epithelial defects with vital dyes
- Evaluate the conjunctiva for hyperemia or chemosis
- Evaluate the eyelids for blepharitis
DIAGNOSTIC TESTS
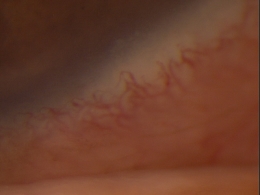
External Ocular Photography
- Document the size, location and extent of the marginal keratitis
- Document the progression or lack of progression of the marginal keratitis
- Help plan a treatment program
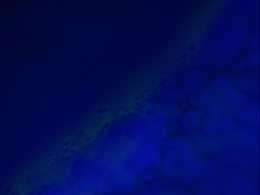
Specular Endothelial Microscopy
- Evaluate the corneal endothelium for signs of inflammation-induced endotheliopathy
- Document the presence or absence of corneal edema
- Help plan a treatment program
The corneal infiltrates found in marginal keratitis are classified by location, severity and cause.
 |
|
Contact Lens-Induced Peripheral Ulcer (CLPU)
|
 |
Microbial Keratitis
This condition is characterized by excavation and necrosis of tissue from the epithelium into the stroma.
- Pain that is severe and increasing
- Ulcer location is often central, but can be paracentral or peripheral
- Focal infiltrates and satellite lesions are possible
The goals of treating meibomian gland disease include the following:
- Improve patient symptoms
- Reduce chronic gland inflammation
- Improve the quality of the meibum secretion
- Prevent damage to the ocular surface
- Prevent meibomian gland dropout
Best practices treatment guidelines from The International Workshop on Meibomian Gland Dysfunction suggest the following treatment options:
Palliative Treatment
- Artificial tears (non-preserved is preferred for frequent use)
- Topical emollient lubricant
- Liposomal spray
- Warm compress therapy
Mechanical Treatment
- Meibomian gland therapeutic expression
Surgical Treatment
- Ductal probing of the meibomian gland
Pharmacologic Treatment
1. Topical azithromycin (e.g., Azasite ophthalmic solution)
2. Topical cyclosporine (e.g., Restasis ophthalmic emulsion)
- If concurrent corneal epitheliopathy is present
- If concurrent aqueous deficiency dry eye syndrome is present
3. Oral tetracyclines
- Tetracycline 250 mg (4x per day for 30 days)
- Doxycycline 50-100 mg (2x per day for 30 days)
- Minocycline 50-100 mg (2x per day for 30 days)
Nutritional Treatment
- Omega-3 fatty acid dietary supplementation to decrease inflammation in the eyelids
In 2003, research presented at the 2003 Annual meeting of the Association for Research in Vision and Ophthalmology found that high dietary intake of omega-3 essential fatty acids decrease the risk of dry eye syndrome. The anti-inflammatory effects of omega-3’s also help the reduce inflammation in the eyelids.
1. Dunbar MT. Infectious Ulcer Or Sterile Infiltrate? Review of Cornea and Contact Lenses. 2007 Oct: 16-20.
2. Sterile Corneal Infiltrates. Handbook of Ocular Disease Management. http://www.reviewofoptometry.com/cmsdocuments/2009/9/ro0409_handbook.pdf. Last accessed July 7, 2014.
3. Bowling EL. Vital stains in cornea and contact lens practice. Review of Cornea and Contact Lenses. 2005 Jan/Feb: 25-28.
4. Silbert JA. Is it an ulcer or an infiltrate? RevOptom. 2007 June 15; (6): 91-101. http://www.revoptom.com/content/d/cornea/c/15408. Last accessed June 7, 2014.
5. Edwards K, Brian G, Stretton S, Stapleton F, Willcox MD, Sankaridurg PR, Sweeney DF, Holden BA. Microbial Keratitis and Silicone Hydrogel Lenses. Contact Lens Spectrum. 2004 Jan: 38-42.
6. Snyder C. Solution Interaction with the Ocular Surface: The Significance in Making the Grade. Clinical & Refractive Optometry. 2005; 16(5): 134-140.
7. Raizman M. Maintaining Corneal Barrier Integrity. 2007 Oct 15; (10): 5-6.
8. Karpecki PM. Much Ado About Staining. RevOptom. 2006 Nov 15; (11): 135-136.
9. Abelson M, Plumer A. Marginal Infiltrates: A Mysterious Malady. 2005 Jan 1. Review of Ophthalmology. http://www.revophth.com/content/d/therapeutic_topics/i/1320/c/25397/. Last accessed June 7, 2014.
370.01
Marginal corneal ulcer
92285
External ocular photography
92286
Specular endothelial microscopy




 Print | Share
Print | Share