ICD-10 Diagnosis Codes:
H16.011–Central corneal ulcer, right eye
H16.012–Central corneal ulcer, left eye
H16.013–Central corneal ulcer, bilateral
Title
Central Corneal Ulcer
Category
Keratitis
Description
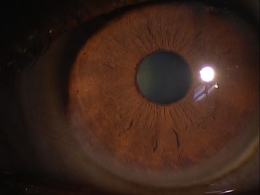
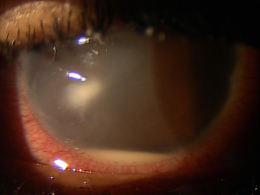
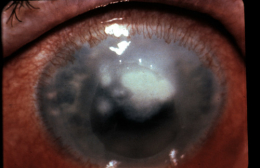
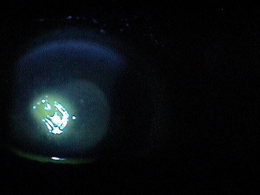
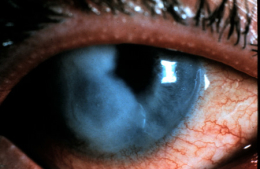
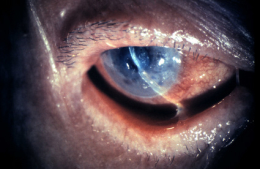
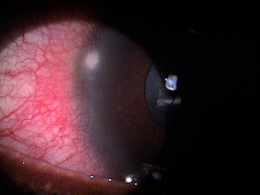
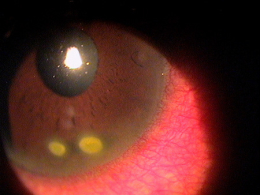
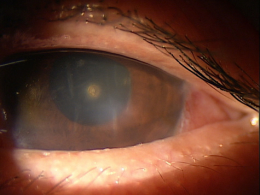
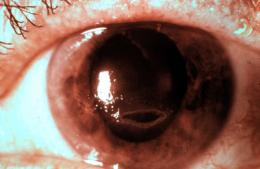
Corneal ulcers are focal white opacities/infiltrates in the corneal stroma with an overlaying epithelial defect.
Corneal ulcers usually stain with fluorescein and can be caused by any of the following organisms.
- Bacteria — the most common causes of corneal ulcers and usually caused by gram positive species
- Viral — the most common cause is herpes simplex
- Fungal — needs to be considered if the patient has had traumatic injury with vegetative matter (i.e., tree branches)
- Atypical mycobacteria — ulcers usually seen in patients with major ocular injuries or corneal grafts
- Acanthamoeba — ulcers caused by acanthamoeba are extremely painful and seen in contact lens patients with poor lens hygiene or has a history of swimming with contact lenses on
The main goal of the diagnostic evaluation in a patient with corneal ulcers is to accomplish the following:
- Determine the etiology of the ulcer
- Develop a treatment plan
- Minimize tissue loss and permanent scarring
- Manage pain and discomfort
Patient History
The patient with a corneal ulcer may present the following signs and symptoms.
- Red eyes
- Photophobia
- Decreased vision in one eye
- Mild-to-moderate discharge
- Mild, moderate, or severe eye pain
Clinical Appearance of the Cornea and Anterior Chamber
- Stain cornea with fluorescein to assess if there is a loss of epithelial tissue overlaying the infiltrate
- Assess the anterior chamber for an inflammatory reaction (i.e., cells and/or flare)
DIAGNOSTIC TESTS
External Ocular Photography
- Document size, shape, location and depth of corneal ulcer
- Document the progress or lack of progress of a corneal ulcer
- Help plan a treatment program
Corneal ulcers can be classified based on their etiology.
Bacterial: These are the most common cause of corneal ulcers. In general corneal infections are assumed bacterial unless otherwise proven. Gram positive species are the most common culprit of bacterial ulcers. The eye will present with mucopurulent discharge. Patient symptoms can range depending on how long the eye has been infected.
Viral: Viral ulcers are usually caused by herpes simplex. The cornea will not appear as necrotic as a bacterial ulcer. The ulcer is more dendritic in nature and eyelid vesicles may also be present.
Fungal: A fungal ulcer are caused by vegetative matter (i.e. tree branches). The infiltrates have feathery borders surround by satellite lesions.
Acanthamoeba: Acanthamoeba related ulcers are extremely painful even though the overall eye looks relatively quiet in comparison to other causes of corneal ulcers. These ulcers can occur in contact lens patients with poor lens hygiene or have a history of swimming with contact lenses on.
Atypical mycobacteria: Atypical mycobacteria are not common causes of ulcers. They can be seen in patients with major ocular injuries or corneal grafts who may be exposed to resistant mycobacteria.
Pharmacological Therapy for Bacterial Corneal Ulcers
1. Cycloplegia
- Atropine 1% t.i.d. for severe cases
- Homatropine 5% t.i.d. for moderate cases
- Cyclopentolate 1% t.i.d. for mild cases
2. Topical antibiotic selection depends on the risk of visual loss
- Low risk of vision loss: small, non-staining fluorescein infiltrate with little to no anterior chamber reaction and minimal discharge
- Non-contact lens wearer: broad spectrum topical antibiotic like Polytrim q.i.d., third generation fluoroquinolones (Ciprofloxacin or Ofloxacin) drops q2-6h until the patient is seen for a one day follow-up
- Contact lens wearer: Tobramycin or Ciprofloxin drop q2-6h in the day and add Tobramycin or Ciprofloxin ointment at bedtime until the patient is seen for a one day follow-up
- Borderline risk: less than 1-1.5 mm peripheral infiltrate or small infiltrate with epithelial defect, mild anterior chamber reaction and moderate discharge
3. Third generation fluoroquinolones (Ciprofloxacin or Ofloxacin) drops qh around the clock until patient is seen again the next day.
- Vision threatening: larger than 1.5 mm staining infiltrate/ulcer, or infiltrate with moderate to severe anterior chamber reaction, purulent discharge or centrally located
4. Fourth generation fluoroquinolones (Vigamox, Zymar, Quixin) every 15 min for 6 hours and then every 30 minutes around the clock until patient is seen again the next day
- No contact lens wear
- Oral pain medications as needed (i.e. Acetaminophen)
- Oral fluoroquinolones (i.e. Ciprofloxacin 500 mg p.o. b.i.d) can penetrate the cornea
One Day Follow-Up
The corneal ulcer should be getting better or staying the same on the one day follow-up. If it is getting worse, check to see if compliance is an issue or if the patient is not getting enough of the drop into the eye. If compliance is not an issue and eye is still not responding, re-evaluate etiology again, consider fortified antibiotics or admission into hospital if endophthalmitis is suspected.
1. Bowling EL. Vital stains in cornea and contact lens practice. Review of Cornea and Contact Lenses. 2005 Jan/Feb: 25-28.
2. Silbert JA. Is it an ulcer or an infiltrate? RevOptom. 2007 June 15; (6): 91-101. http://www.revoptom.com/content/d/cornea/c/15408. Last accessed June 7, 2014.
3. Edwards K, Brian G, Stretton S, Stapleton F, Willcox MD, Sankaridurg PR, Sweeney DF, Holden BA. Microbial Keratitis and Silicone Hydrogel Lenses. Contact Lens Spectrum. 2004 Jan: 38-42.
4. Snyder C. Solution Interaction with the Ocular Surface: The Significance in Making the Grade. Clinical & Refractive Optometry. 2005; 16(5): 134-140.
5. Raizman M. Maintaining Corneal Barrier Integrity. 2007 Oct 15; (10): 5-6.
6. Karpecki PM. Much Ado About Staining. RevOptom. 2006 Nov 15; (11): 135-136.
370.03
Central corneal ulcer
92285
External ocular photography
92286
Specular endothelial microscopy
Occurrence:
The prevalence of corneal ulcer is 0.00011% of the population.
Distribution:
Corneal ulcer is distributed evenly throughout the population.
Risk Factors:
- Contact lens wear
- Active lifestyle involving outdoor activities
- Constant aquatic activity with contact lens wear




 Print | Share
Print | Share