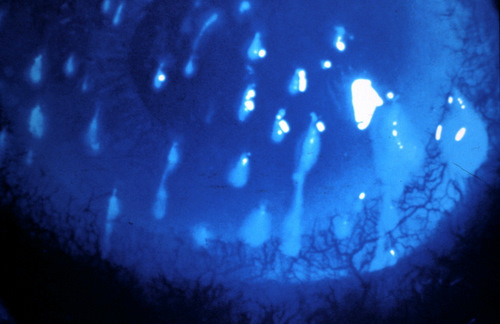
Filamentary keratitis is characterized
by filaments adhering to the cornea
|
ICD-10 Diagnosis Codes: H16.121–Filamentary keratitis, right eye
|
Filamentary keratitis is a type of keratopathy that is associated with the following diseases:
- Dry eye syndrome
- Recurrent corneal erosion
- Bullous keratopathy
- Superior limbic keratoconjunctivitis
- Herpes simplex
- Medicamentosa
- Ptosis
- Connective tssue disorders
- Diabetes
- Psoriasis
The histopathological changes begin as groups of inflammatory cells and fibroblasts infiltrate Bowman’s layer and cause focal elevations on the surface of the cornea. The elevated corneal epithelial defects are irritated by the shearing effects of blinking eyelids and a secondary inflammatory response leads to increased mucus production.
 |
 |
Structural Damage to the Eye
- Because of their elevation, the epithelial defects act as receptor sites for the excess mucus. Corneal filaments form when the normally soluble mucus components of the tear film become compromised.
- When these mucins become corrupted, they precipitate out as particles or strands and damaged epithelial cells bind to them. The binding of the mucin strands with epithelial cells result in the formation of long filaments that adhere to the elevated sites on the corneal surface.
- Corneal filament formation results in structural damage to the cornea. As a patient blinks, the corneal filaments get tugged on and damage the corneal epithelium. This mechanical traction from the eyelids stimulates corneal nerve endings and causes moderate to severe ocular pain.
Functional Damage to the Eye
- Decreased visual acuity can occur as a result of the compromised corneal epithelium and is related to the extent or location of the corneal filaments.
The main goal of the diagnostic evaluation in a patient with filamentary keratitis is to accomplish the following:
- Determine the underlying etilogy of the filamentary keratitis
- Relieve ocular pain and discomfort
- Prescribe a treatment program to treat the underlying condition
Patient History
Patients will usually present with symptoms that range from mild foreign body sensation to severe pain. Episodic tearing and photophobia may also be present. Depending upon the underlying etiology, filamentary keratitis may be unilateral or bilateral. Patients with filamentary keratitis may report that their eyes feel better when they are closed.
Adnexal Examination
Pseudoptosis of the eyelid may be present during gross examination of the face and adnexa. Ask the patient about the history of the ptosis to determine if it is a recent occurrence or if it has been present for a long time.
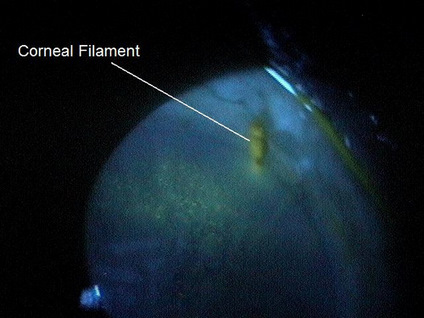 |
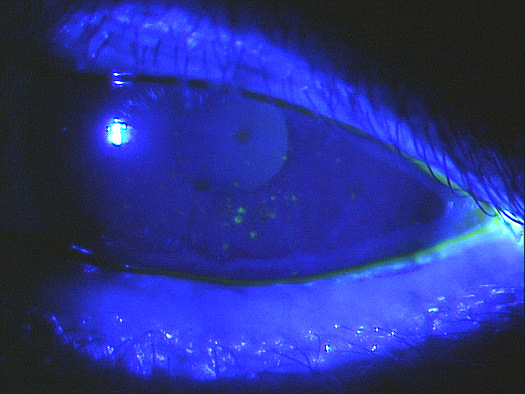
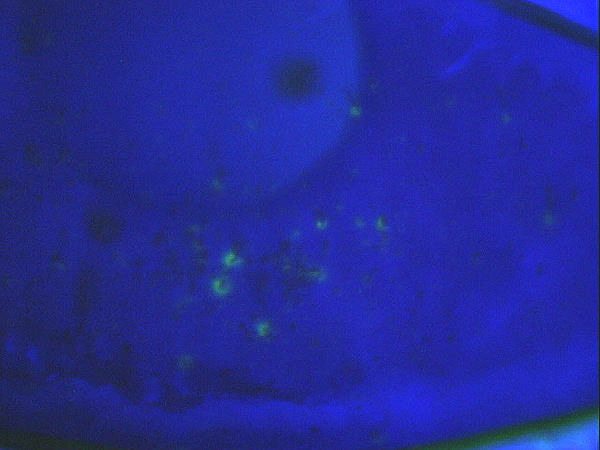
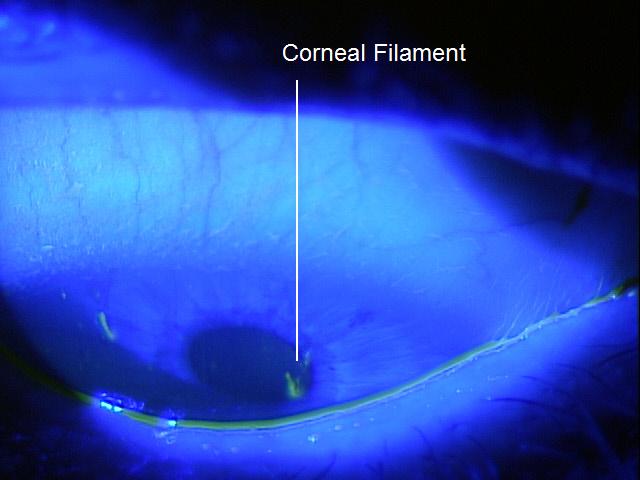
Clinical Appearance of the Cornea
|
|
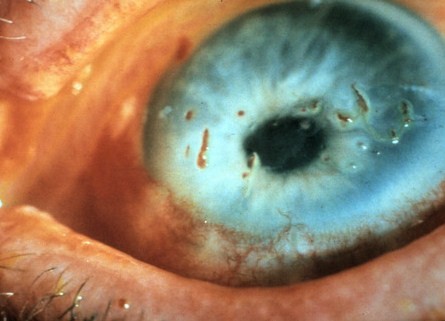 |
Clinical Appearance of the Cornea
|
|
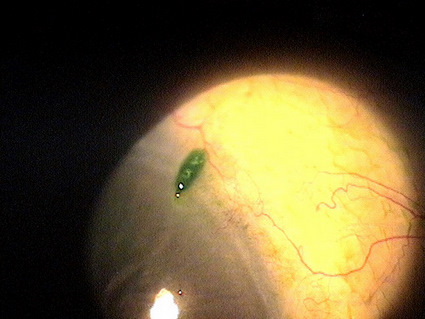 |
Clinical Appearance of the Cornea
|
DIAGNOSTIC TESTS
- Document the extent of the corneal filaments
- Document any other associated structural changes to the cornea and the eyelids
- Help plan a treatment program
- Document the progress or lack of progress of the filamentary keratitis
- Document the delivery of medical treatment
- Document the response to treatment
No specific classification exists for filamentary keratitis. In a general sense, filamentary kerartitis may be classified as mild, moderate, or severe.
 |
Mild Filamentary Keratitis
|
 |
Differential diagnosis would include any other disease that presents with strands of tissue or debris on the corneal surface.
Corneal Laceration
|
The key to treating filamentary keratitis is to address the underlying condition that causes the corneal filaments to form. In addition, the patient should be educated on the potential need for long-term treatment and/or recurrent therapy.
Pharmacologic Treatment
- Non-preserved artificial tears can be used to lubricate the cornea and relieve ocular discomfort
- Topical steroid eye drops can modify or reduce the number of mucus receptor sites by inhibiting inflammatory cells and fibroblasts at the base of the corneal filament
- Topical immunomodulator eye drops (Restasis) can reduce dry eye-induced inflammation and increase aqueous production
- Topical 5% hypertonic solution reduces the formation of corneal filaments by inhibiting receptor site formation and increasing the tear-to-mucus ratio of the precorneal tear film
- Acetylcystene 10% can help eliminate the filament formation in severe presentations
Mechanical Treatment
- Bandage contact lenses with prophylactic antibiotic eye drops can be used in moderate to severe presentations
- The contact lens protects the damaged epithelium from the shearing effects of the eyelids and allows the damaged basal cells of the epithelium to attach to Bowman’s membrane
- Smooth attachment of the basal epithelial cells to Bowman’s membrane prevents the formation of the focal elevations that serve as receptor sites for the corneal filaments
- Pressure-patching can be used for short-term treatment to eliminate corneal filaments in moderate-to-severe presentations
Surgical Treatment
- Punctal occlusion is an option for patients with aqueous deficiency dry eye syndrome
- Corneal filaments may be removed by apllying topical anesthetic and using forceps or a cotton-tipped applicator to gently remove the filaments by grasping them at their base attachment to the cornea
1. Bowling EL. Vital stains in cornea and contact lens practice. Review of Cornea and Contact Lenses. 2005 Jan/Feb: 25-28.
2. Silbert JA. Is it an ulcer or an infiltrate? RevOptom. 2007 June 15; (6): 91-101.
3. Edwards K, Brian G, Stretton S, Stapleton F, Willcox MD, Sankaridurg PR, Sweeney DF, Holden BA. Microbial Keratitis and Silicone Hydrogel Lenses. Contact Lens Spectrum. 2004 Jan: 38-42.
4. Snyder C. Solution Interaction with the Ocular Surface: The Significance in Making the Grade. Clinical & Refractive Optometry. 2005; 16(5): 134-140.
5. Raizman M. Maintaining Corneal Barrier Integrity. 2007 Oct 15; (10): 5-6.
6. Karpecki PM. Much Ado About Staining. RevOptom. 2006 Nov 15; (11): 135-136.
7. Diller R. Sant S. A case report and review of filamentary keratitis. Optometry. 2005 Jan 1; 76(1): 30-36.
8. Simon R. Don’t let FK get carried away. RevOptom. 2011 Oct 15; (10): 98-104.
370.23
Filamentary keratitis
68761
Closure of lacrimal punctum by plug
92285
Ocular photography
92071
Bandage contact lens
Occurrence
Filamentary keratitis is commonly seen in patients with severe dry eye syndrome.
Distribution
Filamentary keratitis is not evenly distributed in the general population.
Risk Factors
- Advancing age
- Female
- History of dry eye syndrome
- Rheumatoid disease
- Thyroid disease




 Print | Share
Print | Share