ICD-10 Diagnosis Codes:
H11.041–Peripheral pterygium, stationary,right eye
H12.042–Peripheral pterygium, stationary, left eye
H12.043–Peripheral pterygium, stationary,bilateral
Title
Pterygium
Category
Disorders Of The Conjunctiva
Description
A pterygium is a type of conjunctival degeneration.
Corneal edema is a clinical sign of corneal disease. The condition is characterized by an increase in corneal thickness secondary to an abnormal accumulation of fluid. The excess fluid produces a swelling of the corneal tisssue and can result in a loss of stromal transparency that produces blurred vision or visual impairment.
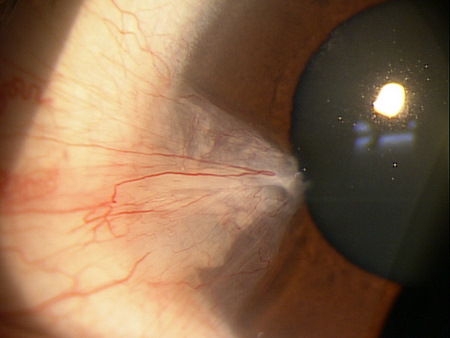
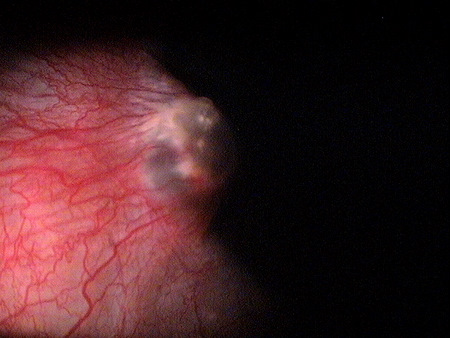
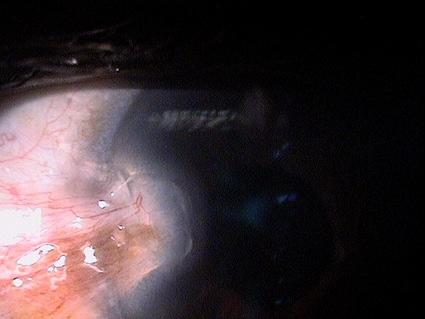
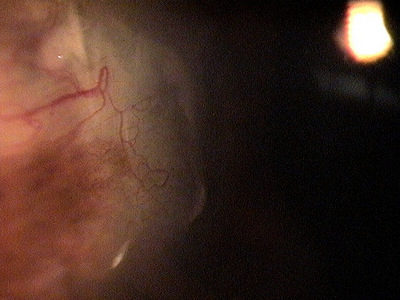
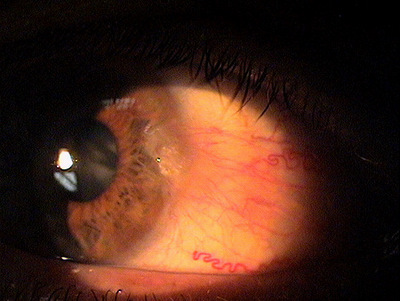
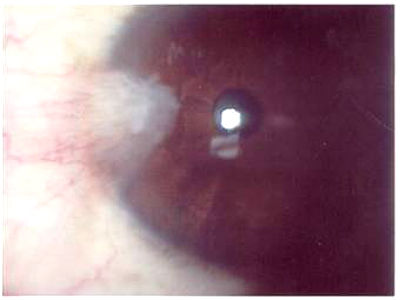
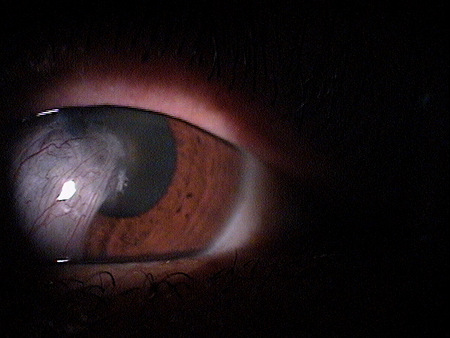
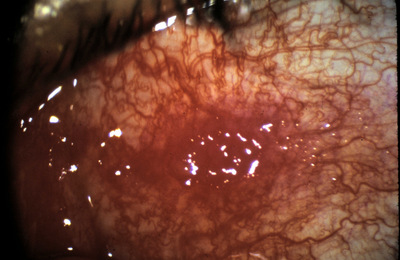
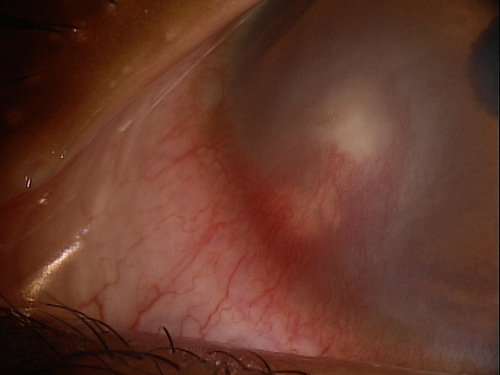
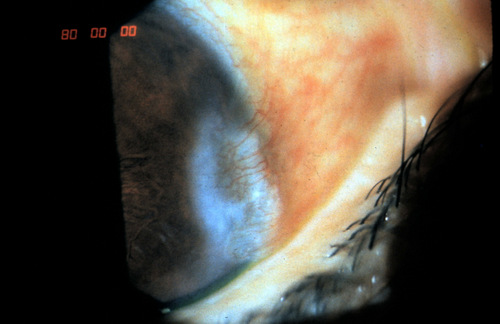
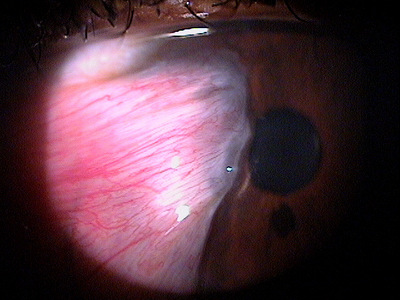
A pterygium presents as an elevated, superficial, external ocular mass on the perilimbal conjunctiva that grows into and onto the cornea. Pterygia can vary in size, height, and rate of growth.
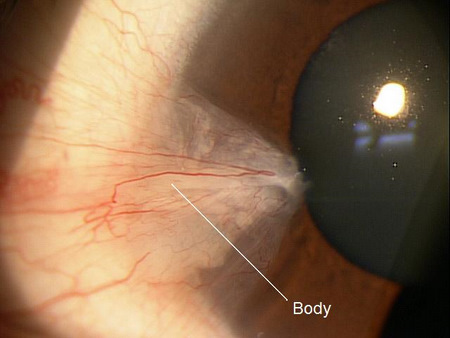
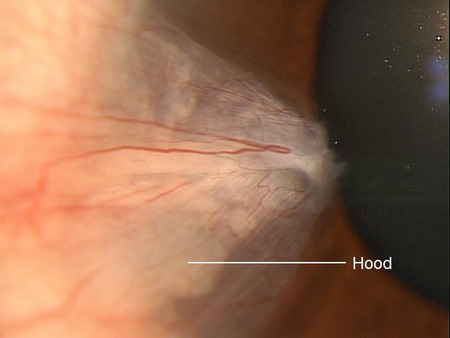
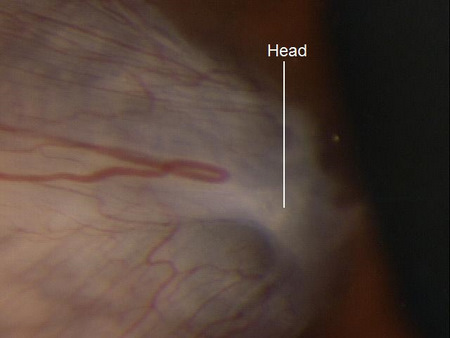
The typical triangular-shaped lesion is comprised of three different anatomic segments.
- Body
- Hood
- Head
A pterygium is a mass characterized by collagen degeneration in the bulbar conjunctiva, fibrovascular proliferation, and an overylying covering of epithelium.
A pterygium evolves through a sequence of three milestones:
1. Small opacity appears of the surface of the conjunctiva
2. Focal limbal failure occurs as the pterygium enlarges- (conjunctivalization of the cornea)
3. Conjunctivalization of the cornea damages corneal structure and decreases function
1st Milestone — Opacification of the conjuctiva
- In its early stages, a pterygium usually appears as a small opacity of the surface of the conjunctiva at the nasal limbus
- As it develops, the lesion spreads to become a fleshy, raised area
2nd Milestone — Focal limbal failure occurs
Functional Damage to the Eye
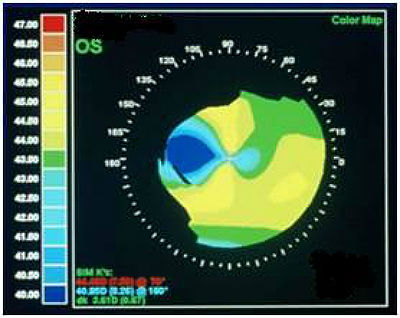
- Irregular astigmatism may be created by pterygium encroachment onto the corneal surface and produce visual impairment
- An elevated pterygium may produce disturbances in the precorneal tear film that disrupt vision
- Large, aggressive, rapidly growing pterygia can obscure the visual axis of the cornea
 |
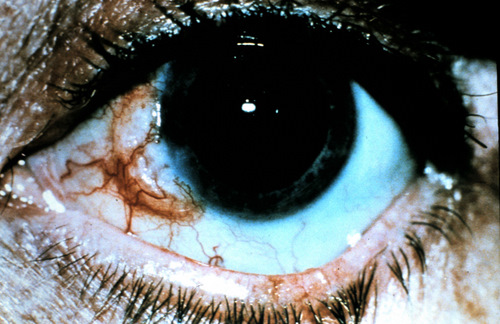
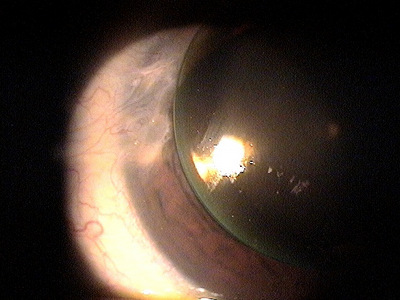
Progressive Pterygium
|
The main goal of the diagnostic evaluation is to accomplish the following:
- Identify the lesion
- Evaluate the cornea for structural damage or functional loss
- Identify risk factors for pterygium development
- Prescribe a treatment program
Patient History
Patients with pterygium present with a variety of complaints, ranging from no symptoms to any or all of the following:
- Persistent ocular redness
- Foreign body sensation
- Dry eyes
- Itchy eyes
- Swelling
- Decreased vision
Clinical Appearance of the Conjunctiva
- Pterygium encroachment onto and into the cornea
DIAGNOSTIC TESTS
The clinical presentation of pterygia can be divided into two general categories – Stationary and Progressive.
This would include any other disease that presents as an interpalpebral conjunctival mass or elevation. Lesions with this clinical appearance mayalso be a clinical sign of the following diseases or conditions.
Conjunctival Tumors
- Conjunctival intraepithelial neoplasia
- Papilloma
- Malignant neoplasms
- Nevus
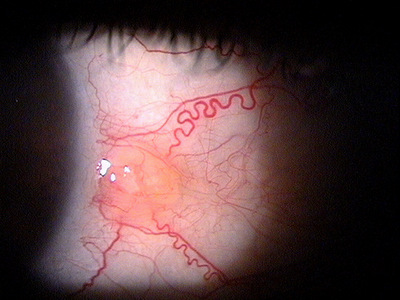
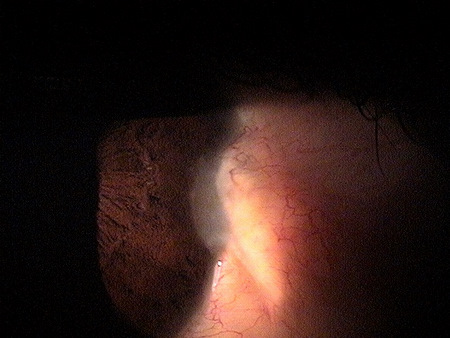
Conjunctival intraepithelial neoplasia (CIN) is the most common mis-diagnosis of a pterygium that can have significant consequences. CINs are the most common primary conjunctival tumor, more commonly seen in those with lighter skin and/or higher degrees of UV exposure. They have a hallmark presentation of blister-like appearances on the conjunctiva, a “frosted” appearance onto the cornea, suspicious vascularization, and in the later stages actual ulceration of the tissue near the limbus. CIN are precursors to squamous cell carcinoma.
Any lesions with findings suspicious for CIN should be referred for an incisional biopsy and likely surgical removal.
Pseudopterygium
A pseudopterygium occurs when a fold of conjunctiva becomes attached to the peripheral cornea. It is caused by corneal inflammation secondary to any of the following conditions:
- Chemical burns
- Peripheral corneal ulcer
- Corneal perforation
- Contact lens wear
- Cicatrizing conjunctivitis
Patients with a normal pterygium can be observed. If the pterygium is small and stable, it is an option. The best way to document and monitor a pterygium is by corneal topography. This will not only document the extent of encroachment but will more importantly document the effect the distortion is having on the visual axis.
Preventative Treatment
- Decrease excessive exposure to wind and sunlight (UVA and UVB)
- Aggressively treat any coexisting ocular surface disease
- Discontinue contact lens wear
- Prescribe contact lenses that do not irritate a pre-existing pterygium
Medical Treatment
- Aggressive lubrication treatment
- Topical steroids if moderate to significant inflammation exists
Surgical Treatment
The only effective treatment for aggressive pterygium growth or pterygia encroaching on the visual axis is surgical removal.
1. Rao SK. Pterygium: a review. eJournal of Ophthalmology. http://www.ejournalofophthalmology.com/ejo/ejo40.html. Last accessed April 2, 2014.
2. Fisher JP. Pterygium. Medscape. http://emedicine.medscape.com/article/1192527-overview. Last accessed April 2, 2014.
3. Skorin L. Become familiar wih advances in pterygium surgery. Primary Care Optometry News. 2009 January: 14.
4. Aminlari A. Singh R. Liang D. Management of pterygium. American Academy of Ophthalmology. http://www.aao.org/publications/eyenet/201011/pearls.cfm. Last accessed April 2, 2014.
372.41
Peripheral pterygium, stationary
92025
Corneal topography
92285
External ocular photography
92132
Anterior segment imaging
76513
Anterior segment ultrasound




 Print | Share
Print | Share