ICD-10 Diagnosis Code:
H53.52–Acquired color vision deficiencies
Title
Acquired Color Vision Deficiencies
Category
Visual Disturbances
Description
Acquired color vision defects may be associated with various eye, optic nerve or brain diseases.
Several eye diseases and clinical conditions can affect a person’s color vision. Structural damage to some component of the afferent visual sensory system leads to a loss of visual function (e.g., loss of chromatic discrimination) that is called dyschromatopsia.
Retinocortical Visual Pathway
- Photoreceptors
- Ganglion cells
- Synaptic elements
- Axons
- Lateral geniculate nucleus
- Visual cortex
In patients with acquired dyschromatopsia, the chromatic defects are characterized by a reduction in a person’s ability to discriminate between different wavelengths of visible light. A common characteristic of acquired color vision defects is that many patients report a raised saturation threshold, giving colors a washed-out appearance.
Acquired color vision defects differ from genetic color deficiencies in several other aspects:
- The loss of color vision is apparent to the affected persons
- Color vision defect is describable in ambiguous terms
- The loss of color discrimination may be asymmetric
- The defect(s) may be widely spread over the color spectrum
- The defect may be unstable over time
Common conditions that can affect a person’s color vision include the following:
- Normal age-related deterioration in chromatic discrimination ability
- Yellowing caused by cataract results in a loss of hue discrimination
- Diseases that result in a loss of foveal function
- Optic nerve disease
- Retinal dystrophies
- Neurologic disease
- Neurologic injury
- Visual field defects
- Common drugs and substances
The pathogenesis of acquired chromatic defects is not completely understood. The most accepted hypothesis invokes a mechanism that involves selective damage to specific components of the afferent visual sensory system. In this theory, impairment of color vision is the result of damage to one or more of the individual neural mechanisms responsible for mediating color vision.
Color vision starts when the three cone photoreceptors convert electromagnetic radiation into a neural signal. Within the retinocortical neural pathway in the brain, there are color discrimination channels that transmit chromatic information to the visual cortex. The signals are transmitted by the parvocellular and koniocellular neural pathways in the brain.
- Red-green chromatic information is transmitted along the parvocellular pathway
- Blue-yellow chromatic information is transmitted along the koniocellular pathway
Structural Damage to the Eye
There are fundamentally different underlying mechanisms of color vision impairment in different classes of disease. In addition, the pathophysiology of acquired color vision loss varies depending upon the anatomical depth of the disease damaging the neural color discrimination channels. Structural damage may occur at any of the following depths:
- Prereceptor — ocular media absorption properties
- Receptor cells — red cones, blue cones, green cones and their ganglion cells
- Postreceptor — retinocortical neural pathways in the brain
Dyschromatopsia of Optic Neuritis
In contrast to genetic color vision defects, which are always bilateral, acquired color vision deficiencies like the dyschromatopsia of optic neuritis can be monocular. The inflammatory demyelination in optic neuritis can produce a loss of visual function that includes decreases in central vision, spacial acuity and color discrimination.
The dyschromatopsia of optic neuritis is characterized by the following:
- No single type of color vision defect is consistently associated with optic neuritis
- The majority of the selective defects were blue-yellow at the time of the acute demyelination event
- Red-green and non-selective color defects were also seen at the time of the acute demyelination event
- Color defects can change over time or remain the same
- The severity of the initial central acuity loss is associated with the likelihood of persistent dyschromatopsia
- Red-green defects are more common in persistent dyschromatopsia (e.g., 6 months or more after acute event)
- Blue-yellow and non-selective color defects are also seen in persistent dyschromatopsia
- Strong association between spatial distribution of visual field defects and hue-discrimination defects (i.e., field depression at the fovea vs. perifovea)
Dyschromatopsia of Glaucoma
- Blue-yellow color deficiency is found in 30% – 50% of patients
- General loss of chromatic discrimination affects 20% – 30%
- Red-green deficiency is seen in 5% of patients
- 20% – 40% of patients with glaucoma never develop chromatic defects
- Some patients develop them in only the advanced stages of the disease
Dyschromatopsia associated with Diabetes/Diabetic Retinopathy
- Chromatic defects may precede diabetic retinopathy in up to 55% of patients
- Reduced chromatic discrimination occurs in 55% – 65% of patients with diabetic retinopathy
- Diabetes could affect visual function at all anatomic levels
- OCT scan may reveal retinal atrophy at the macula
- Blue-yellow color deficiency is found in 89% of patients with chromatic defects
- No regard to the relative spatial distribution of visual field defects
Dyschromatopsia associated with Plaquenil
- Early clinical signs include perifoveal ganglion cell damage (characterized by localized thinning of the outer)
Functional Damage to the Eye
- Loss of chromatic discrimination
- Decreased visual acuity
- Visual field abnormalities
- Pupil abnormalities
- Abnormal VEP and ERG waveforms
The goal of the diagnostic evaluation in a patient with an acquired color vision deficiency is to accomplish the following:
- Use the the correct color vision test or combination of tests to obtain clinically significant information
- Differentiate whether the color vision defect is congenital or acquired
- Determine if the color vision defect is unilateral, asymmetric, or transient
- Identify the primary condition that is producing the color vision defect
- Prescribe a treatment program
Patient History
Patients with acquired color vision deficiencies may present with some or all of the following signs and symptoms:
- None
- Decreased visual acuity
- Loss of visual field
- Altered color vision
- Preexisting eye disease
- Preexisting systemic disease
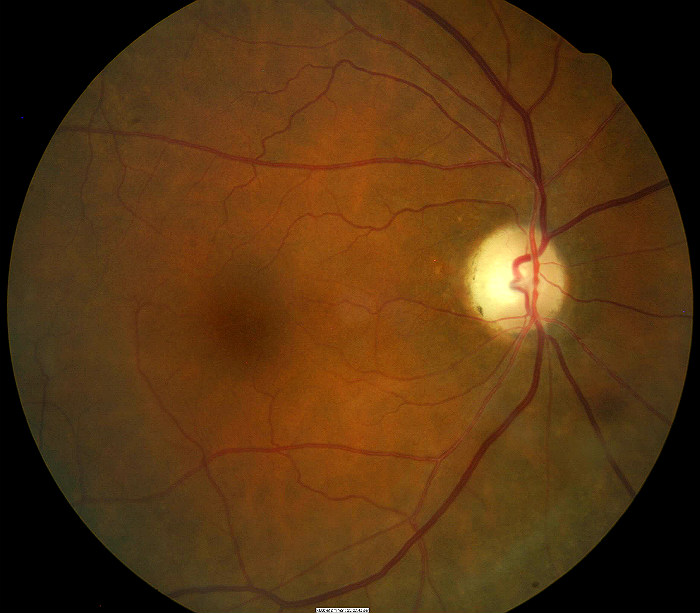
Clinical Appearance of the Retina
The retinal changes associated with acquired color vision deficiencies include the following:
- None
- Pigmentary disorganization at the macula
- Retinal hemorrhaging
- Retinal ischemia
- Optic nerve atrophy
- Optic nerve edema
DIAGNOSTIC TESTS
Color Vision Examination
Because acquired color vision defects tend to be blue-yellow, for best results, formal tests for acquired color vision deficiencies should either broadly cover the full color spectrum or concentrate on the bluish-green to purple region. Screening tests devised to diagnose genetic red-green color defects like Ishihara pseudoisochromatic plates cannot be used alone to diagnose patients with a loss of color vision caused by eye disease, neurologic disease, systemic disease or toxic drug exposure.
If you are relying on pseudoisochromatic plates as your primary screening mechanism, you could add an auxiliary color vision tests such as Sahlgren’s Saturation Test or the Velhagen-Brosch-mann plates that concentrates on the bluish-green to purple color region to cover the full spectrum.
The Farnsworth D-15 test, although popular, allows anomalous trichromats with good or superior chromatic discrimination to make no errors or show only minor transposition errors. Alternatively, the Farnsworth D-100 is more accurate, but it is very time-consuming and does not illuminate saturation deficits.
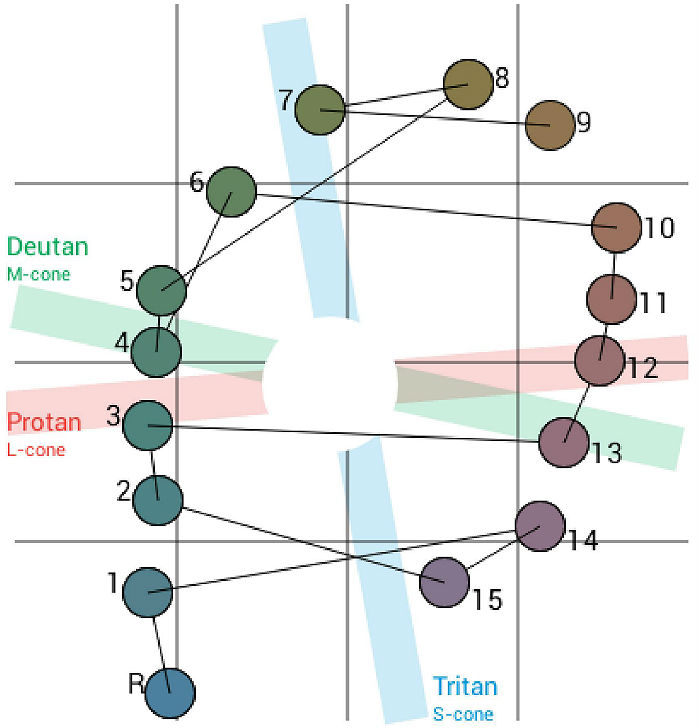
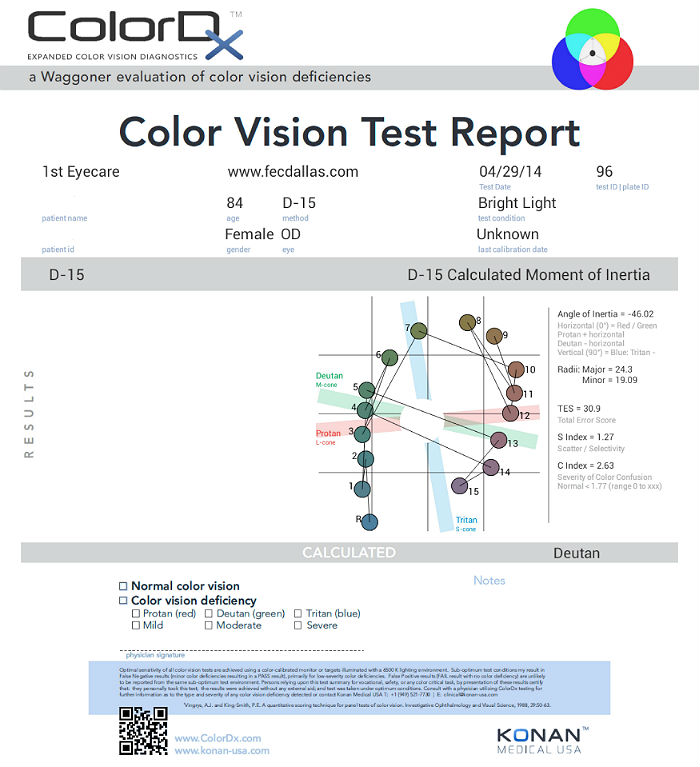
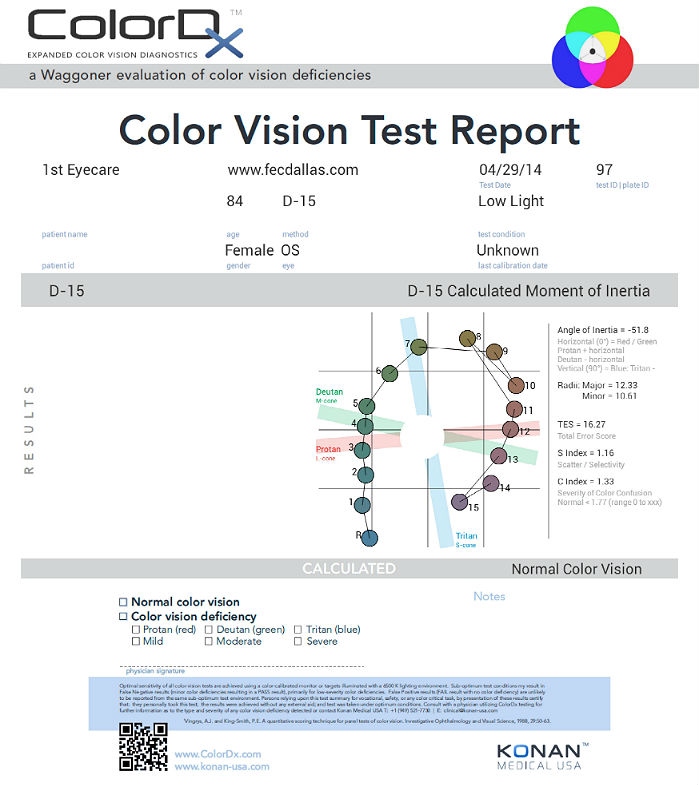
Current best practices suggest’s that the best way to test for acquired dyschromatopsia in clinical practice is with Konan Medical’s Expanded Color Vision Diagnostics software called ColorDx. The Extended Adult Adaptive Evaluation is the best testing strategy for diagnosing acquired color vision deficiencies.
The Extended evaluation consists of 5 sections and is adaptive based upon the results of the General Section.
1. General: 26 test plates for genetic color vision deficiencies
2. Tritan: 12 test plates for acquired deficiencies
Conditional Sections below are added if parts of the General section are missed
3. Protan: extended test for quantification of Protan (red) deficiencies
4. Deutan: extended test for quantification of Deutan (green) deficiencies
5. D-15: extended synergistic test for alternate evaluation methods
Refraction
- 20/30 best corrected visual acuity in the right eye
- 20/25 best corrected visual acuity in the left eye
Fundus Photography
- Temporal pallor of the right optic disc
- Partial optic atrophy in the right eye
 |
 |
|
 |
 |
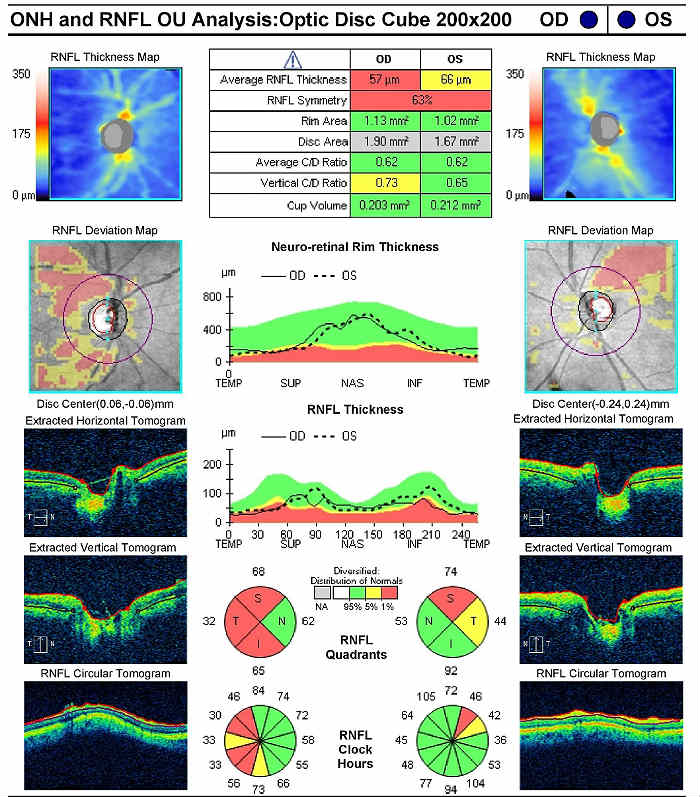
Retinal Scanning Laser
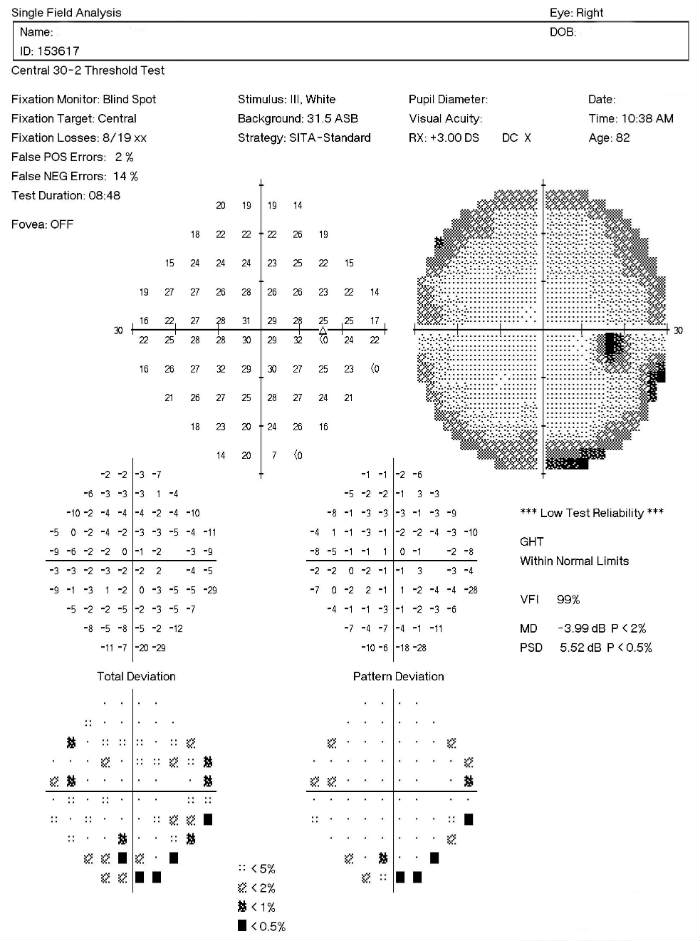
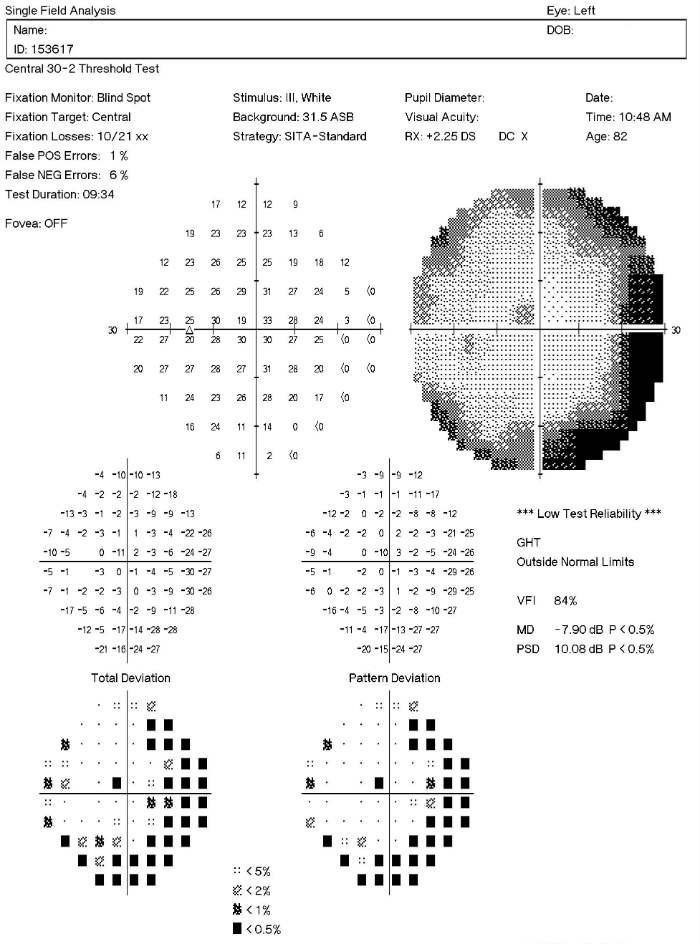
Visual Field Examination
Color Vision Examination
Extended color vision testing divides people into two groups. The first group consist of people with normal color vision and slight color deficiency. The second group consists of people with moderate or severe color deficiency.
The most common test performed in clinical practice is the Farnsworth D15 and the procedure can be accomplished using Konan’s Color Dx software. The test consists of fifteen colored bars and one fixed bar. The hue of each bar has been chosen so that adjacent bars have approximately equal hue differences. When the bars are arranged in order they form a hue circle. As a result, errors in hue discrimination can be made across the hue circle.
Patients with normal color vision usually make no error but may make one or two minor transposition errors, as do those with mild color vision deficiency. Patients with more advanced color deficiency make some or more of the following errors:
- They place colors that lie on the opposite side of the hue circle next to colors that lie on their confusion locus (e.g., diametrical errors)
- Two or more diametrical crossing errors indicates a “failed” test
- If diametrical crossing errors are made, the orientation of the crossing produces a diagnosis of protan, deutan, or tritan color vision deficiency
Acquired color vision deficiencies are classified by severity, selectivity, type and etiology.
Genetic Color Vision Deficiency
Red-green color vision deficiencies are manifest in early infancy. Most patients are males and once fully expressed the disease remains stable throughout life. Genetic color vision defects are not accompanied by any structural abnormalities visible on ophthalmoscopy and there are no other associated clinical abnormalities.
Because genetic color deficiencies occur in 8% of males, incidental occurrence of such defects may be found unrelated to the eye disease being evaluated
The goals of treating a patient with an acquired color vision deficiency include the following:
- Differentiate between congenital and acquired color vision deficiency
- Identify the disease causing the acquired color vision defect
- Prescribe a treatment program
Supportive Treatment for Systemic Etiology
In patients with diabetes, structural damage in the retina from diabetic retinopathy may result in acquired color vision defects. If the patient does not have a type of retinopathy that is treatable with laser surgery, topical steroids or ocular injections, then supportive treatment for the patient’s diabetes is the best treatment option.
- Diet
- Exercise
- Medicine
- Glucose control
In patients with multiple sclerosis, demyelination of the optic nerve may produce an acquired color vision defect. Referral to a neurologist to treat the multiple sclerosis is the best treatment option.
Supportive Treatment for Retinal Etiology
In patients with macular degeneration structural damage in the retina may result in acquired color vision defects. If the patient’s macular degeneration cannot be treated with laser surgery or ocular injections, then nutritional therapy that includes antioxidants and other neutraceuticals is the best treatment option.
In patients taking plaquenil, a toxic maculopathy may develop and produce an acquired color vision defect. Because significant structural damage is usually required to produce a color vision defect, the treatment of plaquenil-induced color vision loss is cessation of plaquenil
1. Karpecki P, Shechtman D. Color Me Curious. RevOptom. 15 Feb 2013. http://www.revoptom.com/content/c/39720/dnnprintmode/true/?skinsrc=%5Bl%5Dskins/ro2009/pageprint&containersrc=%5Bl%5Dcontainers/ro2009/simple. Last accessed May 31, 2014.
2. Deeb S, Motulsky A. Red-Green Color Vision Defects. 29 Sept 2011. http://www.ncbi.nlm.nih.gov/books/NBK1301/. Last accessed May 31, 2014.
3. Pacheco-Cutilla M, Edgar D. Acquired colour vision defects in glaucoma — their detection and clinical significance. Br J Ophthalmo. 1999. http://bjo.bmj.com/content/83/12/1396.full. Last accessed May 31, 2014.
4. Cole B. Assessment of inherited colour vision defects in clinical practice. 11 Apr 2007. http://onlinelibrary.wiley.com/doi/10.1111/j.1444-0938.2007.00135.x/full. Last accessed May 31, 2014.
5. Ivan DJ. Ophthalmology. Rayman’s Clinical Aviation Medicine 5th Ed. 2013; (235-292).
6. Pubmed Health. Color Blindness. 2011 June 1. http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0001997/. Last accessed July 26, 2014.
7. Hints on color vision testing. Department of Ophthalmology, Goteborg University. http://www.oft.gu.se/webdiagnos/color/color.html. Last accessed February 7, 2015.
8. The dyschromaptopsia of optic neuritis: a descriptive analysis of data from the optic neuritis treatment trial. Trans Am Opthalmol Society. 1995; 93:685-708. http://ncbi.nlm.nih.gov/pmc/articles/PMC1312075/. Last accessed on March 1, 2015.
9. Evaluation of Acquired Color Vision Deficiency in Glaucoma Using the Rabin Cone Contrast Test. Invest Ophthalmol Vis Sci. 2014 Aug 28;55(10):6686-90. http://www.ncbi.nlm.nih.gov/pubmed/25168899. Last accessed May 18, 2015.
368.55
Acquired color vision deficiencies
92283
Color vision examination
92083
Visual field examination
92250
Fundus photography
95930
Visual evoked potential
92275
Electroretinography
92225
Extended ophthalmoscopy
92015
Refraction
Plaquenil-induced toxic maculopathy
Primary optic atrophy
Diabetes-induced retinal ischemia
Occurrence
- 15% of the general population
- 20% – 30% of patients with open-angle glaucoma may have a general loss of color discrimination
Distribution
- Males and females are equally affected
Risk Factors
- Macular degeneration
- Diabetic retinopathy
- Multiple sclerosis
- Cataracts
- High-risk medications
- Toxic environmental exposure to certain chemicals




 Print | Share
Print | Share