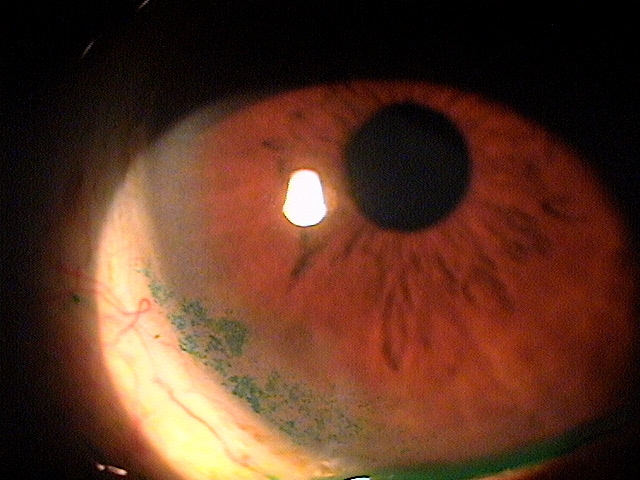
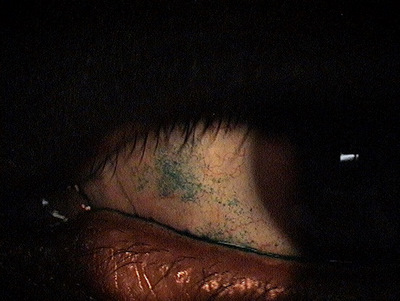
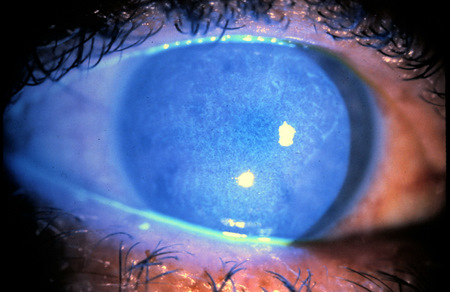
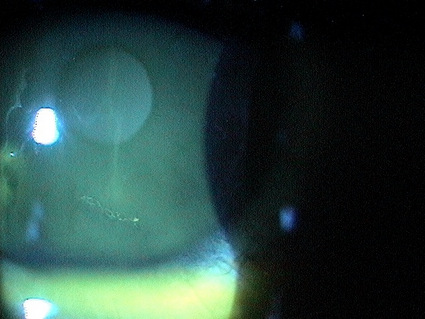
“Dry spots” form on the corneal
surface in dry eye syndrome
ICD-10 Diagnosis Codes:
H04.121–Dry eye syndrome, right lacrimal gland
H04.122–Dry eye syndrome, left lacrimal gland
H04.123–Dry eye syndrome, bilateral lacrimal glands
Title
Dry Eye Syndrome
Category
Disorders Of The Lacrimal System
Description
A disease of the surface of the eye that arises due to either decreased tear film production or increased tear film evaporation and results in symptoms of ocular irritation.
The modern model of dry eye syndrome describes a collection of disorders that interfere with the ability of the lacrimal apparatus to maintain a healthy tear film over the ocular surface. The common link between the various disorders is that they all end up with a loss of water from the tear film.
- The loss of water from the tear film increases its osmolarity above the normal limit of 311 mOsm/L
- The increase in tear film osmolarity is the link between changes in the lacrimal glands, changes in the eyelids, and disease of the ocular surface
 |
Ocular Surface Anatomy and Physiology
|
Dry eye syndrome evolves through a sequence of four milestones:
1. Loss of water from the tear film with an increase in tear film osmolarity
2. Decreased conjunctival goblet cell density and decreased corneal glycogen
3. Increased corneal epithelial desquamation
4. Destabilization of the cornea-tear interface
1st Milestone – Loss of water from the tear film with an increase in tear film osmolarity
The tear film is a balanced mixture of water, mucin, lipids, electrolytes, proteins, and immunoglobulins. When water is lost from a balanced tear film, it produces an imbalance that is characterized by an increase in tear film osmolarity. The osmolarity changes when water is lost from the tear film while solutes such as sodium and potassium are not. The first milestone may be accompanied by mild to moderate patient symptoms and no clinical signs. If left untreated, the disease is likely to progress.
2nd Milestone – Decreased conjunctival goblet cell density and decreased corneal glycogen
Conjunctival epithelial cells secrete transmembrane mucins that form the glycocalyx. The glycolcalyx is a glycoprotein (mucin) coating that covers the corneal and conjunctival epithelium. The function of the glycocalyx is to allow the tear film to bond to the surface of the eye. The conjunctiva also contains specialized goblet cells that secrete a gel-forming mucin that floats free in the tear film to help stabilize it after the blink. When tear film osmolarity is chronically elevated, goblet cells become damaged by the high sodium levels associated with high tear film osmolarity.
High tear film osmolarity also produces an osmotic gradient beween the tear film and the ocular surfce. The osmotic graient is an attempt by the tear film to replace some of the water that is being lost. The mechanism of the osmotic gradient pulls water from the conjunctival and corneal cells into the tear film. This pulling action of the gradient produces a type of osmotic shock that damages some of the cells. As the disease progresses, the level of damage increases. Eventually, enough cells are damaged to produce a clinically significant loss of the inter-cellular attachments between some of the conjunctival epithelial cells. As increasing numers of inter-cellular attachments are damaged, conjunctival epithelial cells begin to slough away at an abnormally high rate. This abnormal sloughing of epithelial cells is called conjunctival epithelial desquamation.
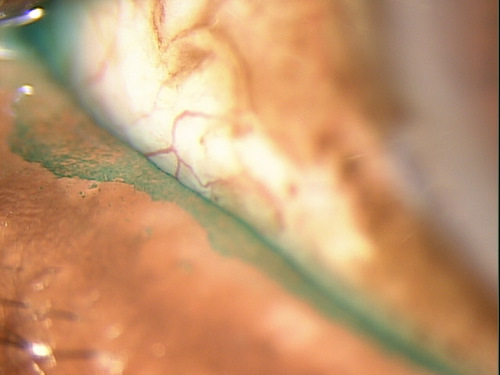
Conjunctival Epithelial Desquamation
|
 |
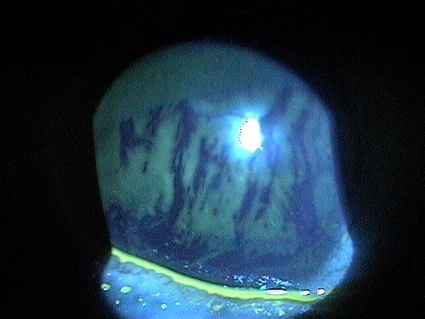
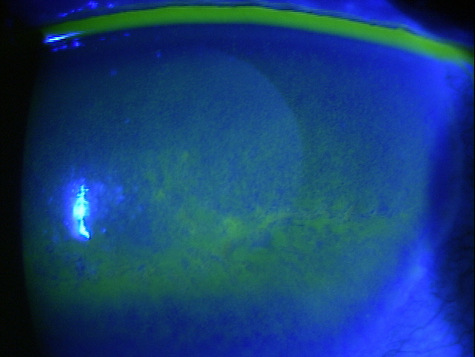
3rd Milestone – Increased corneal epithelial desquamation
Continued exposure to the osmotic gradient produced by high tear film osmolarity will eventualy damage the cornea. The osmotic shock that increases the rate of conjunctival epithelial desquamation eventually increases the rate of corneal epithelial desquamation. The result is also the same – immature corneal epithelial cells reaching the ocular surface without a glycoprotein surface coating.
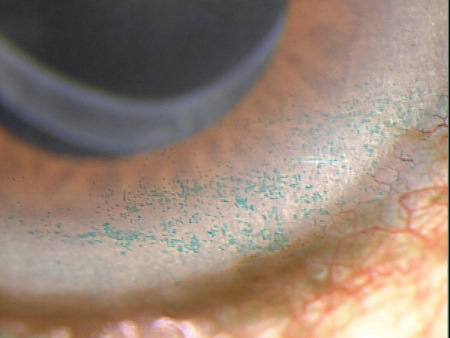 |
Corneal Epithelial Desquamation
|
|
Corneal Epithelial Desquamation
|
 |
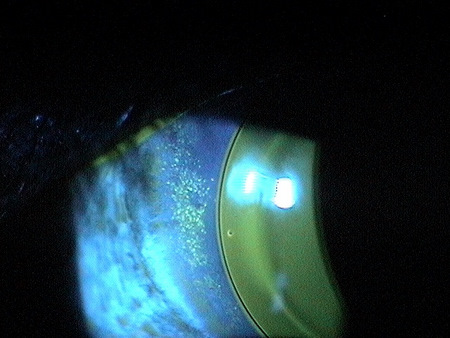
4th Milestone – Destabilization of the cornea-tear interface
The decrease in corneal glycogen precipitates the last milestone in the natural history of dry eye syndrome – destabilization of the cornea-tear interface secondary to the loss of epithelial microvilli. As changes in the corneal epithelial cell surface become more severe, surface glycoproteins are lost. The lost of these glycoproteins (primarily mucins) degrade the glycocalyx and further destabilize the cornea-tear interface.
|
 |
The main goal of the diagnostic evaluation in a patient with dry eye syndrome is to accomplish the following:
- To establish the diagnosis of dry eye syndrome
- To determine WHY there is a loss of water from the tear film
- To establish appropriate therapy
- To relieve discomfort
- To prevent complications
- To educate patients and involve them in managing their dry eye disease
To obtain the information required to determine a clinical diagnosis of dry eye syndrome and to prescribe a treatment plan, the following service components of a medical eye examination should be performed.
- Patient history
- General medical observation
- Adnexal examination
- External ocular examination with biomicroscopy
Patient History
Patients with dry eye syndrome may present with any of the following abnormal clinical symptoms:
- Dry eyes
- Itchy eye
- Burning eyes
- Scratchy eyes
- Stinging eye
- Watery eyes
- Light sensitivity
- Gritty sensations
- Eye pain
- Blurred vision
In addition to physiological conditions, dry eye syndrome-related symptoms can be worsened by exposure to environmental conditions such as wind, air conditioning, and temperature extremes. Activities that reduce blink rate (e.g., extended periods of reading, computer viewing, or driving) can produce more severe symptoms.
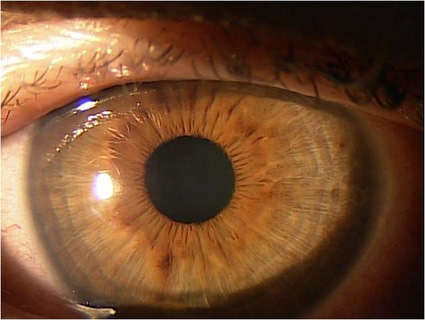
External Ocular Examination with Biomicroscopy
Patients with dry eye syndrome may present with abnormal clinical signs in any of the following anatomical areas:
- Tear film
- Eyelid
- Conjunctiva
- Cornea
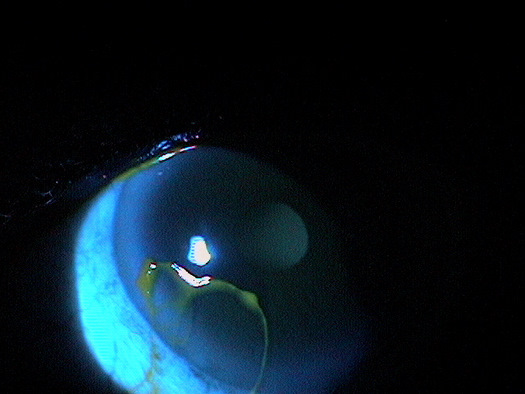 |
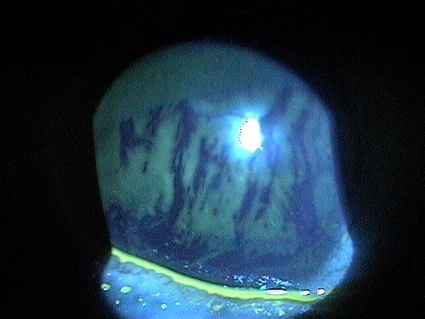
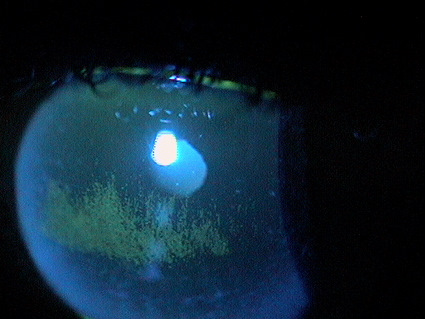
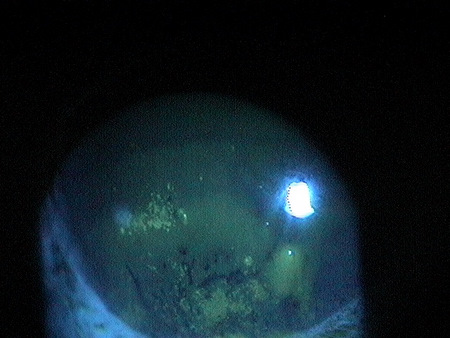
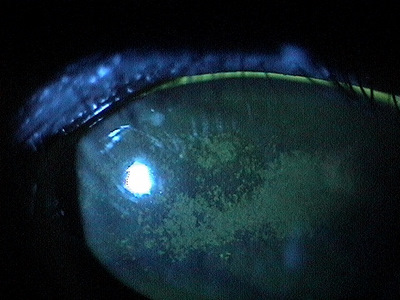
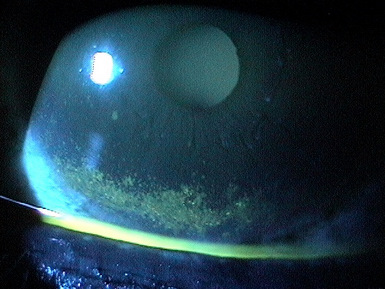
Clinical Appearance of the Tear Film
|
|
Clinical Appearance of the Tear Film
|
 |
|
 |
Clinical Appearance of the Tear Film
|
|
Clinical Appearance of the Tear Film
|
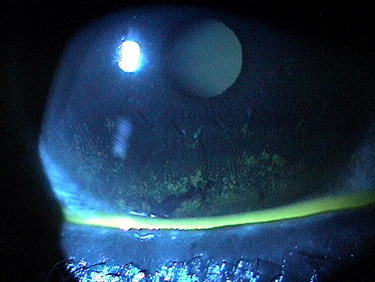 |
|
 |
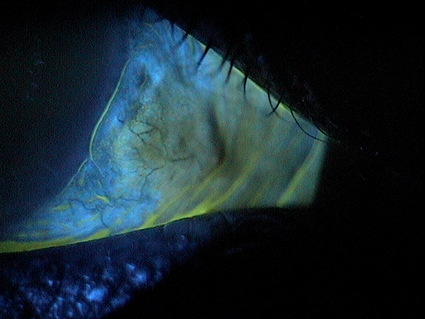
Clinical Appearance of the Eyelid
|
|
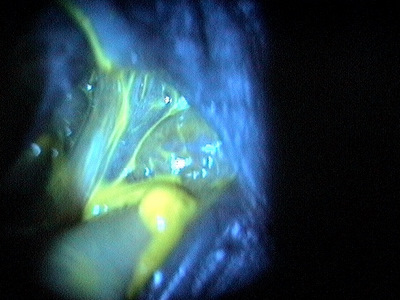
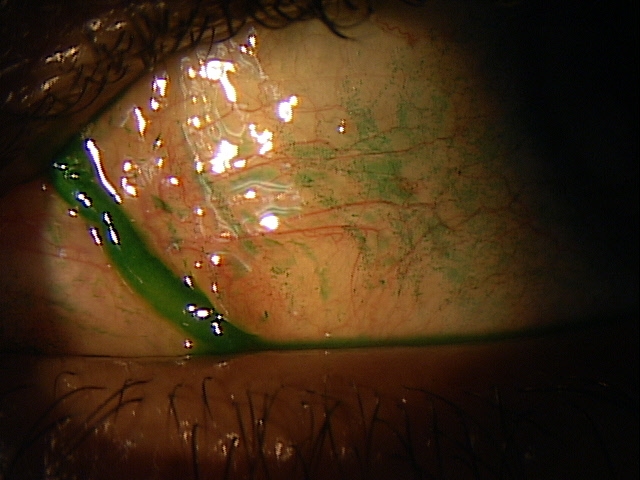
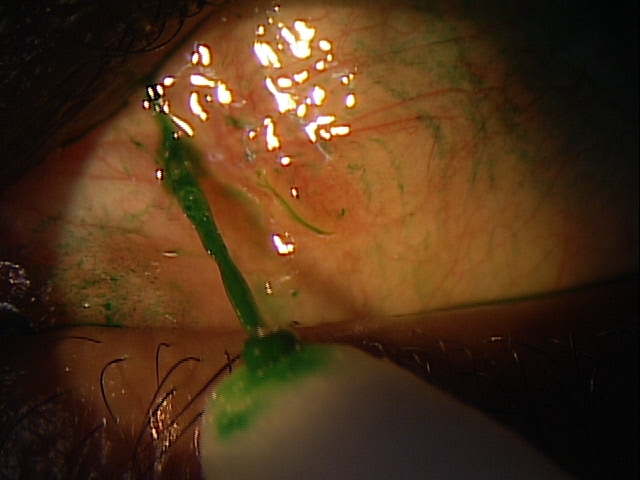
Clinical Appearance of the Conjunctiva
|
 |
|
 |
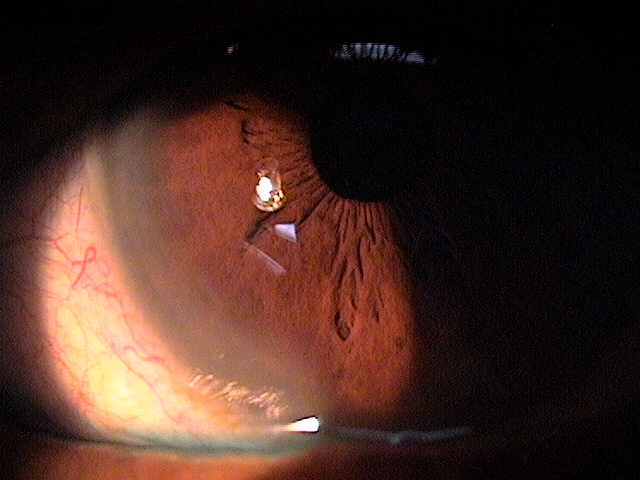
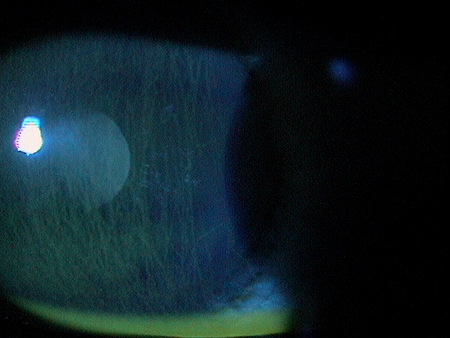
Clinical Appearance of the Cornea
|
According to the 2004 recommendations from the Delphi Panel, dry eye syndrome can also be classified by the stage of the disease.
| Dry Eye Severity Level | Clinical Signs and Symptoms |
| Level 1 – Mild | · Mild to moderate symptoms · No clinical signs · Mild to moderate conjunctival signs |
| Level 2 – Moderate | · Moderate to moderately-severe symptoms · Tear film abnormalities · Mild corneal punctate staining · Conjunctival staining · Visual blur, glare, photophobia |
| Level 3 – Moderately-severe | · Moderately-severe to severe symptoms · Marked corneal punctate staining · Central corneal staining · Filamentary keratitis |
| Level 4 – Severe | · Severe symptoms · Severe corneal staining · Corneal erosions · Conjunctival scarring |
In addition to disease staging, dry eye syndrome can be classified by etiology or clinical appearance.
 |
Etiology of decreased tear film volume
Presence of eyelid margin disease
Presence of clinically apparent inflammation
|
|
The muco-cutaneous junction is a line of squamous cells that runs along the entire length of the upper and lower eyelid margin |
This would include other diseases that present with a superficial punctate keratopathy or excess mucus accumulation in the tear film.
 |
Blepharitis
|
|
 |
Exposure Keratoconjunctivitis
|
|
 |
Chemical Burn
|
|
 |
Topical Drug Toxicity
|
|
 |
Contact Lens-Induced Superficial Punctate Keratopathy
|
|
 |
Retained Conjunctival Foreign Body
|
|
 |
Conjunctivitis
|
|
 |
Trichiasis
|
|
 |
Trauma
|
To follow best practices treatment guidelines, use the algorithm developed by Delphi Panel.
Level 1 – Mild Dry Eye Syndrome
- Patient counseling
- Preserved artificial tears
- Environmental management
- Allergy eye drops
- Increased water intake
- Use of hypoallergenic products
- If no improvement, add level 2
Level 2 – Moderate Dry Eye Syndrome
- Unpreserved artificial tears, gel, ointments
- Topical immunomodulators (e.g., Restatis Ophthalmic Emulsion)
- Topical steroids
- Secretagogues
- Nutritional support
- If no improvement, add level 3
Level 3 – Moderately-Severe Dry Eye Syndrome
- Oral tetracyclines
- Punctal occlusion
- Amniotic membrane therapy
- If no improvement, add level 4
Level 4 – Severe Dry Eye Syndrome
- Amniotic membrane therapy
- Systemic anti-inflammatory therapy
- Oral cyclosporine
- Moisture goggles
- Acetylcysteine
- Punctal cautery
- Eyelid surgery
 |
 |
In 2006, the Asclepius Panel enhanced the Delphi Panel’s recommendation for treating dry eye syndrome. Their recommendations was to prescribe steroids in conjunction with Restasis earlier in the natural history of the disease. Their recommendations include the following treatment guidelines:
Day 1 – Initiate treatment with Lotemax gel eye drops 2-4x per day; use artificial tears as needed
Day 14 – Reduce Lotemax gel to twice daily and discontinue over the next 2-4 weeks; begin Restasis twice daily
Day 60 – Continue with Restasis twice daily; use Lotemax up to 4x per day for breakthrough period
Day 180 – Monitor patient’s progress
1. Morris S. Management of the Chronic Dry Eye Patient. Optometric Management. 1 Apr 2006. http://www.optometricmanagement.com/articleviewer.aspx?articleID=71617. Last accessed August 15, 2014.
2. Legerton J. Schachet J. Look at the Whole Picture. RevOptom. 15 Feb 2007. http://www.revoptom.com/content/d/news_review/c/15509/. Last accessed August 15, 2014.
3. Gilbard J. Dry Eye Natural History, Diagnosis, and Treatment. Ophthalmology Management. 1 Nov 2003. http://www.ophthalmologymanagement.com/articleviewer.aspx?articleid=85952. Last accessed August 15, 2014.
4. Karpecki P. Osmolarity and Dry Eye. RevOptom. 15 Feb 2007. http://www.revoptom.com/content/d/cornea/c/15523/dnnprintmode/true/? skinsrc=%5Bl%5Dskins/ro2009/pageprint&containersrc=%5Bl%5Dcontainers/ro2009/simple. Last accessed August 15, 2014.
5. Karpecki P. Dry Eye: Which Test is Best? RevOptom 15 Feb 2005. http://www.dryeyezone.com/talk/showthread.php?49-Dry-Eye-Which-Test-is-Best. Last accessed January 22, 2015.
375.15
Tear film insufficiency, unspecified
68761
Punctal occlusion
92025
Coneal topography
92285
External ocular photography
92071
Bandage contact lens
65778
Amniotic membrane placement




 Print | Share
Print | Share