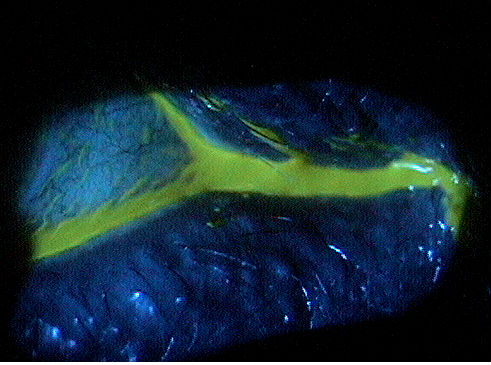
Abnormal tear film that overflows onto the
cheek is common sign of epiphora
secondary to reduced tear drainage
ICD-10 Diagnosis Codes:
H04.221–Epiphora due to insufficient drainage,right lacrimal gland
H04.222–Epiphora due to insufficient drainage,left lacrimal gland
H04.223–Epiphora due to insufficient drainage,bilateral lacrimal glands
Title
Epiphora Due to Insufficient Drainage
Category
Disorders Of The Lacrimal System
Description
Epiphora refers to watering due to obstruction in the lacrimal outflow pathway.
Watering of the eyes is a common symptom in many ocular diseases and conditions.
Epiphora is the term to describe watering that is associated obstruction in the lacrimal outflow pathway, rather than pseudoepiphora or hyperlacrimation, which refers to excessive watering due to reflex irritation of the corneal and conjunctival surface. In true epiphora, the cause of the watering must be differentiated between anatomical and functional lacrimal pathway obstruction.
Anatomical Lacrimal Pathway Obstruction
- Punctal stenosis
- Canalicular stenosis
Lacrimal Pump Mechanism Failure
- Punctal ectropion
- Eyelid laxity
- Facial palsy
The Dry Eye Workshop Report (2007) stressed the importance of the Lacrimal Functional Unit in maintaining and preserving a healthy ocular surface. The Lacrimal Functional Unit maintains ocular surface homeostasis by regulating tear flow and consistes of the following:
- Cornea
- Conjunctiva
- Lacrimal glands
- Meibomian glands
The neural response of the Lacrimal Functional Unit is initiated by activation of the afferent sensory nerves in the cornea and conjunctiva that stimulate efferent parasympathetic and sympathetic nerves that innervate the accessory and main lacrimal glands.
The lacrimal apparatus is a network of anatomical structures, appendages, ducts and glands that secretes the pre-corneal tear film and then drains the tears from the surface of the eye. The outflow of tears is accomplished by the lacrimal drainage system and it includes the following anatomical structures:
- Eyelid margin
- Lacrimal punctum
- Lacrimal canaliculus
- Lacrimal sac
- Nasolacrimal duct
Abnormal tearing is described as acute or chronic. Acute epiphora is usually secondary to one of the following irritative ocular conditions:
- Eyelid malposition
- Trichiasis
- Corneal foreign bodies
- Allergic conjunctivitis
- Dry eye syndrome
- Environmental factors
- Emotional stress
- Sleep deprivation
Structural Damage to the Eye
- xxx
Functional Damage to the Eye
- Decreased vision secondary to frequent blinking and eye rubbing
The main goal of the diagnostic examination in a patient with epiphora is to accomplish the following:
- Differentiate epiphora from pseudoepiphora by performing a lacrimal apparatus evaluation for likely nonobstructive causes of the watering
- Differentiate obstructive causes of epiphora from nonobstructive causes
- Find the site of the obstruction in cases of obstructive epiphora
Patient History
- xxx
External Ocular Examination with Biomicroscopy
When examining the lacrimal drainage system, note any evidence of eyelid malposition and evaluate the dynamics of eyelid closure. Normally, the eyelid margins will be in close proximity and the puncta are apposed when the eyelids are closed. The normal punctum is in contact with the globe and is not usually visible without pulling the lower eyelid downwards and the upper eyelid upwards.
Abnormal findings involving the punctum include malposition, stenosis or obstruction. The lower canaliculus and the lacrimal sac should be palpated and compressed. Abnormal findings include any pain or tenderness during the examination or any reflux of pus or mucopurulent material.
Epiphora is classified based on its cause – anatomical or functional.
Obstructive Causes
- Inflammatory processes
- Infectious process
- Mechanical processes
Nonobstructive Cause
- Punctal ectropion
- Eyelid laxity
- Facial palsy
Pseudoepiphora
- Also known as hyperlacrimation (excessive watering due to reflex irritation of the corneal and conjunctival surface)
- Dry eye syndrome
- Foreign bodies
- Corneal or conjunctival abrasions
- Ocular allergies
The information currently being updated. Please check back later.
1. Sowka J, Kabat A. Epiphora Epiphany. RevOptom. 16 Jan 2009. 146:01. http://www.reviewofoptometry.com/content/d/retina_quiz/c/14929/dnnprintmode/true/?skinsrc=%5Bl%5Dskins/ro2009/pageprint&containersrc=%5Bl%5Dcontainers/ro2009/simple. Last accessed November 1, 2015.
2. Freedman J, Markert M, Cohen A. Primary and Secondary Lacrimal Canaliculitis: A Review of Literature. Survey of Ophthalmology, 56:4. July-Aug 2011. http://www.ncbi.nlm.nih.gov/pubmed/21620429. Last accessed November 1, 2015.
3. Camara J. Obstruction Nasolacrimal Duct. Medscape/EMedicine. http://emedicine.medscape.com/article/1210141-overview#showall. Last accessed November 1, 2015.
4. Townsend W. Implications of the Lacrimal Functional Unit. Contact Lens Spectrum. Oct 2015. http://www.clspectrum.com/articleviewer.aspx?articleID=113331. Last accessed November 1, 2015.
375.22
Epiphora due to insufficient drainage
92285
External ocular photography
68801
Dilation of the lacrimal puctum
68840
Probing of the lacrimal canaliculus
Occurrence
- This condition is relatively common, but the exact frequency is not known.
Distribution
- More prevalent in women
- No predilection to race has been established
- Most commonly diagnosed in middle-aged women
Risk Factors
- Allergies
- Eye injury
- An eye infection
- Loose eyelids
- Weakness of facial muscles or nerves (due to stroke or other medical conditions)
- Tumors
- Environmental factors
- Emotional stress
- Sleep deprivation




 Print | Share
Print | Share