Case Report ID: 6
Title:
Vitreomacular Traction Syndrome
Category:
Description:
Vitreomacular traction syndrome is a type of traction maculopathy. It is thought to occur when the posterior vitreous separates from the retina; but, a persistent vitreal attachment remains at the macula. The vitreal attachment can produce a localized traction that results in a distortion of the macular anatomy and results in metamorphopsia or decreased central visual acuity.
Case Report
- A 60-year-old black woman presents with a chief complaint of decreased vision
- Case history describes a non-specific subjective decrease in vision over the past two months
- Previous eye examination was 20 months earlier with 20/20 visual acuity in each eye
- The patient wore prescription eyeglasses full-time and wanted to know if new eyeglasses would improve her vision
Conclusion
Vitreomacular traction syndrome is frequently undiagnosed or misdiagnosed because of a lack of familiarity with this condition. This case demonstrates the importance of investigating a patient’s vague visual complaints and the importance of simple tests such as an Amsler grid in the early diagnosis of macular disease.
If left untreated, vitreomacular traction syndrome can result in chronic macular edema, vascular incompetence or a full-thickness macular hole.
History of Present Illness
- Associated Signs and Symptoms: none
- Location: vision is worse in the left eye
- Duration: past 3-4 months
- Quality: “I just can’t see right”
- Context: decreased vision is more noticeable when reading
- Severity: mild
- Timing: vision seems to be getting worse over time
- Modifiers: none
Review of Systems
The patient reported joint pain, joint stiffness and swelling. All other medical history was unremarkable.
Past, Family and Social History
Family history was significant for cancer, heart disease, arthritis and stroke.
Best Corrected Distance Visual Acuity
- 20/30 in the right eye
- 20/40 in the left eye
Normal Examination Findings
- Mental status
- General medical observation
- Pupils
- Gross visual fields
- Basic sensorimotor examination
- External examination
- Adnexal examination
Intraocular Pressure Measurements
- 19 mm Hg in the right eye
- 17 mm Hg in the left eye
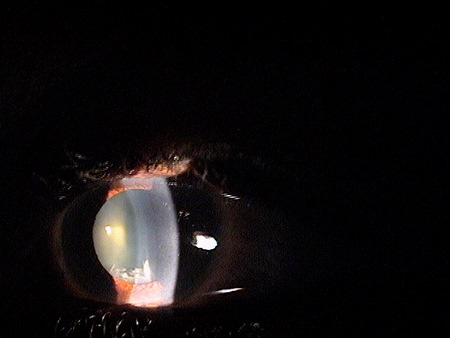
External Ocular Examination with Biomicroscopy
- Crystalline lenses revealed a moderate loss of transparency in both eyes – worse OS
- Cortical spoking and clouding seen with direct illumination slit-lamp technique
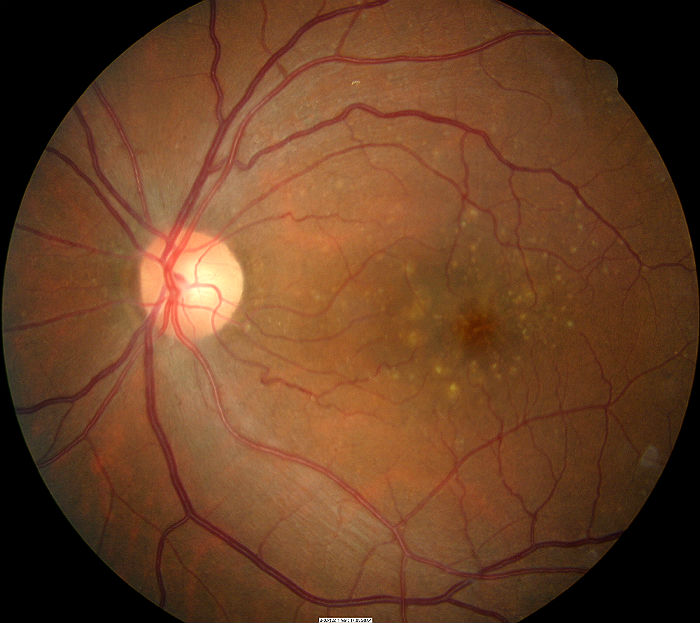
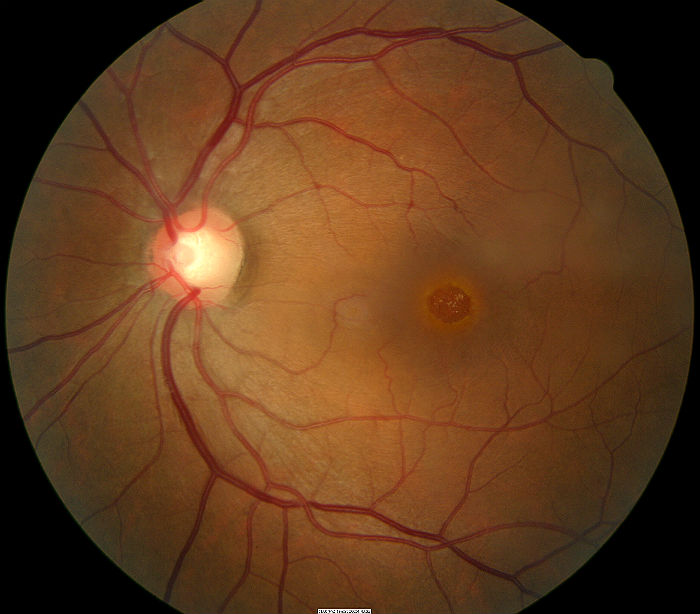
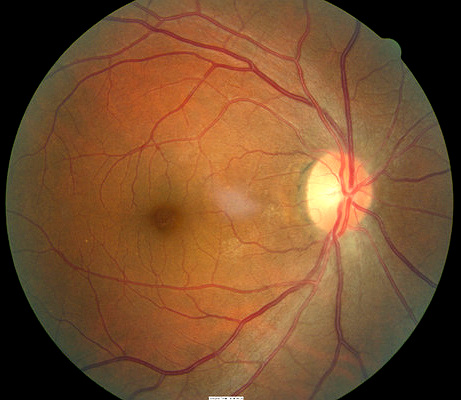
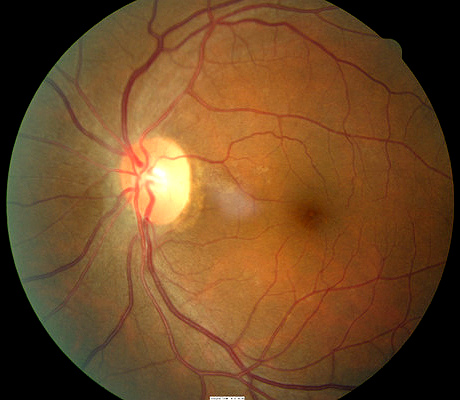
Ophthalmoscopy
Any of the following abnormal retinal signs may be present in vitreomacular traction syndrome:
- Pigmentary disorganization in the macula
- Loss of the foveal reflex
- Loss of the foveal depression
- Localized elevation of the macula
- Retinal straie secondary to traction
- Chronic cystoid macular edema
 |
 |
Clinical Diagnosis
Clinical diagnoses are determined based on the knowledge obtained from the patient’s medical history and from the results of the eye examination alone, without the benefit of diagnostic tests or procedures.
The patient’s clinical diagnoses are cataract and early age-related macular degeneration based on the following clinical findings:
- Abnormal appearance of the crystalline lenses in both eyes
- Mild pigmentary disruption in the macula of both eyes
- Loss of the foveal reflex in the left eye (compared to previous examination)
- Loss of best corrected visual acuity in both eyes (compared to previous examination)
Treatment Plan
To gather the clinical information required to treat cataracts and macular degeneration, a diagnostic and treatment program is initiated.
- Determination of different types of diagnoses
- Selection of one or more treatment options
Differential Diagnoses
Several macular diseases have clinical signs that mimic the appearance of vitreomacular traction syndrome.
Most patients with vitreomacular traction do not experience significant vision loss (usually less than 20/50, although some will progress to more significant central vision loss). Vitreomacular traction typically has an asymmetric presentation with the fellow eye rarely showing clinical changes. The pathogenesis and risk factors for vitreomacular traction syndrome are not well established.
While the risk of progression to more severe disruption of foveal function or progression to a macular hole exist, it is low. Serial OCT analysis documents that many presentations spontaneously resolve. The resultant visual function is often good, sometimes with persistent metamorphopsia. Resolved vitreomacular traction syndrome is a common cause of soft 20/20 acuity or persistent complaints regarding quality of vision with normal Snellen acuity. The clinical appearance of the macula may seem completely normal after spontaneous resolution, but more often there are subtle changes in the anatomy that indicate prior physical alteration of the tissue.
Ordering Diagnostic Tests
When the fundus appearance, visual acuity or qualitative aspects of vision are abnormal, the following diagnostic tests can help determine the presence of vitreomacular traction syndrome:
- Amsler grid
- Retinal laser scan with time-domain or spectral-domain OCT
- Fluorescein angiography
- Fundus photography
- Central (10-2) visual fields
- B-scan ultrasound
- Electroretinogram
The decision to order and perform additional diagnostic testing is totally based on the concept of medical necessity which can only be determined by the examining optometrist or ophthalmologist.
Refraction
- Measuring visual acuity is a method of evaluating functional vision loss
- Vitreomacular traction can produce central visual field defects which result in a loss of visual acuity
- There was no improvement in the left eye’s visual acuity after a subjective refraction was performed
- 20/25 distance visual acuity in the right eye
- 20/40 distance visual acuity in the left eye
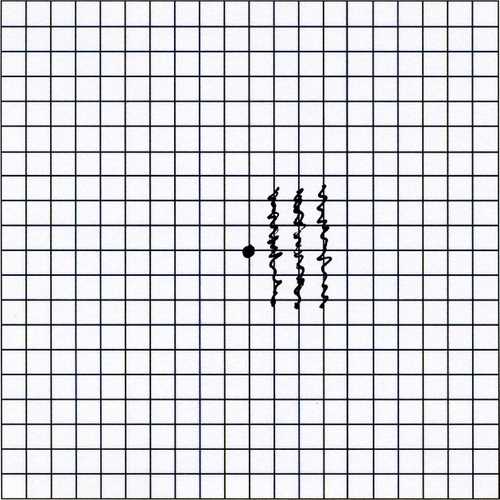
Amsler Grid
Amsler grid testing is used to evaluate the 10 degrees of visual field surrounding fixation. The subjective test allows the patient to report visual distortions which would support any clinical findings regarding macular involvement. These visual distortions are called metamorphopsia and are directly related to a compromise in the macular structure.
Amsler Grid Test Procedure
The Amsler grid is divided into four quadrants with a central fixation dot.
- It is held roughly 30 cm from the patient with one eye occluded
- The patient is instructed to fixate on the dot and subjectively report any distortions such as wavy lines, thickened lines, or any missing areas on the grid
Right Eye
- Non-specific distortion in the superior nasal corner of the grid
Left Eye
- Metamorphopsia adjacent to the fixation point
- Increased thickness of the paracentral grid lines
- Increased thickness of the central fixation dot
Both Eyes
- Clinically significant asymmetry
- Test results correlate with OCT test results
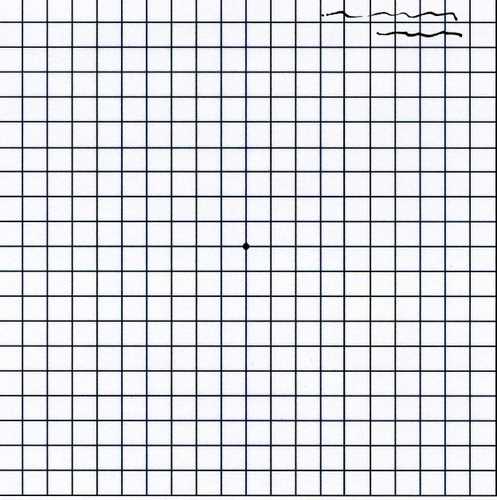 |
 |
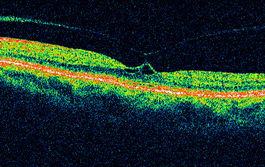
Retinal Laser Scan — Macula
- Measuring the average retinal thickness with detailed analysis of retinal structure in the macula provides an overall assessment of macular health
- The procedure can be accomplished by using the Stratus OCT manufactured by Carl Zeiss Meditec or other retinal scanning lasers
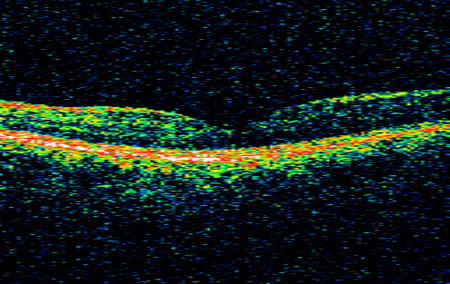 |
Right Eye
|
|
Left Eye
|
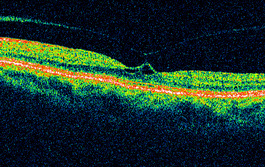 |
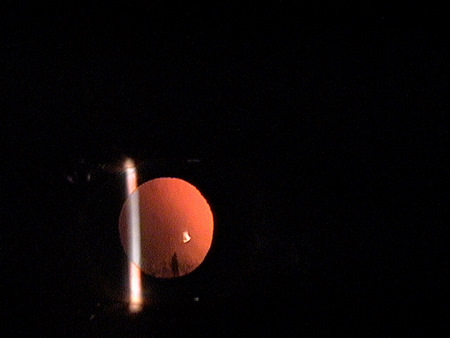
B-Scan Ultrasound
B-scan ultrasound can be used to demonstrate the total peripheral detachment of the posterior vitreous face as well as detachment from the optic nerve. Only the macular-foveal attachment will be visible in the ultrasound. Although often not as clear a picture as seen with OCT technology, the ability to visualize the posterior vitreous face in a more wide field view can be beneficial and can assist in making the differentiation of a total from a partial vitreous detachment.
Fluorescein Angiography
Fluorescein leakage around sites of vitreous detachment can show the usually subtle damage to the surface vessels. It may also be beneficial in differentially diagnosis of other potential macular disorders.
Central Visual Field
Central field visual testing can assist in differentiating acuity loss related to retinal pathology from acuity loss related to corneal or lens opacification. Mild to moderate corneal or lenticular opacification will not significantly effect threshold values in a 10-2 visual field.
Threshold values can be used to estimate potential acuity if the cornea or lenticular opacity is removed.
- 32dB or higher – expect normal Snellen acuity
- High teens to low thirties – expect one or two lines loss of Snelen acuity
- Mid to high teens – expect three to four lines loss of Snellen acuity
- Low to mid teens – expect five to eight lines loss of Snellen acuity
In this case, the average 10-2 threshold was around 30dB in each eye which would correspond to only a line of acuity loss, two lines at most. It would appear that the majority of the subjective vision loss is related to the retinal pathology but the cataract in the left eye was also a contributing factor.
After reviewing the diagnostic test results, the clinical diagnosis of age-related macular degeneration was changed to a more substantiated physical diagnosis of vitreomacular traction syndrome in the left eye and early cataract in both eyes.
According to Current Procedural Terminology, when eye doctors perform ophthalmological examinations, the complexity of medical decision-making is not separated from the examining techniques used. As a guideline to assist eye doctors in enhancing their medical decision-making skills, consider that the complexity of medical decision-making involves three components.
The first component concerns the number of possible diagnoses and treatment options that must be considered. Determination of the diagnosis of vitreomacular traction syndrome involves the determination of structural damage to the vitreous and retina with associated functional loss of vision. There are many other potential causes for structural alteration in the macula so the differential diagnosis shows moderate complexity.
The second component concerns the amount and complexity of medical records and diagnostic tests that have to be obtained, reviewed and analyzed. In addition to an eye examination, this visit required the review and analysis of a subjective refraction, a retinal laser scan, and a threshold visual field examination.
Third, the complexity of medical decision-making is affected by the risk of significant complications and/or morbidity associated with vitreo-macular traction and the risks involved in any treatment options. This patient’s retinal condition was classified as a significant problem where the risk of significant central vision loss without treatment was possible. In addition, the treatment plan will involve continued monitoring of the retinal condition.
Non-Surgical Treatment Guidelines
Observation for spontaneous resolution is the most common treatment option for mild vitreomacular traction syndrome. Non-surgical treatment involves close monitoring of the condition both on a home and clinical basis to maximize the earliest detection of further vision deterioration. This is best accomplished by home Amsler grid testing and repeat ophthlalmoscopic evaluations including OCT analysis.
Surgical Treatment Guidelines
In moderate-to-advanced cases, surgical vitrectomy is often successful in restoring normal or near normal acuity levels. More recently, retinal surgeons are using proteolytic enzymes to dissolve the vitreous attachments. Jetrea (ocriplasmin) is the first such intravitreal agent for this purpose.
Most retinal specialists use the following criteria to determine the need for surgical treatment:
- 20/50 – 20/70 or worse visual acuity
- Declining visual acuity
- Patients with an intolerance for visual distortions
Clinical signs of any of the following:
- Cystoid macular edema
- Vascular incompetence
- Impending macular hole
Since a significant number of vitreomacular traction cases resolve spontaneously, clinicians should be slow to recommend invasive surgery until Snellen acuity loss exceeds 20/50 or structural retinal changes point to a significant risk of macular hole formation. Retinal surgeons establish individual thresholds related to the decision to perform surgery, typically strongly based on Snellen acuity. Eye doctors should familiarize themselves with these thresholds so referral options can be made only at the appropriate time.
Treatment Program
Observation for Spontaneous Resolution — The patient was counseled regarding the condition and the need for home monitoring with Amsler grid. Any changes in acuity or the Amsler grid should be reported immediately. Because this was the initial diagnosis of vitreomacular traction syndrome, the next visit was scheduled for 1 month.
Discussion
Traction on the macular tissue produces gradual, anatomic and functional deterioration in proportion to traction forces and their duration of action. Macular traction is tangential to the macular surface in disorders such as cellophane maculopathy, macular pucker and macular hole. Macular traction is anterior/posterior to the macular surface in vitreomacular traction syndrome. Traction maculopathies are estimated to occur in 6.4% of the population over age 50.
This case demonstrates management of a common condition that eye doctors can easily become uncomfortable with. For example, vitreomacular adhesion can lead to vitreomacular syndrome. Complications include loss of vision secondary to retinal thickening, foveal cysts, vascular incompetence, cystoid macular edema and macular hole. In addition, cataract surgery increases the complications from vitreomacular traction syndrome.
Even though the microscopic retinal appearance can often be disturbing, the patient may have near normal acuity. If the visual acuity declines, referral to a retinal specialist may be warranted. Because of the risk of surgical intervention combined with the nature of the condition to spontaneously resolve, referrals for surgical intervention should be conservatively considered.
Based on patient history, the nature of the presenting problem, and my own clinical judgement this patient needed an evaluation of the complete visual system.
- Perform the eye examination that is medically necessary
- Provide the diagnostic tests or services that are medically necessary
- Properly document the services provided
- Code from the documentation
- Report the services to the payor
| Diagnosis Code | Procedure Code | Modifier | Quantity | Payor | Amount Allowed |
| H35.342 - Macular cyst, hole, or pseudohole, left eye | 92014 - Medical eye examination | 1 | Aetna | 89.51 | |
| H35.342 - Macular cyst, hole, or pseudohole, left eye | 92015 - Refraction | 1 | Aetna | 20.74 | |
| H35.342 - Macular cyst, hole, or pseudohole, left eye | 92133 - Retinal laser scan | 1 | Aetna | 34.38 | |
| H35.342 - Macular cyst, hole, or pseudohole, left eye | 92083 - Visual field examination | 1 | Aetna | 72.00 | |
| Total | $216.63 |
H35.342
Macular cyst, hole, or pseudohole
left eye
362.54
Macular cyst
92015
Refraction
92083
Visual field examination
92250
Fundus photography
92134
Retinal laser scan
92275
Electroretinography
92283
Color vision examination




 Print | Share
Print | Share