Title:
Category:
Description:
Optic neuritis is second only to glaucoma as the most common acquired disorder of the optic nerve in patients under the age of 50. It usually presents as a unilateral inflammation of the optic nerve and it is commonly associated with the following conditions:
- Autoimmune disorders (multiple sclerosis, rheumatoid, lupus)
- Infections (viral, tuberculosis, toxoplasmosis, syphilis, mumps, measles)
- Diabetes
- Granulomatous diseases (sarcoidosis, cat scratch)
- Idiopathic Case Report
Case Report
- A 38-year-old black female presents with complaints of dizzy spells described as “spinning”
- The initial episode was 2 months ago which was accompanied by blurred vision in the right periphery, lasting 1 day
- A second episode occurred 2 weeks ago which she awakened with dizziness and then had vomiting
- She had a viral infection with cough 3 days later after the second episode
- Both episodes of dizziness lasted approximately 10 minutes
- Patient states she saw visual scotomas and halos in the daytime light with the last episode while driving
- Temporal history revealed an eye examination performed 14 months earlier with no abnormal findings
- The patient wore plano tinted contact lenses and wanted to get a new supply of lenses
Conclusion
Some of the clinical signs of optic neuritis, like that associated with multiple sclerosis, include sudden onset of unilateral vision loss associated with retro-orbital pain that is aggravated by eye movement. With multiple sclerosis, decreased vision following exercise, hot shower or bath or activities that elevate body temperature can also occur (Uhthoff’s Phenomenon). Common symptoms patients report are tender or sore eyes. There can be a loss of color vision and contrast sensitivity. In addition, there may be an afferent pupillary defect and optic disc hyperemia or optic disc swelling (optic papillitis).
History of Present Illness
- Associated Signs and Symptoms: intermittent pain
- Location: arms and legs
- Duration: many years
- Quality: tingling pain
- Context: approximately 20 episodes of pain over the past 12 months
- Severity: pain is moderate-to-severe
- Timing: seems to be getting worse, episodes last for several hours
- Modifiers: Pain is relieved by Hydrocodone as prescribed by her primary care physician. Pain may occur to any area of arms or legs and she is not aware of any specific triggers. Pain is improved with exercise.
Review of Systems
Patient reports numbness, tingling, headaches, and dizziness but reports no bladder symptoms, no bowel symptoms, no confusion, no memory loss, no speech disorder, no convulsions, no syncope, no blackouts, no weakness, no muscle twitching, no muscle cramps, no vertigo, no loss of hearing, no tinnitus, no imbalance or falling, no difficulty with gait or walking, no back pain, no neck pain, no double vision, no photophobia, and no vision loss.
Past, Family and Social History
Patient states she has occasional mild headaches. She denies any big headaches. She is taking birth control pills and has menses every 3 months. She denies any history of seizures and states her memory is good.
Uncorrected Distance Visual Acuity
- 20/20 in the right eye
- 20/20 in the left eye
Normal Examination Findings
- Mental status
- Pupils
- Basic sensorimotor examination
- External examination
- Adnexal examination
- External ocular examination with biomicroscopy
- Ophthalmoscopy
Intraocular Pressure Measurements
- 14 mm Hg in the right eye
- 12 mm Hg in the left eye
General Medical Observation
- Mild hand tremor, bilaterally
Gross Visual Fields
- There was a slight hemianopsia on the right side
Clinical Diagnosis
The clinical diagnosis is a determination based on the knowledge obtained from the patient’s medical history and from the results of the eye examination alone, without the benefit of diagnostic tests or procedures.
The patient’s clinical diagnosis is subjective visual disturbances with a probable neurologic etiology:
Patient symptoms included all the following:
- Numbness
- Tingling
- Headaches
- Dizziness
- Intermittent blurred vision
- Mild hand tremor
Treatment Plan
To gather the information required to diagnose the etiology of the visual disturbances, a diagnostic and treatment program is initiated.
- Determination of different types of diagnoses
- Selection of one or more treatment options
Differential Diagnoses
The differential diagnoses that need to be identified and excluded include any conditions that produce subjective visual disturbances with associated neurologic signs in young patients:
-
Multiple sclerosis
-
Arteritis
-
Vitamin D deficiency
Multiple sclerosis is a common demyelinating disorder of the central nervous system. It affects more than 350,000 people in the United States and the prevalence is increasing. Almost half of patients with multiple sclerosis present with ocular findings as the initial manifestation of the disease.
Ordering Diagnostic Tests
When additional clinical information is needed to complete the differential diagnostic process, diagnostic tests and procedures are ordered. The performance of these tests and procedures leads to the completion of the differential diagnostic process while simultaneously initiating the treatment program. Based on the clinical diagnosis of visual field defect secondary to presumed multiple sclerosis, the following diagnostic tests and procedures could be considered at the conclusion of the eye examination.
- Refraction
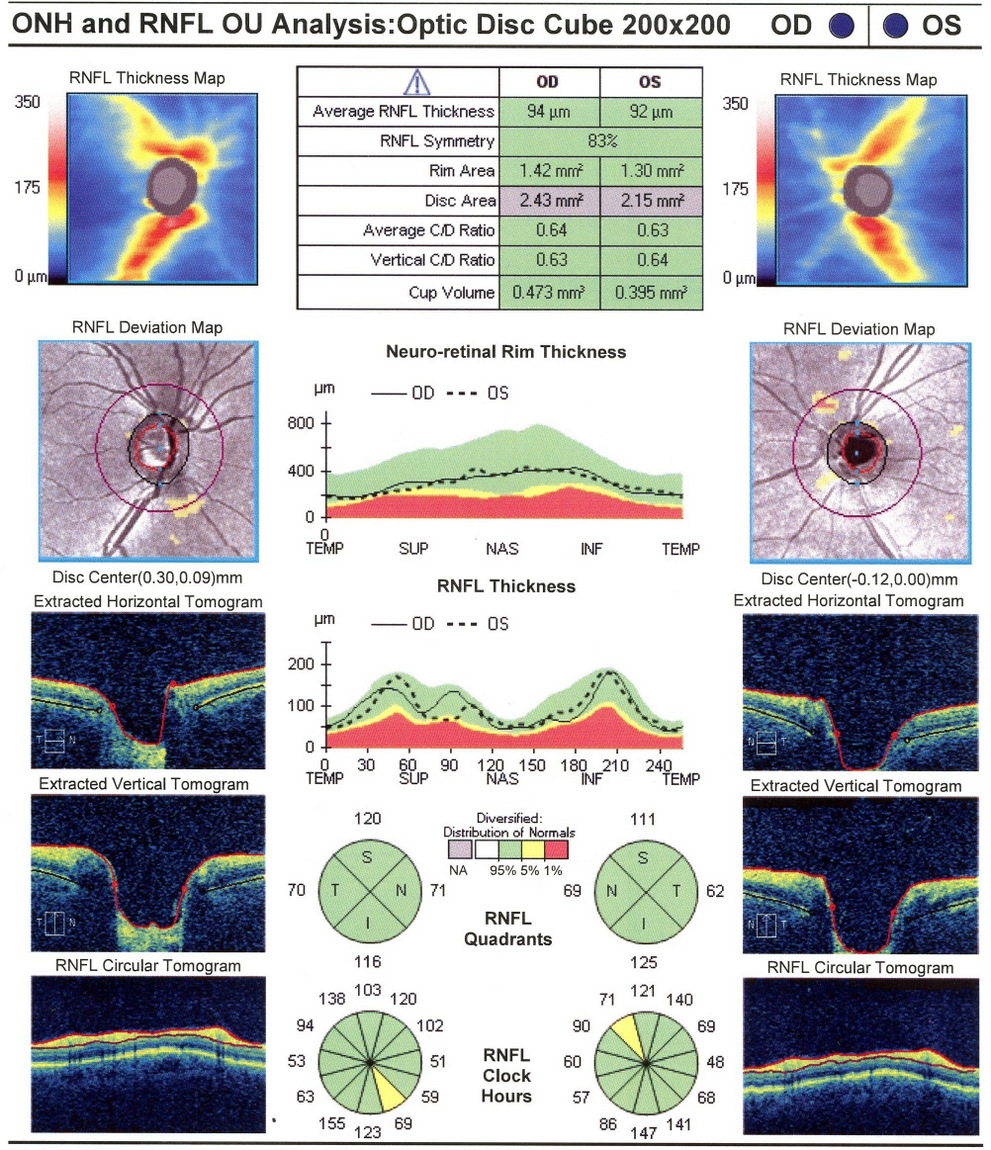
- Retinal nerve fiber layer scan
- Visual field examination
- Extended color vision examination
- Visual evoked potentials
- MRI of the brain with and without contrast
The decision to order and perform additional testing is totally based on the concept of medical necessity which can only be determined by the examining optometrist or ophthalmologist.
Refraction
- Measuring visual acuity is a method of evaluating functional vision loss
- This patient’s visual acuity was normal
Retinal Laser Scan — Nerve Fiber Layer
- Topographical analysis of the optic nerve provides an overall assessment of optic nerve anatomy and health
- The procedure can be accomplished by using the CIRRUS OCT manufactured by Carl Zeiss Meditec or other scanning lasers
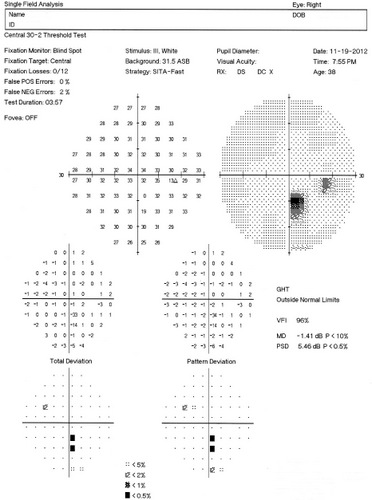
Visual Field Examination
- Automated threshold perimeters measure the visual field by plotting the threshold luminance value of the patient in various locations in the visual field
- The luminance of the light stimulus is represented by non-specific units of measurement called decibels (dB)
Optic neuritis typically produces central visual field, although patients in the Optic Neuritis Treatment Trial presented with visual field defects in varying locations and severity. In Tranquair’s “Hill of Vision” concept, loss of retinal sensitivity represents a reduction in the height of the hill. Optic neuritis associated with multiple sclerosis is most likely to produce a reduction in the peak of the hill of vision (central defects).
 |
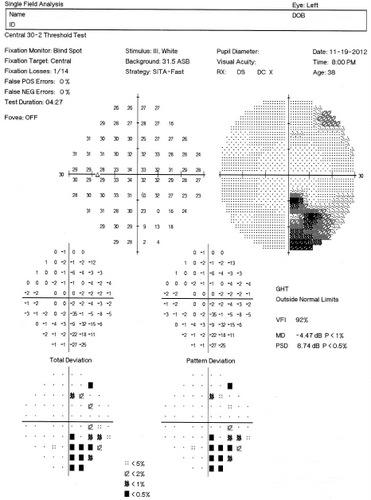 |
Automated threshold perimeters characterize specific parameters of the overall visual field status by the use of numbers called Global Indices. Two of the indices, Mean Deviation (MD) and Pattern Standard Deviation (PSD), express the raw data generated by the instrument.
A visual field defect can be classified as mild, moderate or advanced based upon an abnormal Mean Deviation.
- Mild visual field defect = 0 through -5.99 dB
- Moderate visual field defect = -6.00 dB through -11.99 dB
- Advanced visual field defect = anything above -12.00 dB
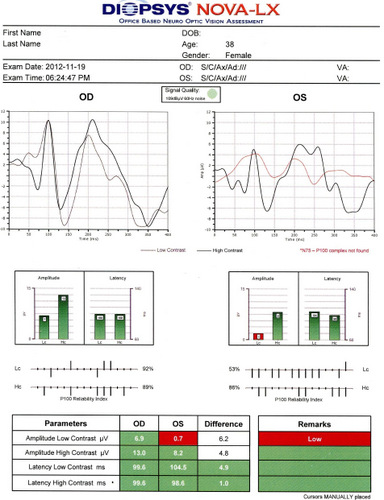
The Pattern Standard Deviation is a measure of focal loss of visual field taking into account any generalized depression in the hill of vision. Some feel it is more diagnostic than the Mean Deviation in demonstrating specific diagnoses for field loss – the higher the PSD, the more likely the patient has disease. Others feel the high degree of data manipulation contaminates the PSD value. In this patient, the PSD is significantly higher in the left eye and clinically significant asymmetry is diagnostic for optic nerve disease.
Right Eye
- Very mild loss of retinal sensitivity
- Paracentral scotoma; inferiorly
Left Eye
- Mild loss of retinal sensitivity
- Dense central scotoma; inferonasal quadrant
Both Eyes
- Clinically significant asymmetry
- Central visual field defect frequently found in unresolved optic neuritis
- Visual field test results correlate with visual evoked potential test results
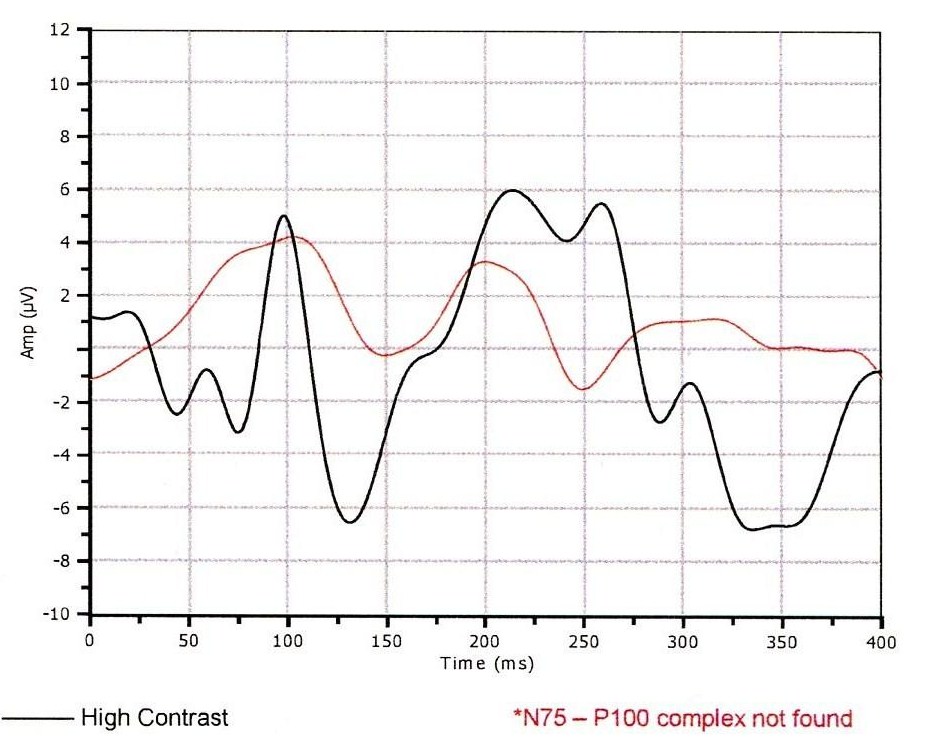
Visual Evoked Potential Testing
- Visual evoked potential testing evaluates the integrity of the afferent visual sensory system
- The procedure can be accomplished by using the NOVA-LX Testing Device manufactured by DIOPSYS
- In optic nerve disease, the amplitude of the VEP response is decreased and the P100 peak time is delayed compared to the other eye
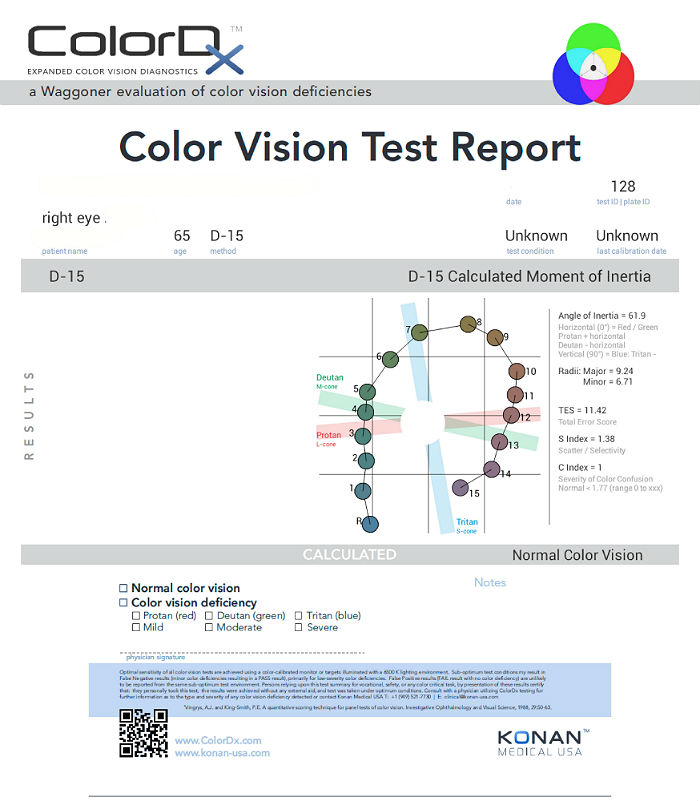
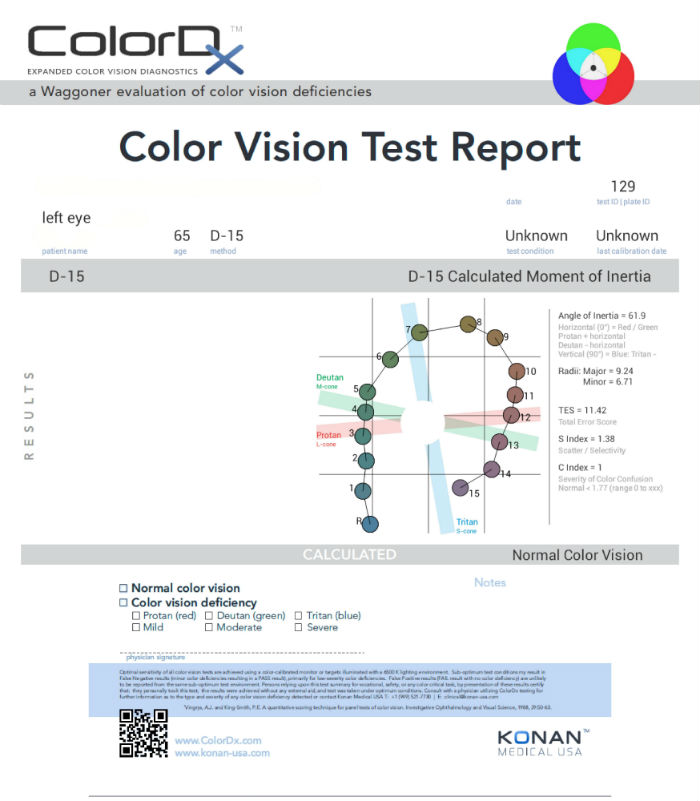
Color Vision Examination
An extended color vision examination measures the combined function of the retina, the optic nerve and the intracranial visual pathway and is used clinically to detect or monitor color vision loss due to disease at any of these locations. Extended color vision testing divides people into two groups.
- The first group consists of people with normal color vision and slight color deficiency
- The second group consists of people with moderate or severe color deficiency
One of the most common tests performed in clinical practice is the Farnsworth D15. When performed on Konan Medical’s ColorDx software, the test is presented as fifteen colored bars and one fixed bar on an Android tablet. The hue of each bar has been chosen so that the adjacent bars have approximately equal hue differences. When the bars are arranged in order, they form a hue circle. As a result, errors in hue discrimination can be made across the hue circle.
Patients with normal color vision usually make no error but may make one or two minor transposition errors, as do those with mild color vision deficiency. Patients with more advanced color deficiency make some or more of the following errors:
- They place colors that lie on the opposite side of the hue circle next to colors that lie on their confusion locus (e.g., diametrical errors)
- Two or more diametrical crossing errors indicates a “failed” test
- If diametrical crossing errors are made, the orientation of the crossing produces a diagnosis of protan, deutan, or tritan color vision deficiency
- This patient’s color vision was normal in each eye
 |
 |
Physical Diagnosis
After reviewing the diagnostic test results, the clinical diagnosis of subjective visual disturbances was changed to a more substantiated physical diagnosis of retrobulbar optic neuritis secondary to presumed multiple sclerosis. An MRI of the brain with and without contrast was ordered.
Magnetic Resonance Imaging (MRI)
Four days after the eye examination, an MRI without and with intravenous gadolinium was performed at a nearby imaging center. There was no prior examination for comparison.
Radiologist’s Findings:
- Within the left side of the splenium of the corpus callosum, there is a lesion measuring about 9 mm in size
- Within the medial left occipital cortex, there is a poorly defined, somewhat curvilinear lesion measuring roughly 12 x 4 mm in size
- Within the medial left parietal cortex, there is a poorly defined lesion measuring 0.8 x 0.6 cm in size
- Within the cortex of the inferior left cerebellum, there is a poorly defined lesion measuring 1.2 x 0.9 cm in size
- There is no enhancement of any of the lesions that suggests neoplastic and/or infectious etiologies
- There is no evidence of restricted diffusion to suggest acute or subacute ischemia
- There is no mass effect, extra-axial fluid, or hydrocephalus
Radiologist’s Impression:
- Given the patient’s age and the involvement of the corpus callosum, demyelinating disease such as multiple sclerosis must be highly considered
- The variable appearance of the lesions is also compatible with demyelinating lesions
- Vasculitides should also be considered
- Neurologic referral is recommended
- Follow-up MRI is recommended
The diagnostic test results suggested strongly that the etiology of the subjective visual disturbances was optic neuritis. Although the exact etiology of the optic neuritis could not be determined based on these test results, the condition was presumed to be related to multiple sclerosis based on the patient’s age and symptoms.
According to Current Procedural Terminology, when eye doctors perform ophthalmological examinations, the complexity of medical decision-making is not separated from the examining techniques used. As a guideline to assist eye doctors in enhancing their medical decision-making skills, consider that the complexity of medical decision-making involves three components.
The first component concerns the number of possible diagnoses and treatment options that must be considered. Optic neuritis is a complex disease with multiple potential etiologies, each etiology having it’s own unique treatment plan.
The second component concerns the amount and complexity of medical records and diagnostic tests that have to be obtained, reviewed and analyzed. In addition to an eye examination, this visit required the review and analysis of a subjective refraction, a retinal laser scan, a threshold visual field examination, an extended color vision examination and a visual evoked potential test. Also, an MRI of the brain was ordered at the conclusion of the in-office diagnostic work-up.
Third, the complexity of medical decision-making is affected by the risk of significant complications and/or morbidity associated with optic neuritis and the risks involved in any treatment options. This patient’s optic neuritis was classified as a significant problem where the risk of total vision loss without treatment was significant and there was significant potential for other systemic co-morbidities. In addition, multiple treatment potentials and coordination of care are essential elements of patients presenting with sight threatening disorders commonly associated with systemic disease.
Treatment Guidelines
Treatment of optic neuritis is directed as the suspected underlying etiology. In most cases, the specific diagnosis will require coordination of care with the patient’s primary care physician and typically a neurologist. Systemic imaging is almost always indicated – enhanced MRI with fat suppression of optic nerve and brain.
Specific to the diagnosis of multiple sclerosis, this specific diagnosis can be very challenging, even to the neurologic specialist. MRI findings show characteristic ovoid, periventricular opacities in the brain white matter, although the presence of these “plaques” varies between 25-75% of the time. Visual field testing typically reveals central defects and/or generalized suppression. Visual evoked potentials show a delayed P100 peak time, the result of axonal demyelination. The VEP abnormality often persists for years after the initial vision problems (80-90% at one year).
Treatment Program
Per the National Multiple Sclerosis Society, current recommended treatment of multiple sclerosis involves four goals:
- Modifying the disease course
- Reducing exacerbations
- Managing symptoms
- Improving function
There are no treatment options applicable to the primary eye care presentation. The Optic Neuritis Treatment Trial definitely showed that treatment of the acute presentation with steroids is contraindicated, especially oral administration. The four treatment goals are best managed by joint efforts of neurology and internal medicine subspecialties.
After reviewing the results of the MRI and determining a physical diagnosis, the patient was referred to a neurologist for further evaluation. After several weeks of additional diagnostic testing, the neurologist diagnosed the patient with multiple sclerosis.
Once treatment is initiated for multiple sclerosis, the eye doctor is still involved in monitoring the ocular manifestations of the disease. In particular, changes in VEP test results can be the earliest sign of disease exascerbation. To that end, a follow up visit was scheduled for 6 months.
Discussion
First, this case demonstrates several key aspects of the challenging differential diagnosis and multiple treatment options for patients presenting with optic neuritis. Because decreased vision is typically the primary symptom in a patient with optic neuritis, optometrists or ophthalmologists are often the first specialists consulted. Although not a key component of treating the systemic disorders associated with optic neuritis, eye doctors play an essential role in the initial diagnosis and coordination of care for these patients.
Second, this patient had been examined by her primary care physician multiple times and was treated with narcotic pain medication – all without a diagnostic work-up to determine the etiology of her chronic pain. Although her visual symptoms became apparent two months before her eye examination, they clearly were not the initial symptoms of her multiple sclerosis. A medical doctor with a higher index-of-suspicion for multiple sclerosis may have allowed for earlier diagnosis and treatment.
Third, this patient did not present with the “classic” signs of optic neuritis associated with multiple sclerosis. There was no sudden onset unilateral vision loss associated with retro-orbital pain that is aggravated by eye movement. Her color vision, optic disc appearance and pupillary reflexes were normal. There was no Uhthoff’s Phenomenon. In fact, her symptoms of chronic pain improved after exercise. This patient is a reminder that every patient is different and can present at any stage in the natural history of the disease.
“Textbook presentations” are just that – for textbooks only.
Last, this case demonstrates that optometrists and ophthalmologists must always be aware of the ocular manifestations of systemic disease. On the date of the examination, the patient’s uncorrected visual acuity was 20/20 in each eye and her fundus examination was normal. Only a careful examination of her gross visual fields, an attentive general medical observation, a detailed review of systems and a comprehensive case history produced the suspicion necessary to order additional diagnostic testing and eventually result in an improved patient care outcome.
Based on patient history, the nature of the presenting problem, and my own clinical judgement this patient needed an evaluation of the complete visual system.
- Perform the eye examination that is medically necessary
- Provide the diagnostic tests or services that are medically necessary
- Properly document the services provided
- Code from the documentation
- Report the services to the payor
| Diagnosis Code | Procedure Code | Modifier | Quantity | Payor | Amount Allowed |
| H53.10 - Unspecified subjective visual disturbances | 92014 - Medical eye examination | 1 | United Healthcare | 101.46 | |
| H53.10 - Unspecified subjective visual disturbances | 92015 - Refraction | 1 | United Healthcare | 20.90 | |
| H53.413 - Scotoma involving central area, bilateral | 92083 - Visual field examination | 1 | United Healthcare | 73.34 | |
| H53.413 - Scotoma involving central area, bilateral | 92133 - Retinal laser scan | 1 | United Healthcare | 49.78 | |
| H46.12 - Retrobulbar neuritis, left eye | 92283 - Color vision examination | 1 | United Healthcare | 43.69 | |
| H46.12 - Retrobulbar neuritis, left eye | 95930 - Visual evoked potential testing | 1 | United Healthcare | 106.02 | |
| Total | $417.24 |
H46.12
Retrobulbar neuritis, left eye
377.32
Retrobulbar neuritis (acute)
92015
Refraction
92083
Visual field examination
92250
Fundus photography
92133
Retinal laser scan
95930
Visual evoked potential
92283
Color vision examination




 Print | Share
Print | Share