Case Report ID: 12
Title:
Contact Lens-Induced Peripheral Corneal Ulcer
Category:
Description:
Contact lens-induced peripheral infiltration or sterile ulceration is a type of marginal keratitis.
It is an acute, non-infectious inflammatory condition that is usually associated with overnight contact lens wear, wearing old disposable lenses, poor lens hygiene, anoxia and idiopathic factors.
Contact lens-induced peripheral ulcer (CLPU) or sterile infiltrates are characterized by the following abnormal signs and symptoms:
- Pain upon awakening
- Foreign body sensation
- Increased tearing
- Increased ocular redness
- Photophobia
- Blepharospasm
- Intermittent decreased vision
Case Report
- A 24-year-old Black woman presented with a chief complaint of eye pain
- Case history described a subjective decrease in comfort over the past 24 hours
- The patient routinely slept in her contact lenses for 1-2 weeks at a time
Conclusion
This presentation presents the common diagnostic dilemma of pure inflammation versus inflammatory disease progressing toward infection versus true corneal infection. Because the clinical signs and symptoms of all three diseases are similar, accurate differential diagnosis is the key to proper treatment.
History of Present Illness
- Associated Signs and Symptoms: decreased vision in the right eye
- Location: right eye
- Duration: this morning (approx 2 hours)
- Quality: deep ocular pain
- Context: sensitive to bright light
- Severity: severe
- Timing: pain is getting worse over time
- Modifiers: none
Review of Systems
- The patient reported that she was in good health and taking no medications
Past, Family and Social History
- Non-contributory
Best Corrected Distance Visual Acuity
- 20/30 in the right eye
- 20/20 in the left eye
Normal Examination Findings
- Mental status
- General medical observation
- Pupils
- Adnexal examination
- Ophthalmoscopy
Not Performed on Today’s Examination
- Gross visual fields
- Basic sensorimotor examination
General Medical Observation
- A well-nourished female in moderate distress secondary to eye pain
Intraocular Pressure Measurements
- 15 mm Hg in the right eye
- 7 mm Hg in the left eye
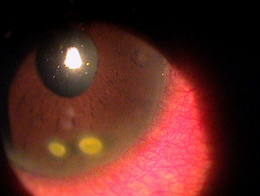
External Ocular Examination with Biomicroscopy
- Begin the biomicroscopic examination with an overview of the cornea using low magnification
- Use a diffuse illumination technique for the initial assessment
- Evaluate corneal infiltrates using high magnification views with direct and indirect illumination techniques as well as vital dye staining techniques
Clinical Diagnosis
The clinical diagnosis is a determination based on the knowledge obtained from the patient’s medical history and from the results of the eye examination alone, without the benefit of diagnostic tests or procedures.
The patient’s clinical diagnosis is contact lens-induced peripheral corneal ulcer based on the following clinical findings:
- History of overnight contact lens wear
- Clinical appearance of the involved eye
- Nature of the presenting problem
Treatment Plan
To gather the clinical information required to treat contact lens-induced peripheral corneal micro-ulcer, a diagnostic and treatment program is initiated.
- Determination of different types of diagnoses
- Selection of one or more treatment options
After a clinical diagnosis has been determined, the diagnostic process continues with a process that involves the identification and exclusion of differential diagnoses. The differential diagnosis process allows the doctor to distinguish between two or more diseases with similar signs and symptoms by systematically comparing their signs and symptoms.
Conditions presenting with similar presentations include:
Sterile, peripheral corneal infiltrate
- Presentation similar to ulceration but epithelium predominantly intact with negative staining
- Not specifically associated with contact lens wear
- Marginal keratitis
- Lesion typically more widespread
- Mucopurulent discharge
- Concurrent eyelid disease
- Immune compromise
Bacterial Keratitis
- Typically focal involvement but more toward central or midperipheral cornea
- Common to have tissue ulceration with extensive infiltration that spreads away from the lesion
- Significant corneal edema
 |
Microbial Keratitis
|
|
Marginal Keratitis
|
Ordering Diagnostic Tests
When additional clinical information is needed to complete the differential diagnostic process or to assist in the treatment program, tests and procedures are ordered. The performance of these tests and procedures leads to the completion of the differential diagnostic process while simultaneously initiating the treatment program. Based on the clinical diagnosis of contact lens-induced peripheral corneal ulcer or infiltrate, the following diagnostic tests could be ordered at the conclusion of the eye examination.
- External ocular photography
- Laboratory analysis
The decision to order and perform additional testing is totally based on the concept of medical necessity which can only be determined by the examining optometrist or ophthalmologist.
Anterior Segment Photography
Any case of compromised tissue that could pose a threat to function could justify the medical necessity of photodocumentation. In this case, the compromised cornea tissue posed risks of infection, true ulceration, and loss of vision. Photodocumentation of the tissue provides a baseline to monitor disease regression and efficacy of treatment.
Laboratory Testing
When there is significant suspicion of true corneal infection, cultures of the suspected pathogen can be considered. Laboratory testing can also be indicated when the presentation does not respond to treatment as expected. In the case of this patient, true infection was not suspected and laboratory analysis not considered medically necessary.
Physical Diagnosis
Completion of the differential diagnosis process either returns you to the original clinical diagnosis or it produces a more substantiated physical diagnosis. This component of the diagnostic and treatment program, the determination of a physical diagnosis, is accomplished by studying the physical manifestations of health and illness revealed in the eye examination, the patient’s complete medical history, and supported by various diagnostic tests and procedures.
According to Current Procedural Terminology, when eye doctors perform ophthalmological examinations, the complexity of medical decision-making is not separated from the examining techniques used. However, as a tool to assist eye doctors in enhancing their medical decision-making skills, consider that the complexity of medical decision-making in this case report involves three components.
Diagnosis Guidelines
The first component concerns the number of possible diagnoses and treatment options that must be considered. The diagnosis and treatment of a potential corneal ulcer is predicated on making the proper diagnosis and on understanding the natural history of corneal ulceration.
The second component concerns the amount and complexity of medical records and diagnostic tests that have to be obtained, reviewed and analyzed. In addition to an eye examination, this visit required the review and analysis of external photodocumentation.
Third, the complexity of medical decision-making is affected by the risk of significant complications and/or morbidity associated with a potential corneal ulcer and the risks involved in any treatment options. True corneal ulcers are a sight and even eye threatening presentation. Even corneal infiltrates pose a signficant risk of scarring and conversion to a more serious ulcerative or infection process.
Treatment Options
To begin the treatment of a corneal infiltrate, the eye doctor must consider the risk of the presenting lesion converting to an infectious process. This is a difficult and sometimes impossible process of clinical guess work. It can be considered conservative if not prudent to consider all corneal lesions as infectious until proven otherwise. This is even more of a factor in a contact lens patient, much less one who abuses lens wear. To this end, aggressive treatment could be recommended initially until the risk of secondary infection is minimized. In 24 hours, a non-infectious lesion with antibiotic cover often does not appear any better but is no worse. Ultimately, sterile infiltrates are a pure inflammatory response and should be treated as such.
Moxeza ophthalmic solution was prescribed q2h and the patient scheduled for a follow-up evaluation the next day. The next day there was a slight reduction in inflammation and no change in the staining pattern. Omnipred ophthalmic solution was prescribed qid, the Moxeza dosage was reduced to tid and the patient asked to return in two days. At that visit there was significant reduction in inflammation and patient symptoms. The corneal lesion was reduced in size. The Moxeza was discontinued, Omnipred continued and the patient scheduled to return in five days. Strong counseling was provided regarding safe wear of contact lenses and any overnight wear of lenses discouraged.
Based on patient history, the nature of the presenting problem, and my own clinical judgement this patient did not need an evaluation of the complete visual system.
- Perform the eye examination that is medically necessary
- Provide the diagnostic test or service that is medically necessary
- Document the service provided
- Code from the documentation
- Document the service provided
- Report the service to the payor
| Diagnosis Code | Procedure Code | Modifier | Quantity | Payor | Amount Allowed |
| H18.821 - Corneal disorder due to contact lens, right eye | 92012 - Medical eye examination | 1 | Cigna | 82.25 | |
| H18.821 - Corneal disorder due to contact lens, right eye | 92285 - External ocular photography | 1 | Cigna | 19.83 | |
| H18.231 - Secondary corneal edema, right eye | 92286 - Specular endothelial microscopy | 1 | Cigna | 39.21 | |
| Total | $141.29 |
H18.821
Corneal disorder due to contact lens,
right eye
371.82
Corneal disorder due to contact lens
370.01
Marginal corneal ulcer
92015
Refraction
92285
External ocular photography




 Print | Share
Print | Share