ICD-10 Diagnosis Codes:
H18.611–Keratoconus, stable, right eye
H18.612–Keratoconus, stable, left eye
H18.613–Keratoconus, stable, bilateral
Title
Keratoconus
Category
Corneal Opacity And Other Disorders Of Cornea
Description
Keratoconus is a disease of the cornea. It is characterized by progressive thinning of the corneal stroma and a progressive steepening in the shape of the cornea.
Keratoconus typically is an isolated ocular disorder but can be seen more commonly in patients with Down’s Syndrome, atopic disease, mitral valve prolapse and patients that exhibit chronic eye rubbing (often from atopic disease).
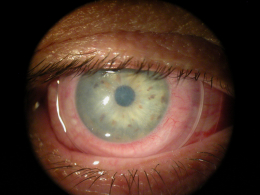
Structural Damage to the Eye
- Steepening of the cornea especially the inferior region
- Thinning of the corneal apex
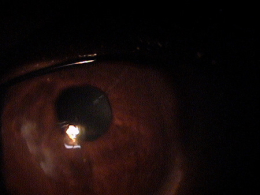
- Fine “tension” lines in the deep stroma (Vogt’s striae)
- All these findings producing mild to severe irregular corneal astigmatism
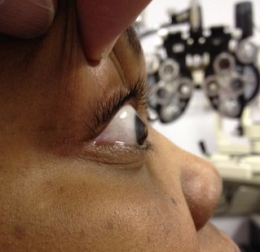
- Bulging of the inferior cornea to the point of producing a visible cone when the patient looks down (Munson’s sign)
- Ring of iron deposit accumulates in corneal endothelium at the base of the cone (Fleischer Ring)
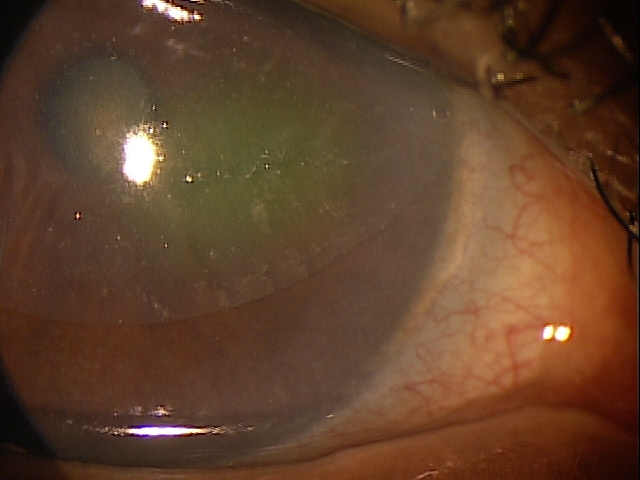
- Breaks in the posterior cornea lead to severe stromal edema (acute corneal hydrops)
Functional Change in the Visual System
- Decreased vision – quantitatitve and qualitative
- Glare
- Halos around lights
- Monocular diplopia
- Ghost images
- Multiple unsatisfactory attempts in obtaining good visual acuity with eyeglasses
- Often reports of functional vision only when wearing contact lenses, especially gas permeable lenses
- Can also report contact lens intolerance
The main goal of the diagnostic evaluation in a patient with keratoconus is to accomplish the following:
- Make a definitive diagnosis of keratoconus
- Determine if the patient can function adequately with an eyeglasses prescription
- If not, prescribe medically necessary contact lenses
Patient History
Patients with keratoconus may present with any of the following signs and symptoms:
- None
- Systemic history of Down’s Syndrome, atopic disease or mitral valve prolapse
- Photophobia
- Halos around lights
- Monocular diplopia
- Variable and inconsistent refractions
- History of multiple spectacle prescriptions in a short period of time
- Complaints of distortion rather than blurred vision at both distance and near
External Examination with Biomicroscopy
DIAGNOSTIC TESTS
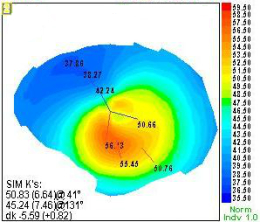
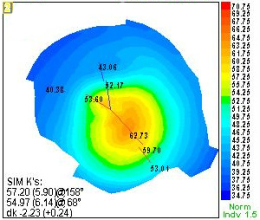
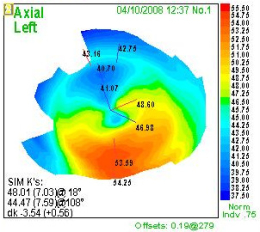
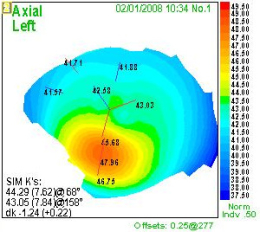
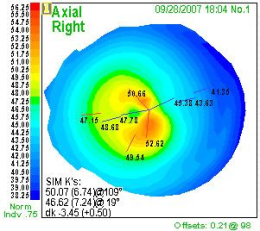
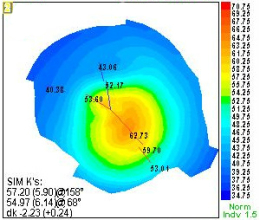
Computerized Corneal Topography
Anterior Segment Imaging
- In-vivo imaging of the cornea
- Optical coherence tomography produces a cross-section of the cornea showing the anatomy and quality of the tissue
- Measures corneal thickness
- Anterior segment imaging can determine the location of the most severe area of cornea thinning and ectasia
Although keratoconus can be classified by the shape of the cone, by the central keratometric measurement, or by its level of severity in producing visual impairment, a common system of classification uses clinical findings to define four stages of keratoconus.
Stage 1 – Mild Keratoconus
|
 |
|
Stage 2 – Moderate Keratoconus
|
 |
|
Stage 3 – Advanced Keratoconus
|
 |
|
Stage 4 – Severe Keratoconus
|
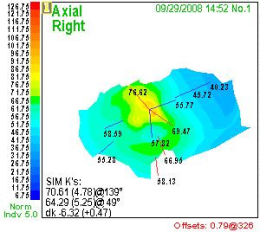 |
Corneal Warpage due to Contact Lens Wear
Wearing contact lenses, especially high-riding gas permeable lenses, can produce reversible irregular corneal astigmatism. The topographic appearance can easily mimic early keratoconus. Refitting the lenses and monitoring the condition over time may be the only way to confirm the lack of corneal disease.
Other Causes of Irregular Astigmatism
Consider other causes of irregular corneal astigmatism from corneal scarring – prior corneal surgery including refractive surgery, trauma and healed past infections. Iron deposits can also occur in patients with pterygium, surgical scars and central depression from refractive surgery.
Induced Hypoxia or Early Signs of Endothelial Failure
Stromal striations similar to Vogt’s striae can occur in severe contact lens-related corneal edema or the late stages of Fuchs’ endothelial dystrophy.
Terrien Marginal Corneal Degeneration
Terrrien marginal corneal degeneration is a mild inflammatory disease affecting the superior limbus, which can induce irregular against-the-rule astigmatism from the neovascularization and lipid deposits on the cornea.
Keratoglobus
Keratoglobus is a rare disease in which the entire cornea, from limbus to limbus, thins. The thinning can cause the cornea to spontaneous perforate.
Posterior Keratoconus
Posterior keratoconus is a rare, congenital disease were the posterior cornea protrudes into the stroma.
Pellucid Marginal Degeneration
This condition is characterized by a corneal thinning that occurs about a millimeter above the inferior limbus which leads to ectasia. Although pellucid marginal degeneration is similar to keratoconus, most eye doctors believe that they are two distinct conditions.
Pellucid may have significantly less effect on qualitative vision, may occur in older patients and often shows slower to sometimes clinically insignificant progression.
Treatment with Eyeglasses
- Patients with mild keratoconus can usually obtain functional vision with glasses
- As the disease progresses patients may need new eyeglass prescriptions as frequently as every six months
Mechanical Treatment
According to the Collaborative Longitudinal Evaluation of Keratoconus (CLEK) Study, over 70% of patients with keratoconus wear contact lenses.
Treatment with Contact Lenses
|
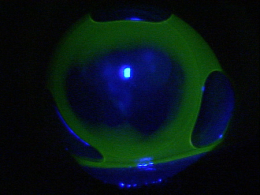
Central bearing reveals a flat |
Pharmacologic Treatment
- Hypertonic eye drops and ointments to manage acute corneal hydrops
- Cycloplegic eye drops to reduce eye pain in acute corneal hydrops
- Topical steroid eye drops to reduce inflammation in acute corneal hydrops
Surgical Treatment
Consider surgical treatment options if mechanical and pharmacologic treatments are unsuccessful.
- Amniotic membrane placement
- Penetrating keratoplasty
- Lamellar keratoplasty
- Excimer laser corneal ablation
- Intact corneal implants
- Corneal collagen cross-linking with ultraviolet A and ribloflavin (currently under investigation)
- Sulfur hexafluride gas (SF6) to reduce corneal edema during episodes of acute keratoconus (currently under investigation)
Amiotic Membrane Inserts
1. Weissman B. Keratoconus. Medscape/EMedicine. 22 Apr 2014. http://emedicine.medscape.com/article/1194693-overview. Last accessed August 17, 2014.
2. John T. A Wide-Angle View of Keratoconus. RevOptom. Oct 2012. http://www.revoptom.com/continuing_education/tabviewtest/lessonid/108692/. Last accessed August 17, 2014.
3. Shovlin J. Softer Approach to Keratoconus? RevOptom. 15 June 2012. http://www.revoptom.com/content/d/contact_lenses___and___solutions/c/35207/. Last accessed August 17, 2014.
371.60
Keratoconus
76513
Anterior segment ultrasound
76514
Corneal pachymetry
92015
Refraction
92025
Corneal topography
92285
External ocular photography
92132
Anterior segment imaging
92071
Bandage contact lens
92072
Treatment with contact lens
65778
Amniotic membrane placement
Occurrence
- 50-200 cases per 100,000 population
- Most keratoconus cases appear spontaneously, although approximately 14% of cases present with evidence of genetic transmission
Distribution
- An equal incidence of keratoconus occurs in males and females
Risk Factors
- Ocular allergies
- Rigid contact lens wear
- Vigorous eye rubbing




 Print | Share
Print | Share