ICD-10 Diagnosis Codes:
H18.621–Keratoconus, unstable, right eye
H18.622–Keratoconus, unstable, left eye
H18.623–Keratoconus, unstable, bilateral
Title
Keratoconus Acute Hydrops
Category
Corneal Opacity And Other Disorders Of Cornea
Description
Corneal hydrops occurs after a rupture in Descemet’s membrane and is characterized by severe corneal edema.
Corneal hydrops occurs when the barrier function of the posterior cornea is compromised after a rupture in Descemet’s membrane. The break in Descemet’s membrane allows fluid into the corneal stroma and results in severe corneal edema.
Corneal hydrops can occur in the following diseases:
|
 |
Acute corneal hydrops occurs in about 3% of all patients with keratoconus and 86% of the patients that experience a hydrops event have keratoconus.
Risk factors for keratoconic patients developing corneal hydrops include the following:
- Rapid keratoconus progression
- Severe allergic disease
- Down’s syndrome
- Young age at the time of initial diagnosis
- Poor visual acuity at the time of initial diagnosis
Structural Damage to the Eye
Keratoconus is a non-inflammatory thinning and protrusion of the cornea. It is usually bilateral, but is often asymmetric in its presentation. In advanced keratoconus, vision loss can occur when a spontaneous rupture of Descemet’s membrane leads to acute corneal hydrops and corneal scarring.
Functional Damage to the Eye
- Sudden monocular visual impairment
- Severe decrease in vision if the corneal edema is located in the visual axis
The main goal of a diagnostic evaluation in a patient with acute corneal hydrops is to accomplish the following:
- Determine the proximity of the area of edema to the corneal limbus
- Rule out any potential complications (e.g., infectious keratitis, corneal perforation, neovascular glaucoma)
- Relieve ocular pain and any other associated symptoms
- Prescribe a treatment program to manage the patient’s recovery
Patient History
Patients with acute corneal hydrops may present with any of the following signs and symptoms:
- Sudden corneal opacififcation
- Monocular visual impairment
- Ocular discomfort
- Photophobia
- Epiphora
Approximately 29% of patients can identify a traumatic inciting event that ruptured Descemet’s membrane.
- Vigorous eye rubbing — 67% of patients with trauma-induced acute corneal hydrops
- Traumatic contact lens insertion — 33% of patients with trauma-induced acute corneal hydrops
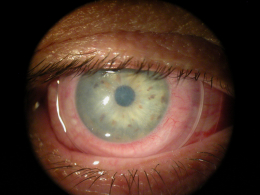
External Ocular Examination with Biomicroscopy
- Determine the proximity of the area of edema to the corneal limbus
- Estimate the total area of the corneal surface affected by the edema
DIAGNOSTIC TESTS
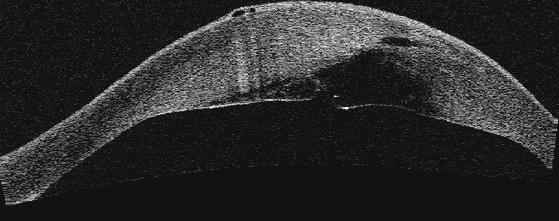
Anterior Segment Imaging
- To document the corneal thinning and protrusion seen in keratoconus
- To document the deliver of medical treatment
- To document the response to treatment
- To help plan a treatment program
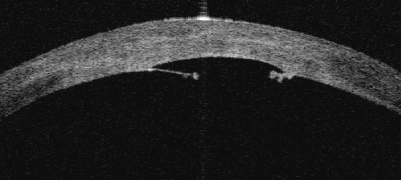
Anterior segment imaged with a Visante OCT by Carl Zeiss Meditec
- 35-year-old black male with advanced keratoconus
- Corneal protrusion (bulging) in both eyes
- Paracentral corneal thinning in both eyes
- Maximal corneal thinning near the apex of the protrusion
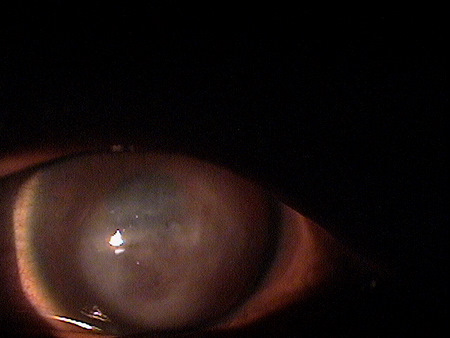
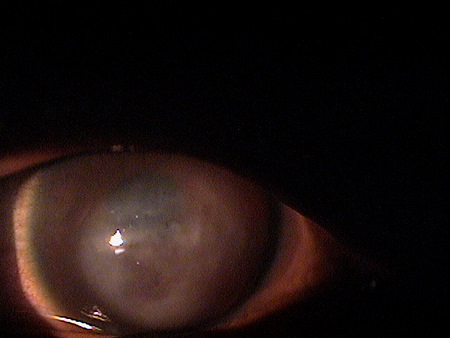
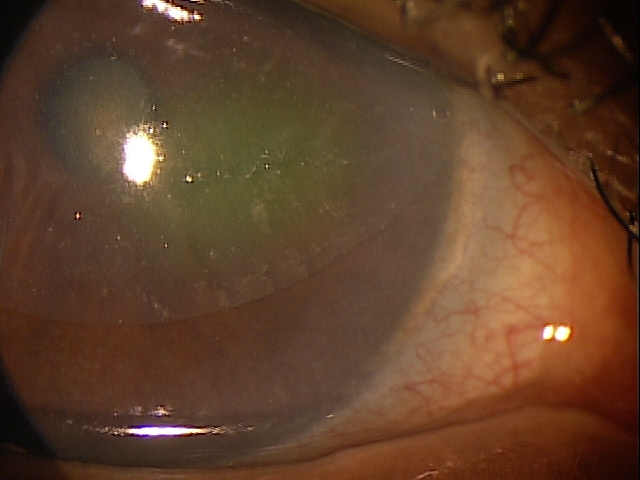
External Ocular Photography
- To document the corneal hydrops
- To help plan a treatment program
Corneal hydrops has no classification other than a corneal degeneration as it is secondary to pre-existing corneal disease.
Corneal hydrops is almost always associated with a decompensated keratoconic condition. It is often preceded by additional stress on the cornea in the form or excessive rubbing, damage from contact lens insertion and removal, or trauma to the eye. This history should reveal the prior diagnosis of keratoconus.
Another possible differential for acute hydrops is an advanced corneal endothelial dystrophy, especially Fuchs’. Again, the clinical picture and history should be definitive of the prior existence of chronic Fuchs’ endothelial dystrophy.
The only other significant potential differential, and likely the most worrysome, would be an infectious keratitis. In this case, the decompensation should be more focal, associated with a mucopurulent discharge, and likely a history of extended wear contact lenses or trauma to the eye.
Treatment of corneal hydrops depends on the causative factor.
Corneal Hydrops Secondary to Keratoconus
Hydrops secodary to keratoconus requires minimal but necessary intervention. The eye should be protected with a plastic shield. Prophylactic, broad spectrum topical antibiosis is definitely warranted. Some doctors recommend a light pressure patch changed daily. Others advocate a large bandage contact lens, although some corneal specialists feel the use of a bandage lens is contraindicated due to the potential for increasing the likelihood of a neovascular response.
An excellent compromise could be a amnionic membrane allograft. If the hydrops is secondary to keratoconus, the cornea will scar over that area resulting in even greater reduction of vision. The patient should be made aware of this. Once significant fibrin scarring is completed, surgical repair of the opacified cornea can be considered.
If complete perforation of the cornea is present, applying a Fox shield and referring the patient to a corneal specialist is advised.
Corneal Hydrops Secondary to Fuchs’ Endothelial Dystrophy
Treatment of hydrops secondary to Fuchs’ dystrophy would be similar to hydrops caused by keratoconus.
Corneal Hydrops Secondary to Infectious Keratitis
This would be an unlikely presentation as an infections disorder would more likely cause true perforation of the cornea. In this case, the eye should be shielded and referred immediately to a corneal specialist.
1. Weissman B. Keratoconus. Medscape/EMedicine. 22 Apr 2014. http://emedicine.medscape.com/article/1194693-overview. Last accessed August 17, 2014.
2. John T. A Wide-Angle View of Keratoconus. RevOptom. Oct 2012. http://www.revoptom.com/continuing_education/tabviewtest/lessonid/108692/. Last accessed August 17, 2014.
3. Shovlin J. Softer Approach to Keratoconus? RevOptom. 15 June 2012. http://www.revoptom.com/content/d/contact_lenses___and___solutions/c/35207/. Last accessed August 17, 2014.
371.62
Keratoconus acute hydrops
92285
External ocular photography
76514
Corneal pachymetry
92132
Anterior segment imaging
76513
Anterior segment ultrasound
65778
Amniotic membrane placement




 Print | Share
Print | Share