Case Report ID: 71
Title
Preoperative Evaluation and Postoperative Management for Epiretinal Membrane Surgery
Category
Peri-Operative Management Of Ocular Surgery (4)
Description
Epiretinal membranes can produce contractile forces on the surface of the retina that damage its structure. This case presents the diagnosis and treatment of the membrane and the postoperative macular pucker.
Case Report
xxxxxxxxxxxx
Conclusion
xxxxxxxxxxx
.
History of Present Illness
- xxxxx
- xxxxx
Review of Systems
- xxxxx
- xxxxx
Past, Family and Social History
Non-contributory
Best Corrected Distance Visual Acuity
- 20/25 in the right eye
- 20/40 in the left eye
Normal Examination Findings
- General medical observation
- Gross visual fields
- Basic sensorimotor examination
- External examination
- Pupillary examination
- Adnexal examination
- External ocular examination with biomicroscopy
Intraocular Pressure Measurements
- 14 mm Hg in the right eye
- 14 mm Hg in the left eye
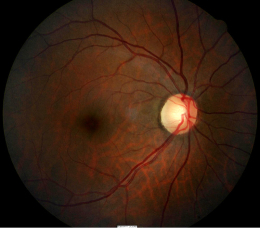
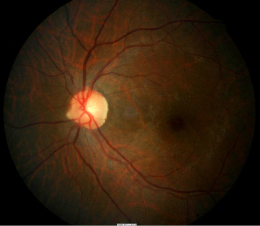
Ophthalmoscopy
- Normal fundus appearance in the right eye
- Small epiretinal membrane in the left eye
Clinical Diagnosis
The clinical diagnosis is a determination based on the knowledge obtained from the patient’s medical history and from the results of the eye examination alone, without the benefit of diagnostic tests or procedures.
The patient’s clinical diagnosis is macular pucker based on the following clinical findings:
- Recent history of cataract surgery in the left eye
- Unexpected decreased visual acuity in left eye
- Ocular discomfort in the left eye
- Presence of bullous keratopathy on the left cornea
Treatment Plan
To gather the information required to properly counsel a patient regarding postoperative management for epiretinal membrane surgery, a diagnostic and treatment program is initiated.
- Determination of different types of diagnoses
- Selection of one or more treatment options
Ordering Diagnostic Tests
Testing beyond the eye examination should not be conducted unless significant signs or symptoms exist. Even then, the only services necessary would be the comprehensive eye examination and an A-scan. The following would not be reimbursed unless medical necessity is documented.
- Contrast sensitivity
- Potential acuity
- Non-screening visual fields
- Fluorescein angiography
- External ocular photography
- Specular endothelial microscopy
- Corneal pachymetry
- Extended color vision examination
- Electrodiagnostic testing
The decision to order and perform additional testing is totally based on the concept of medical necessity which can only be determined by the examining optometrist or ophthalmologist.
Refraction
- Measuring visual acuity is a method of evaluating functional vision loss
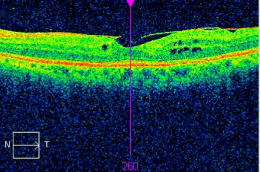
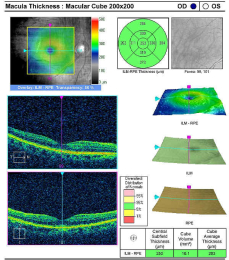
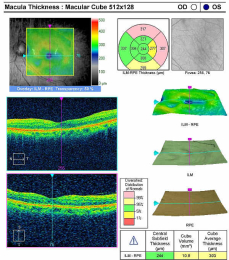
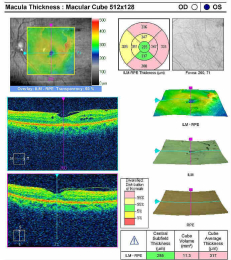
Retinal Laser Scan — Macula
- The procedure can be accomplished by using the Cirrus OCT manufactured by Carl Zeiss Meditec
Right Eye
- Normal retinal thickness
- Normal foveal depression
Left Eye — Preoperative
- Epiretinal membrane overlying the macula
- Loss of normal macular structure (e.g., deformation of the retinal surface)
- Dark areas are foveal cysts
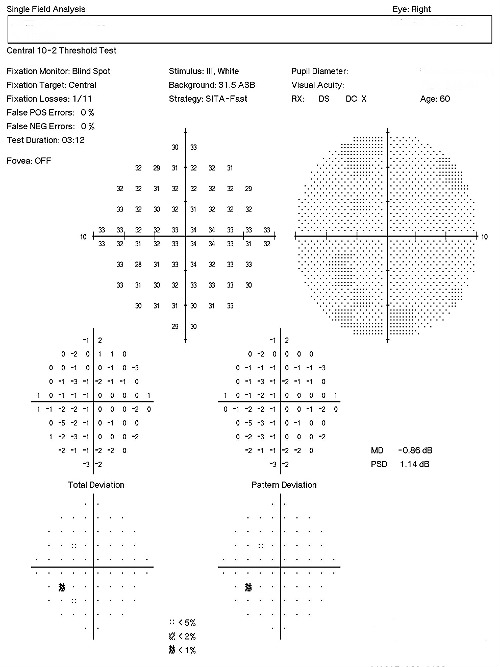
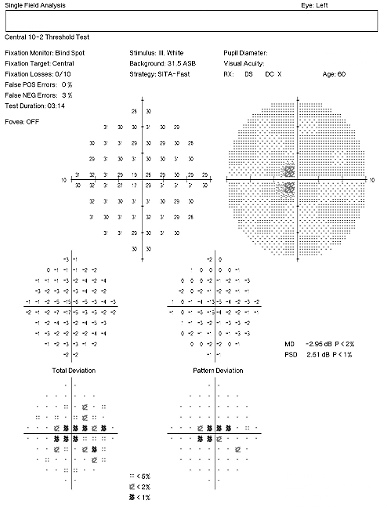
Visual Field Examination
- Automated threshold perimeters measure the visual field by plotting the threshold luminance value of the patient in various locations in the visual field
- The luminance of the light stimulus is represented by non-specific units of measurement called decibels (dB)
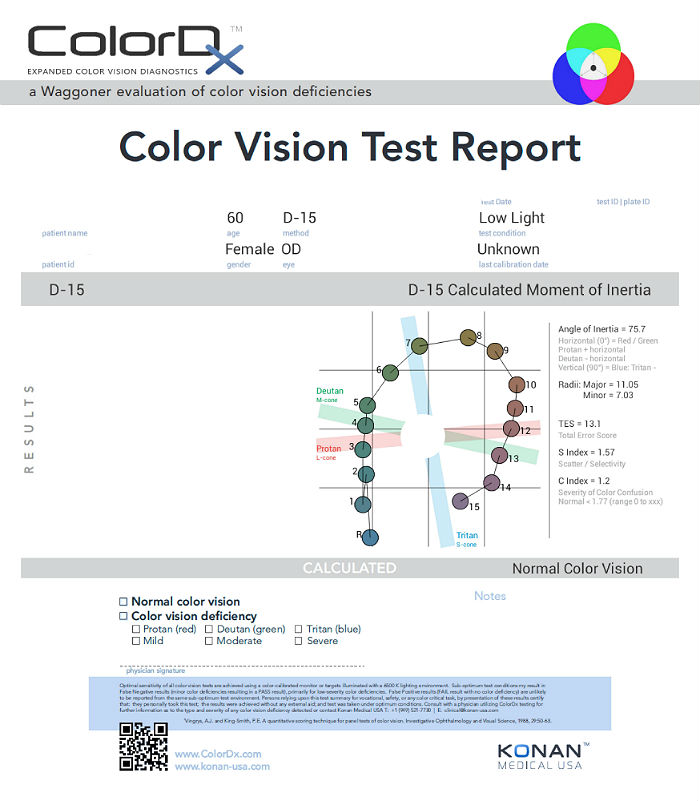
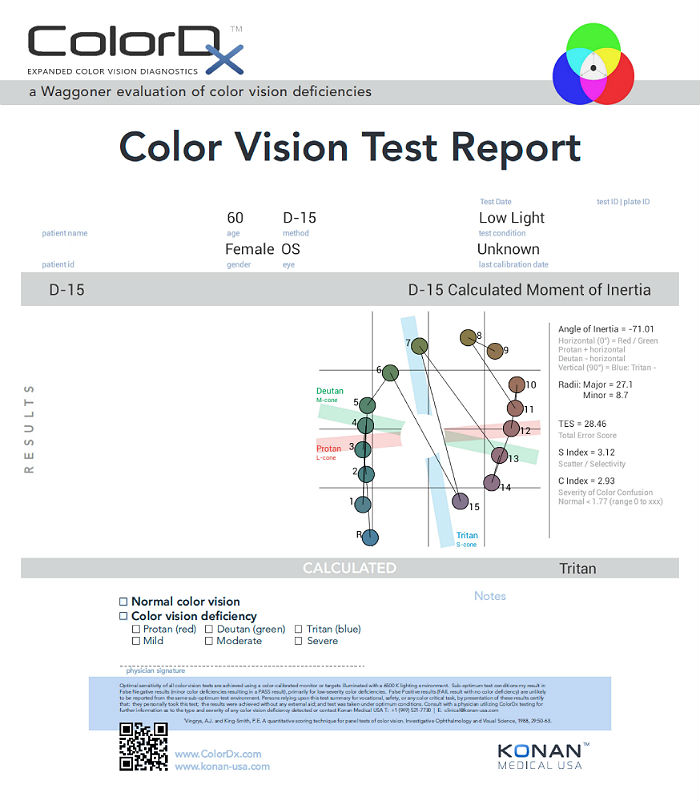
Color Vision Examination
An extended color vision examination measures the combined function of the retina, the optic nerve and the intracranial visual pathway and is used clinically to detect or monitor color vision loss due to disease at any of these locations. Extended color vision testing divides people into two groups.
- The first group consists of people with normal color vision and slight color deficiency
- The second group consists of people with moderate or severe color deficiency
One of the most common tests performed in clinical practice is the Farnsworth D15. When performed on Konan Medical’s ColorDx software, the test is presented as fifteen colored bars and one fixed bar on an Android tablet. The hue of each bar has been chosen so that the adjacent bars have approximately equal hue differences. When the bars are arranged in order, they form a hue circle. As a result, errors in hue discrimination can be made across the hue circle.
Patients with normal color vision usually make no error but may make one or two minor transposition errors, as do those with mild color vision deficiency. Patients with more advanced color deficiency make some or more of the following errors:
- They place colors that lie on the opposite side of the hue circle next to colors that lie on their confusion locus (e.g., diametrical errors)
- Two or more diametrical crossing errors indicates a “failed” test
- If diametrical crossing errors are made, the orientation of the crossing produces a diagnosis of protan, deutan, or tritan color vision deficiency
- Normal color vision in the right eye
- Acquired color vision defect (tritan) in the left eye
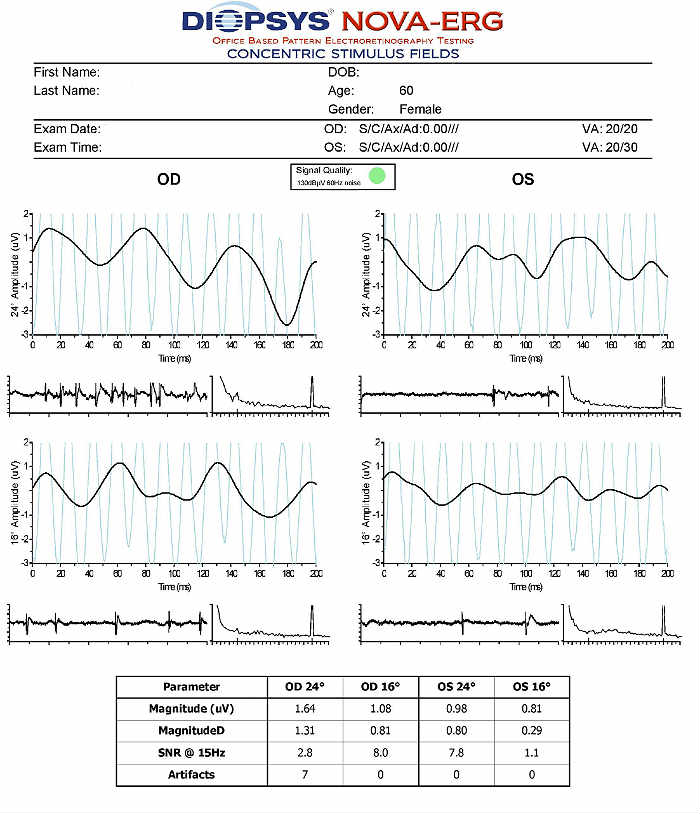
Electroretinography
- Electroretinogram testing evaluates the integrity of the retina
- The procedure can be accomplished using the NOVA-ERG Testing Device manufactured by DIOPSYS
- Specialized pattern electroretinogram (PERG) test uses a contrast-reversing pattern for the stimulus to produce information about ganglion cell function
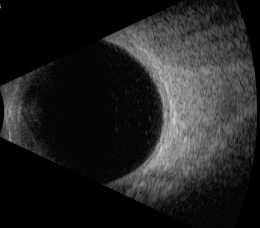
B-Scan Ophthalmic Ultrasound
- Document the presence or absence of ultrasound hollowness within the choroidal nevus
- Document the height of the choroidal nevus
- Document the presence or absence of choroidal tissue excavation
|
B-Scan Ultrasound — Left Eye
|
According to Current Procedural Terminology, when eye doctors perform ophthalmological examinations, the complexity of medical decision-making is not separated from the examining techniques used. As a guideline to assist eye doctors in enhancing their medical decision-making skills, consider that the complexity of medical decision-making involves three components.
The first component concerns the number of possible diagnoses and treatment options that must be considered. Determination of the diagnosis of vitreomacular traction syndrome involves the determination of structural damage to the vitreous and retina with associated functional loss of vision. There are many other potential causes for structural alteration in the macula so the differential diagnosis shows moderate complexity.
The second component concerns the amount and complexity of medical records and diagnostic tests that have to be obtained, reviewed and analyzed. In addition to an eye examination, this visit required the review and analysis of a subjective refraction, a retinal laser scan, and a threshold visual field examination.
Third, the complexity of medical decision-making is affected by the risk of significant complications and/or morbidity associated with vitreo-macular traction and the risks involved in any treatment options. This patient’s retinal condition was classified as a significant problem where the risk of significant central vision loss without treatment was possible. In addition, the treatment plan will involve continued monitoring of the retinal condition.
Surgical Treatment Guidelines
In moderate-to-advanced cases, surgical vitrectomy is often successful in restoring normal or near normal acuity levels. More recently, retinal surgeons are using proteolytic enzymes to dissolve the vitreous attachments. Jetrea (ocriplasmin) is the first such intravitreal agent for this purpose.
Most retinal specialists use the following criteria to determine the need for surgical treatment:
- 20/50 – 20/70 or worse visual acuity
- Declining visual acuity
- Patients with an intolerance for visual distortions
Clinical signs of any of the following:
- Cystoid macular edema
- Vascular incompetence
- Impending macular hole
Since a significant number of vitreomacular traction cases resolve spontaneously, clinicians should be slow to recommend invasive surgery until Snellen acuity loss exceeds 20/50 or structural retinal changes point to a significant risk of macular hole formation. Retinal surgeons establish individual thresholds related to the decision to perform surgery, typically strongly based on Snellen acuity. Eye doctors should familiarize themselves with these thresholds so referral options can be made only at the appropriate time.
Surgical Treatment
Pars Plana Vitrectomy with Membrane Peel
Potential side effects include the following
- Intraocular inflammation
- Intraocular infection
- Intraocular hemorrhage
- Retinal detachment
- Extended recovery period
Treatment Program
Observation for Spontaneous Resolution — The patient was counseled regarding the condition and the need for home monitoring with Amsler grid. Any changes in acuity or the Amsler grid should be reported immediately. Because this was the initial diagnosis of vitreomacular traction syndrome, the next visit was scheduled for 1 month.
Palliative Treatment
- Observation in the early stages of the disease and there is minimal pulling-effect upon the macula
Pharmacologic Treatment
JETREA Intravitreal Injection
- Liquefies vitreous
- Produces a separation between the vitreous cortex and the internal limiting membrane
- Resolution of vitremacular traction in 26% of treated group during Phase III clinical studies
Potential side effects include the following:
- Intraocular inflammation
- Intraocular infection
- Intraocular hemorrhage
- Increased intraocular pressure
- Lens subluxation
- Floaters
- Retinal detachment
- Changes in color vision
Discussion
Traction on the macular tissue produces gradual, anatomic and functional deterioration in proportion to traction forces and their duration of action. Macular traction is tangential to the macular surface in disorders such as cellophane maculopathy, macular pucker and macular hole. Macular traction is anterior/posterior to the macular surface in vitreomacular traction syndrome. Traction maculopathies are estimated to occur in 6.4% of the population over age 50.
This case demonstrates management of a common condition that eye doctors can easily become uncomfortable with. For example, vitreomacular adhesion can lead to vitreomacular syndrome. Complications include loss of vision secondary to retinal thickening, foveal cysts, vascular incompetence, cystoid macular edema and macular hole. In addition, cataract surgery increases the complications from vitreomacular traction syndrome.
Even though the microscopic retinal appearance can often be disturbing, the patient may have near normal acuity. If the visual acuity declines, referral to a retinal specialist may be warranted. Because of the risk of surgical intervention combined with the nature of the condition to spontaneously resolve, referrals for surgical intervention should be conservatively considered.
Based on patient history, the nature of the presenting problem, and my own clinical judgement this patient needed an evaluation of the complete visual system.
- Perform the eye examination that is medically necessary
- Provide the diagnostic tests or services that are medically necessary
- Properly document the services provided
- Code from the documentation
- Report the services to the payor
| Diagnosis Code | Procedure Code | Modifier | Quantity | Payor | Amount Allowed |
| H35.372 - Puckering of macula, left eye | 92014 - Medical eye examination | 1 | Aetna | 90.43 | |
| H35.372 - Puckering of macula, left eye | 92015 - Refraction | 1 | Aetna | 14.04 | |
| H35.372 - Puckering of macula, left eye | 92083 - Visual field examination | 1 | Aetna | 47.88 | |
| H35.372 - Puckering of macula, left eye | 92133 - Retinal laser scan | 1 | Aetna | 32.40 | |
| H35.372 - Puckering of macula, left eye | 92283 - Color vision examination | 1 | Aetna | 41.40 | |
| H35.372 - Puckering of macula, left eye | 92275 - Electroretinography | 1 | Aetna | 116.60 | |
| Total | $298.40 |
H35.372
Puckering of macula, left eye
H43.312
Vitreous membranes and strands,
left eye
362.56
Macular pucker
379.25
Vitreous membranes and strands
92283
Color vision examination
92275
Electroretinography (ERG)
92250
Fundus photography
92083
Visual field examination,
extended intensity
76512
B-scan ultrasound




 Print | Share
Print | Share