Case Report ID: 22
Title:
Preoperative Evaluation For Cataract Surgery
Category:
Peri-Operative Management Of Ocular Surgery (4)
Description:
This case presents treatment guidelines for a patient about to undergo cataract surgery.
Cataract surgery is a common out patient surgical procedure. Both optometrists and ophthalmologists should be aware of new medicologal considerations regarding cataract surgery and Medicare’s or other payor’s established guidelines regarding the medical necessity of patients having cataract surgery.
All patients should undergo a PARQ Conference prior to submitting to cataract surgery. The conference covers the following topics:
- Procedure
- Alternatives
- Risks
- Questions
Case Report
- A 68-year-old white male presents to the office complaining of decreased vision
- Temporal history revealed a previous examination and new eyeglasses less than one year earlier that provides unsatisfactory vision
- The patient has been told previously that he has cataracts and is now ready to consider cataract surgery. He states he can no longer safely drive at night and he does volunteer work at his church two nights a week. He also states he cannot read the print in his Bible or on his computer even with a store bought magnifier.
Conclusion
The PARQ conference involves the patient giving his/her informed consent to undergo cataract surgery. For the doctor to discuss any risks of the proposed surgery with the patient, certain clinical information must be obtained and certain questions must be answered.
- Are there any signs of corneal endothelial dystrophy?
- Are there any signs of peripheral retinal disease?
- Are there any signs of vitreoretinal interface pathology?
- Are there any repeatable visual field defects?
- Are there any other ophthalmic or systemic conditions that could influence the procedure or expected visual outcome?
History of Present Illness
- Associated Signs and Symptoms: none
- Location: vision is worse in both eye
- Duration: past three years
- Quality: n/a
- Context: decreased vision was initially only bothersome at night but now is affecting all vision tasks
- Severity: moderate to severe decrease in vision
- Timing: vision seems to be getting worse over time
- Modifiers: none
Review of Systems
The patient reported that he was being treated for hypertension, type II diabetes and a “problem with his prostate.” He was currently taking metformin and prazosin.
Past, Family and Social History
- Non-contributory
Uncorrected Distance Visual Acuity
- 20/30 in the right eye
- 20/50 in the left eye
Normal Examination Findings
- Mental status
- General medical observation
- Pupils
- Gross visual fields
- Basic sensorimotor examination
- Adnexal examination
- External examination
- Ophthalmoscopy
Intraocular Pressure Measurements
- 15 mm Hg in the right eye
- 16 mm Hg in the left eye
External Ocular Examination with Biomicroscopy
- +2 cortical clouding in the right eye
- +3 cortical clouding in the left eye
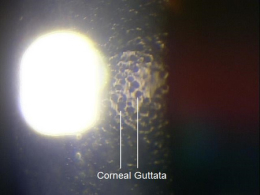
- Corneal guttata in both eyes
Clinical Diagnosis
The clinical diagnosis is a determination based on the knowledge obtained from the patient’s medical history and from the results of the eye examination alone, without the benefit of diagnostic tests or procedures.
The patient’s clinical diagnosis is cataract and corneal endothelial dystrophy based on the following clinical findings:
- Presence of cortical changes in the lenses of both eyes
- Presence of corneal guttata in both eyes
- Decreased visual acuity in both eyes
Treatment Plan
To gather the information required to properly counsel a patient regarding developing cataracts and endothelial dystrophy, a diagnostic and treatment program is initiated.
- Determination of different types of diagnoses
- Selection of one or more treatment options
The diagnosis of cataract with reduction in functional vision is relatively straightforward. The equally important clinical decisions are:
- Are the cataracts causing reduction in vision that is effecting the patient’s quality of life?
- Are other conditions present that could be causing the patient’s reduced vision?
Many patients present with reported reductions in vision before surgery is actually indicated while others have advanced cataract development due to delayed reporting. The decision to recommend surgery is based on three variables:
- Is the patient experiencing an interrupting with or problem with activities of daily living that could be enhanced by removing their clouded lens?
- Does an assessment of the risk/benefit ratio fall in favor of the minimal risks related to cataract surgery?
- Are there restrictions in the patient’s insurance payor plan that would not allow coverage for cataract surgery at the patient’s level of clinical presentation and resultant symptoms?
While the risk of cataract progression is high, the risk of secondary damage to the eye from the cataract is low. Except in the case of phacomorphic lens development and the associated risk of secondary glaucoma, there are few cases in modern times where a cataract must be removed to prevent associated ocular damage.
Since the risks associated with cataract surgery are low, lens removal should and can be considered once the patient is experiencing documented limitation of lifestyle. This approach to managing effects on lifestyle issues can downplay the role of Snellen acuity. Optometrists and ophthalmologists must still remain knowledgeable of the particular limitations for surgery that may be present in individual payor payment policy.
In this case, the patient reported problems with several activities of daily living (ADLs) – night driving, reading his Bible, and working on his computer.
Ordering Diagnostic Tests
Testing beyond the eye examination should not be conducted unless significant signs or symptoms exist. Even then, the only services necessary would be the comprehensive eye examination and an A-scan. The following would not be reimbursed unless medical necessity is documented.
- Contrast sensitivity
- Potential acuity
- Non-screening visual fields
- Fluorescein angiography
- External ocular photography
- Specular endothelial microscopy
- Corneal pachymetry
- Extended color vision examination
- Electrodiagnostic testing
The decision to order and perform additional testing is totally based on the concept of medical necessity which can only be determined by the examining optometrist or ophthalmologist.
Refraction
- Measuring visual acuity is a method of evaluating functional vision loss
- Cataracts can produce a loss of visual acuity as well as loss of quality of vision
- There was no improvement in visual acuity in either eye after a subjective refraction was performed or by pinhole testing
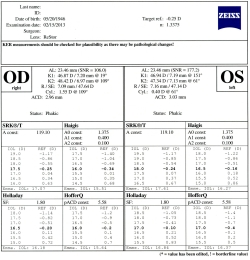
Specular Endothelial Microscopy
Most modern day cataract surgery is performed by phacoemulsification techniques. These techniques have documented risks for the corneal endothelium secondary to high turbulence factors. Knowledge of the health of the corneal endothelium assists in preoperative counseling in two ways.
First, if the corneal endothelium is compromised enough, the decision to proceed with cataract surgery can be delayed or even reversed. It may present a situation where corneal surgery is considered before cataract surgery or combined with cataract surgery. Second, and more commonly, knowledge of the health of the corneal endothelium can provide a better prediction of postoperative acuity limitations secondary to surgically-induced (iatrogenic) corneal edema. With this knowledge, the doctor is better prepared to counsel the patient regarding the speed of recovery following surgery and the surgeon can potentially take precautions to minimize the usual stresses placed on the endothelium during routine phacoemulsification.
According to the Centers for Medicare and Medicaid Services, patients about to undergo a surgical procedure associated with a high risk to the corneal endothelium should have a preoperative risk assessment that includes specular microscopy if they have slit-lamp evidence of an endothelial dystrophy or corneal edema.
Surgical trauma during cataract surgery generally results in a 4-10% loss of endothelial cells, a condition known as iatrogenic endotheliopathy. Risk factors for a higher percentage of postoperative cell loss include the following:
- Diabetes
- Glaucoma
- Pre-existing endothelial disease
- Shallow anterior chamber
- Previous ocular surgery
According to the American Academy of Ophthalmology, if the endothelial cell density is high, the risk of chronic postoperative corneal edema is low. Conversely, if the endothelial cell density is low, the risk of chronic postoperative corneal edema is high. To perform the preoperative risk assessment, first determine the endothelial cell density using specular microscopy. Then, after performing specular microscopy, the doctor can determine the level of risk and counsel the patient accordingly.
The following table provides a guideline for assessing the potential problems with cataract surgery related to corneal endothelial cell density:
| Endothelial Cell Functional Reserve | Endothelial Functional Reserve Ability | Surgical Risk For Postoperative Edema |
| Above 2000 mm2 | High | Low |
| 1000 - 2000 mm2 | Adequate | Moderate |
| 500 - 1000 mm2 | Low | High |
| 300 - 500 mm2 | Minimum | High |
| Below 300 mm2 | None | High |
Knowledge of the biometry of a patient’s eye is essential for proper intraocular lens power selection but can also be beneficial in making the decision to recommend surgery. These are different diagnostic services requiring different billing strategies.
A-Scan Ultrasound
A-scan with IOL power calculation (CPT Code 76519) is used exclusively for the stated purpose. Any doctor billing for this service should make sure they are completing the requirements of the code description, which includes determining the IOL power. A-scan for diagnostic purposes (CPT Code 76511) applies to measuring and analyzing the sizes, depths and structure of the globe contents. A diagnostic A-Scan is applicable in preoperative cataract evaluations when it is determined that abnormal or unphysiologic globe biometry (shallow anterior chamber, enlarged lens, etc) could warrant an earlier consideration of cataract surgery to restore a more functional intraocular anatomy.
Ophthalmic Biometry
- Measuring the physical parameters of the globe is required to determine the proper IOL power
- The procedure can be accomplished using the IOL Master manufactured by Carl Zeiss Meditec
All of the diagnostic test results confirmed the initial diagnosis of clinically significant cataract in both eyes.
According to Current Procedural Terminology, when eye doctors perform ophthalmological examinations, the complexity of medical decision-making is not separated from the examining techniques used. As a guideline to assist eye doctors in enhancing their medical decision-making skills, consider that the complexity of medical decision-making involves three components.
The first component concerns the number of possible diagnoses and treatment options that must be considered. The diagnosis of the presence of a cataract is low complexity. Determining the clinical significance of the cataract can be more complex and involves a thorough understanding and evaluation of the entire eye and vision system. As there is only one treatment option, the complexity regarding the treatment of cataract primarily involves the determination of the need for surgical removal to restore functional vision.
The second component concerns the amount and complexity of medical records and diagnostic tests that have to be obtained, reviewed and analyzed. In addition to an eye examination, this visit required the review and analysis of a subjective refraction, a specular microscopy evaluation and the calculation of IOL power using optical coherence biometry.
Third, the complexity of medical decision-making is affected by the risk of significant complications and/or morbidity associated with cataracts and the risks involved in any treatment options. This patient’s cataract condition was classified as a moderate problem where the risk of significant, irreversible vision loss without treatment was very low. However, medical decision-making is complicated in the actual decision to monitor the condition or recommend surgical intervention. This decision is multifactorial and involves consideration of ocular and vision data, individual patient vision needs, patient motivation, ability of the eye to withstand surgical stresses and the motivation or desire of the patient to proceed with a surgical option.
Treatment Guidelines
Cataracts are not a medically treatable process. Patients will commonly ask if there is anything they can do to stop or delay cataract development. While some studies show anti-glycation compounds and high dose anti-oxidants can reduce the normal process of cataract development, the science behind this remains to be established. The only guaranteed treatment is surgical removal when the impact on the patient’s functional vision has an impact on their quality of life or activities of daily living. Once that decision is made, the patient is either monitored or scheduled for surgery.
Cataract surgery is most often an option for the patient. Except in the cases of spherophakia or advanced cataract development, the cataract rarely poses any risk of harm to the eye. To that end, no patient has to agree to cataract surgery. The doctor is often placed into a more tenuous situation when a patient’s vision is reduced to a point that, despite their refusal for surgical correction, does not qualify the patient to legally or safely drive. In those cases, the doctor is obligated to explain to the patient that they are not legal to continue driving and recommend they no longer do so until their vision is corrected.
In the age of modern cataract surgery where the benefit is high and the risks are low, it should be a rare occurrence where a properly educated patient would refuse surgery.
Treatment Program
The patient was counseled regarding the nature of her disease and given the option to proceed with surgery. The patient desired to have their vision restored and the patient was scheduled for surgery, standard single focus intraocular lenses, left eye first. The maximum interval between the preoperative evaluation and surgery should not exceed three months. Patient should be educated to contact their optometrist or ophthalmologist if there is any change in vision between the preoperative evaluation and the time of surgery.
Cataract surgery is indicated when the following criteria are met
Standardized measurement of the patient’s visual function is completed, the results of which show cataract surgery will improve visual function commensurate with the risk of surgery.
- Impaired visual function
- 20/40 or worse Snellen acuity
- Decreased ability to carry out activities of daily living
- Decreased ability to carry out vocational requirements
- Glare symptoms are not specific for indications for surgery unless they cause interference with activities of daily living (glare testing is not required)
- The patient has undergone a comprehensive evaluation, typically including an A-scan or ophthalmic biometry
- The patient has been educated with the risks and benefits of cataract surgery
Cataract surgery is contraindicated in the following situations
- Glasses or other visual aids provide satisfactory or functional vision
- Patient’s lifestyle is not compromised by the cataracts
- Coexisting medical conditions would contraindicate intraocular surgery
- Cataract surgery would not improve vision
- Informed consent is not obtained
Based on patient history, the nature of the presenting problem, and my own clinical judgement this patient needed an evaluation of the complete visual system.
- Perform the eye examination that is medically necessary
- Provide the diagnostic tests or services that are medically necessary
- Properly document the services provided
- Code from the documentation
- Report the services to the payor
Physicians Quality Reporting System
PSRS Measure 130: Current Medications with Name, Dosage, Frequency and Route Documented – CPT code G8427
This measure applies to patients 18 years and older. The measure should be reported on the day of the examination and can be used with any diagnosis code.
PQRS Measure 226: Patient screened for tobacco use and identified as a non-user of tobacco – CPT code 1036F
This measure applies to patients 18 years and older. The measure should be reported on the day of the examination and can be used with any diagnosis code.
Multiple Procedure Payment Reduction
Effective January 1, 2013, there is a small reduction in payment from Medicare if certain multiple procedures are billed on the same day. The fee for the technical component of the diagnostic test for the second and subsequent tests will be reduced by 20%. The second diagnostic test and subsequent tests should be reported with a -51 modifier. Professional services such as gonioscopy, extended ophthalmoscopy and provocative glaucoma testing are excluded from this policy. Visual evoked potential testing is excluded from this policy.
Modifier 51
This modifier is used to identify the secondary procedure or when multiple procedures are performed on the same day by the same provider. List the major primary procedure first and append the modifier to the subsequent procedure. The primary procedure is the one with the highest dollar value.
| Diagnosis Code | Procedure Code | Modifier | Quantity | Payor | Amount Allowed |
| H25.013 - Cortical age-related cataract, bilateral | 92014 - Medical eye examination | 1 | Medicare | 127.03 | |
| H25.013 - Cortical age-related cataract, bilateral | 92136 - Optical coherence biometry | 1 | Medicare | 94.54 | |
| H18.51 - Endothelial corneal dystrophy | 92286 - Specular microscopy | 51 | 1 | Medicare | 35.81 |
| H25.013 - Cortical age-related cataract, bilateral | G8427 - Current medications documented | 1 | Medicare | 0.00 | |
| H25.013 - Cortical age-related cataract, bilateral | 1036F - Patient screened for tobacco use | 1 | Medicare | 0.00 | |
| Total | $257.38 |
H25.013
Cortical age-related cataract,
bilateral
366.15
Cortical senile cataract
92136
Ophthalmic biometry
with IOL power calculation
76519
A-Scan with IOL power calculation
92286
Specular endothelial microscopy




 Print | Share
Print | Share