Case Report ID: 18
Title
Primary Optic Atrophy
Category
Posterior Segment Disease (1)
Description
This case presents the diagnosis and treatment of primary optic atrophy with an unknown etiology.
Optic atrophy is not a specific disease, but a clinical sign of one of several disease processes. The condition may be either primary or secondary and is the endpoint of any disease process that causes axon degeneration in the retinogeniculate neural pathway.
Optic atrophy is commonly associated with the following conditions:
- Glaucomatous optic neuropathy
- Hereditary optic neuropathies
- Intracranial trauma
- Compressive lesions in the brain (e.g., tumor or aneurysm)
- Metabolic optic neuropathies (e.g., toxic or nutritional neuropathy, juvenile diabetes)
- Post inflammatory atrophy (e.g., optic neuritis or Devic disease)
- Circulatory optic neuropathies (e.g., central artery occlusion, cranial arteritis, carotid artery occlusion)
Case Report
- A 44-year-old black male presents for a “routine” eye examination
- Case history revealed no specific complaint other than a slight decrease in vision in the left eye over the past several years
- Patient used over-the-counter reading glasses for near vision and wanted to know if new eyeglasses would improve his vision
Conclusion
This case demonstrates the importance of investigating a patient’s vague visual complaints and the importance of performing confrontation visual fields and a dilated fundus examination in patients that present for “routine” eye care.
History of Present Illness
- Associated Signs and Symptoms: none
- Location: vision is worse in the left eye
- Duration: past 5 years
- Quality: “vision is a little dim in the left eye”
- Context: n/a
- Severity: mild
- Timing: staying the same
- Modifier: none
Review of Systems
The patient reported he was in good health and taking no medications.
Past, Family and Social History
He worked as a maintenance man and reported no unusual head trauma or work-related accidents. In his youth, he was a bull rider in local rodeos and reported multiple falls and injuries associated with this activity.
Best Corrected Distance Visual Acuity
- 20/20 in the right eye
- 20/25 in the left eye
Normal Examination Findings
- Mental status
- General medical observation
- Pupils
- Basic sensorimotor examination
- External examination
- Adnexal examination
- External ocular examination with biomicroscopy
Intraocular Pressure Measurements
- 15 mm Hg in the right eye
- 14 mm Hg in the left eye
Gross Visual Fields
- Confrontation testing revealed a severe constriction in all meridians of gaze in the left eye
Ophthalmoscopy
The evaluation of the retina and the optic nerve was abnormal.
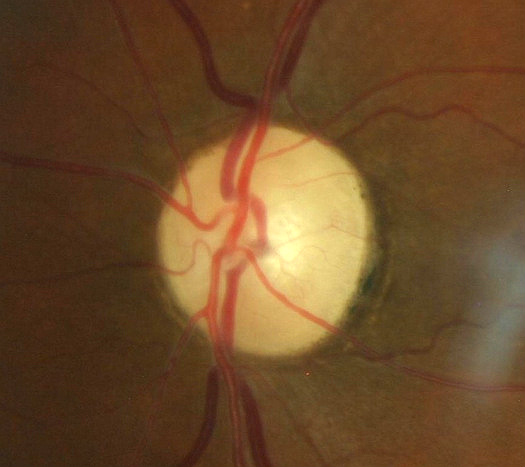
- Healthy optic disc in the right eye
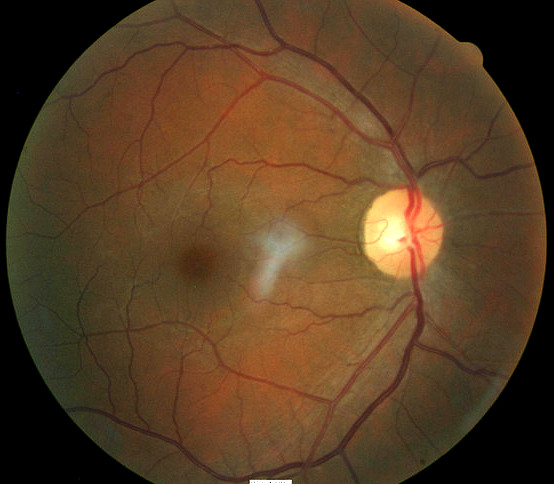
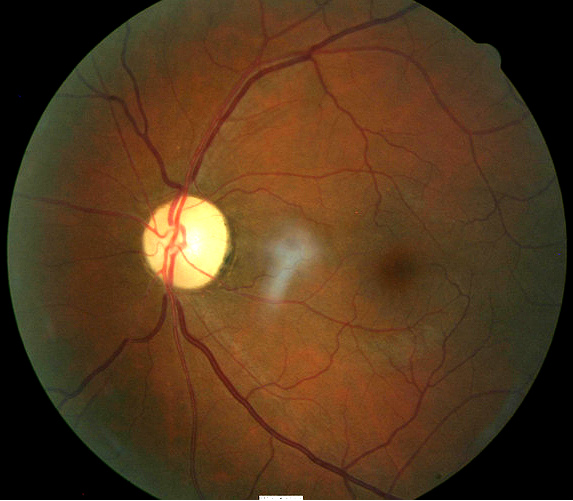
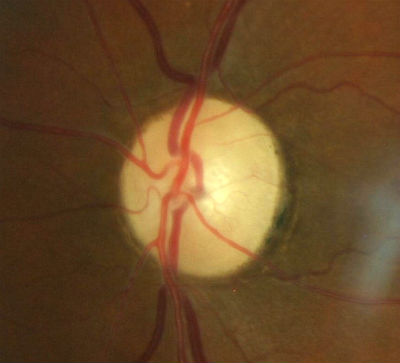
- Changes in coloration of the left optic disc
- Pallor of the entire optic disc
- Thinning/narrowing of the small blood vessels on the optic disc surface
Clinical Diagnosis
The clinical diagnosis is a determination based on the knowledge obtained from the patient’s medical history and the results of the eye examination alone, without the benefit of diagnostic tests or procedures.
The patient’s clinical diagnosis is primary optic atrophy based on the following clinical findings:
- Pallor of the optic disc in the left eye
- Abnormal confrontation visual field in the left eye
- Decreased visual acuity in the left eye
Treatment Plan
To gather the information required to treat primary optic atrophy, a diagnostic and treatment program is initiated.
- Determination of different types of diagnoses
- Selection of one or more treatment options
Primary optic atrophy is a condition where the doctor must determine whether the etiology or pathologic versus nonpathologic. After a clinical diagnosis has been determined, the diagnostic process continues with a process that involved the indentification and exclusion of differential diagnoses. The differential diagnosis process allows the eye doctor to distinguish between two or more disease with similar signs and symptoms by systemically comparing their signs and symptoms.
Differential Diagnoses
The list of possible diseases would include any pathology in which optic disc pallor is a clinical finding:
- Glaucoma
- Axial myopia
- Optic disc drusen
- Optic nerve pit
- Scleral crescent
- Tilted optic disc
- Myelinated nerve fibers
- Optic nerve hypoplasia
If the patient’s history does not match any of these conditions, a diagnostic and treatment program must be initiated. The decision to order and perform additional diagnostic testing is totally based on the concept of medical necessity which can only be determined by the examining optometrist or ophthalmologist.
Ordering Diagnostic Tests
- Refraction
- Visual field examination
- Retinal nerve fiber layer scan
- Extended color vision examination
- Visual evoked potential testing
- Electroretinogram
The decision to order and perform additional testing is totally based on the concept of medical necessity which can only be determined by the examining optometrist or ophthalmologist.
Refraction
- Measuring visual acuity is a method of evaluating functional vision loss
- Primary optic atrophy, especially in more severe presentations, can produce a loss in visual acuity
- 20/20 distance acuity in the right eye
- 20/25 distance acuity in the left eye
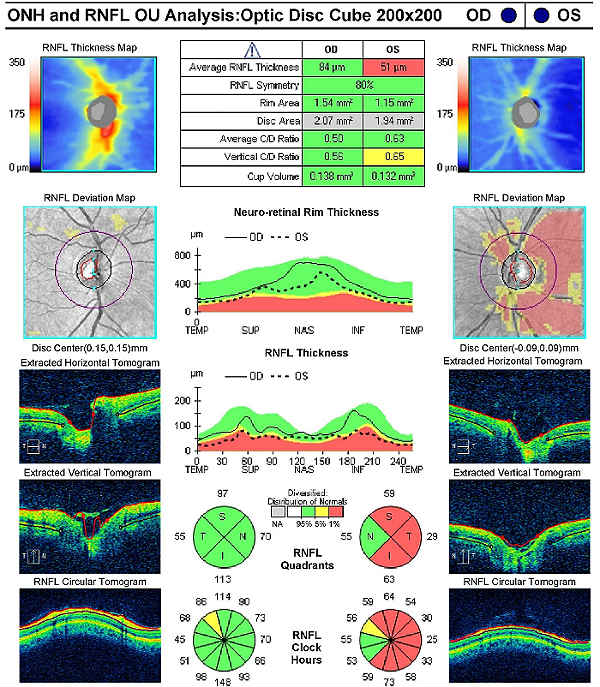
Retinal Laser Scan
- Measuring the average retinal nerve fiber layer thickness provides an overall assessment of retinal nerve fiber layer health
- The procedure can be accomplished by using the CIRRUS OCT manufactured by Carl Zeiss Meditec or other retinal scanning lasers
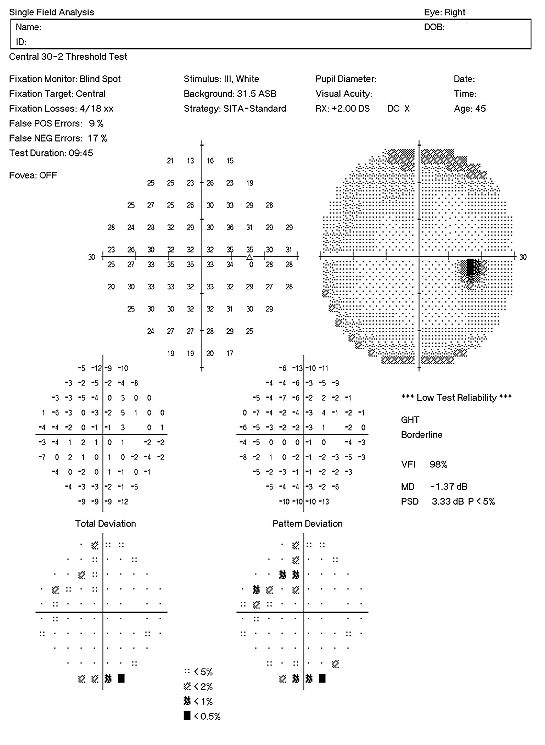
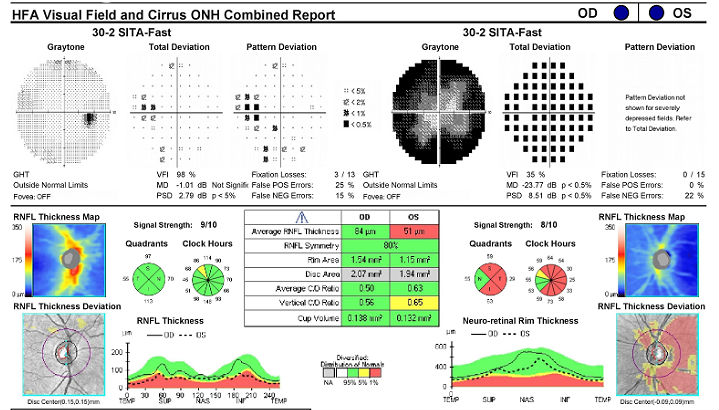
Visual Field Examination
- Automated threshold perimeters measure the visual field by plotting the threshold luminance value of the patient in various locations in the visual field
- The luminance of the light stimulus is represented by non-specific units of measurement called decibels (dB)
When a neuro-ophthalmic condition is suspected, the most useful testing strategy is the 30-2 threshold visual field. Common findings include enlargement of the blind spot, paracentral scotomas, constriction of isopters, altitudinal defects, and bitemporal defects.
Right Eye
- Mild loss of retinal sensitivity
- Scattered paracentral scotomas
- Low test reliability
Left Eye
- Severe loss of retinal sensitivity
- Double arcuate scotoma temporally
- Good test reliability
FORUM Image Management System
- Forum data/image management system is manufactured by Carl Zeiss Meditec
- The system enables you to connect all your diagnostic systems into a central server-based software
- From this centralized database, you will be able to access all the diagnostic images in your exam room or from a remote location
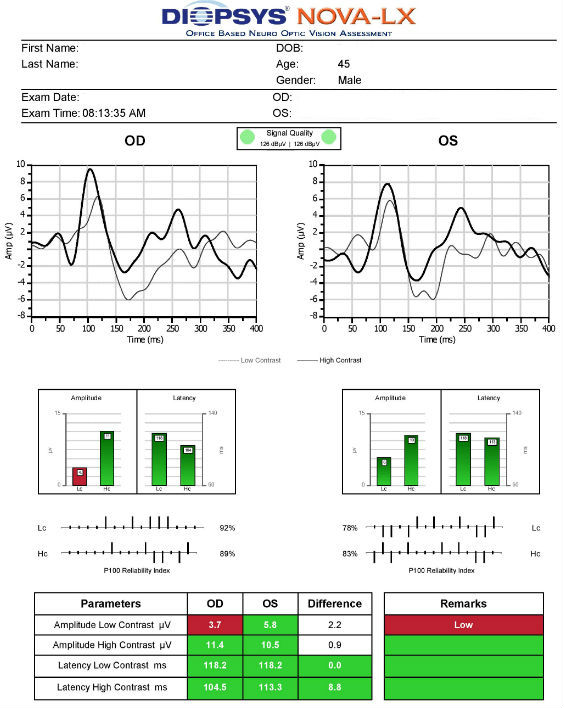
Visual Evoked Potential
- Visual evoked potential testing evaluates the integrity of the afferent visual sensory system
- The procedure can be accomplished by using the NOVA-LX VEP Testing Device manufactured by DIOPSYS
In optic nerve disease, the amplitude of the visually evoked response is decreased and the latency is delayed compared to the normal eye. In cases of optic atrophy due to compressive lesions, the amplitude of the response is reduced while the latency tends to be normal.
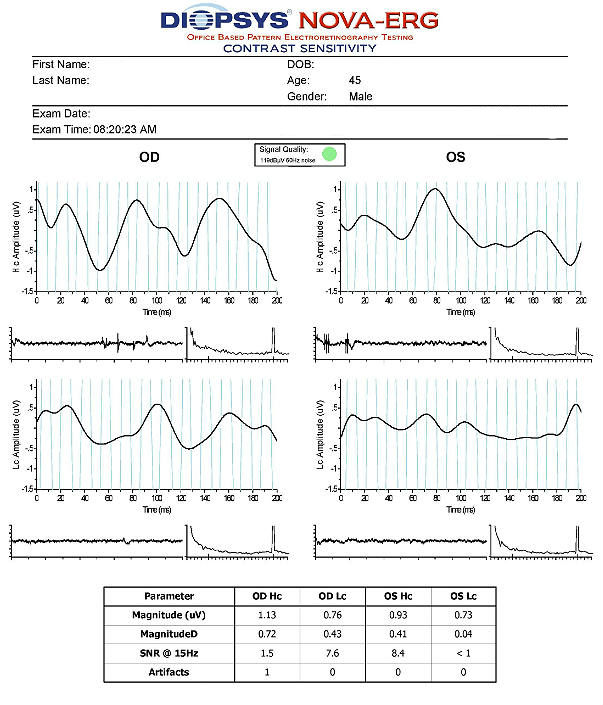
Electroretinography
- Electroretinogram testing evaluates the integrity of the retina
- The procedure can be accomplished using the NOVA-ERG Testing Device manufactured by DIOPSYS
- Specialized pattern electroretinogram (PERG) test uses a contrast-reversing pattern for the stimulus to produce information about ganglion cell function
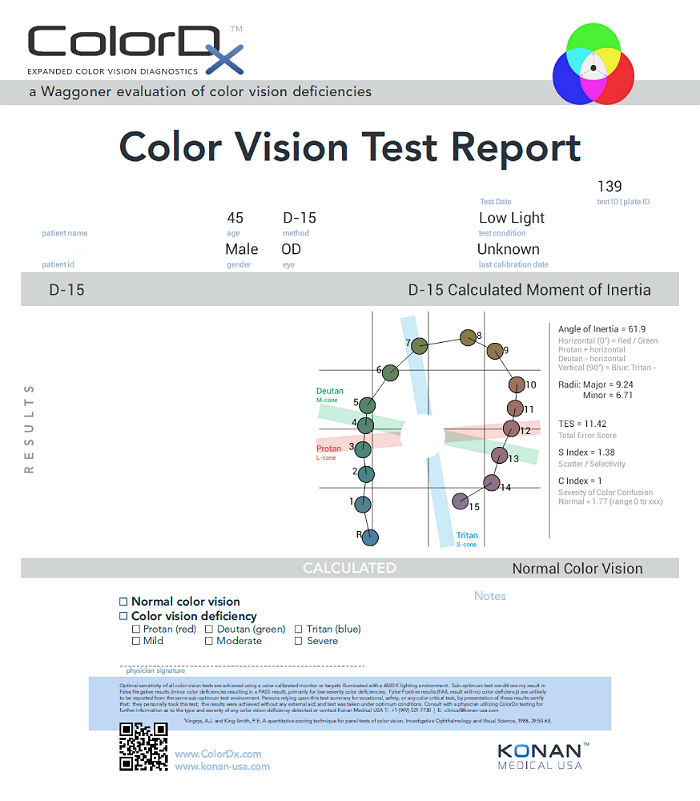
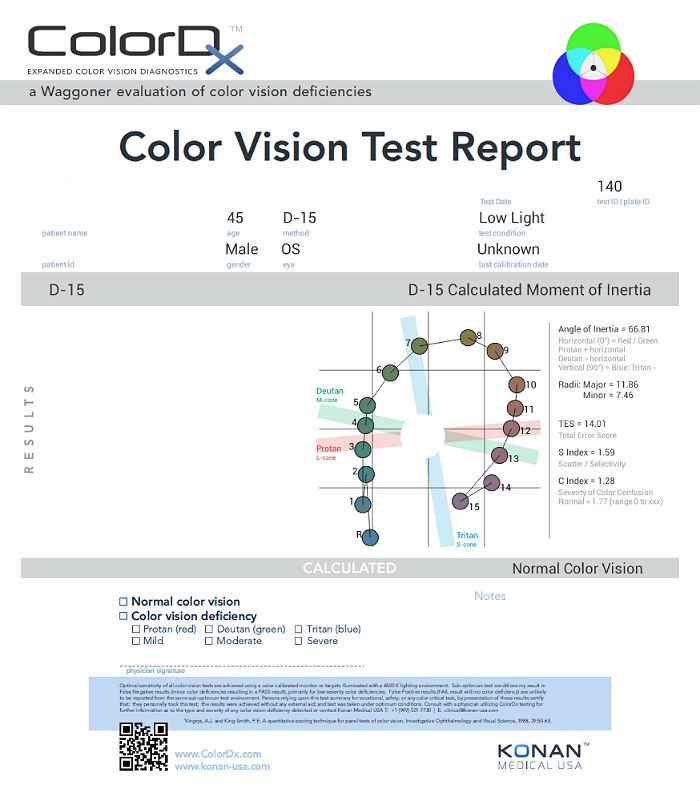
Extended Color Vision Examination
An extended color vision examination measures the combined function of the retina, the optic nerve and the intracranial visual pathway and is used clinically to detect or monitor color vision loss due to disease at any of these locations. Extended color vision testing divides people into two groups.
- The first group consists of people with normal color vision and slight color deficiency
- The second group consists of people with moderate or severe color deficiency
One of the most common tests performed in clinical practice is the Farnsworth D15. When performed on Konan Medical’s ColorDx software, the test is presented as fifteen colored bars and one fixed bar on an Android tablet. The hue of each bar has been chosen so that the adjacent bars have approximately equal hue differences. When the bars are arranged in order, they form a hue circle. As a result, errors in hue discrimination can be made across the hue circle.
Patients with normal color vision usually make no error but may make one or two minor transposition errors, as do those with mild color vision deficiency. Patients with more advanced color deficiency make some or more of the following errors:
- They place colors that lie on the opposite side of the hue circle next to colors that lie on their confusion locus (e.g., diametrical errors)
- Two or more diametrical crossing errors indicates a “failed” test
- If diametrical crossing errors are made, the orientation of the crossing produces a diagnosis of protan, deutan, or tritan color vision deficiency
- This patient’s color vision was normal in each eye.
Systemic Evaluation
Eye doctors should consider a systemic evaluation in cases of unexplained optic atrophy. A typical investigative protocol would include the following tests:
- MRI of the brain and orbit with contrast
- Carotid Doppler ultrasound study
- Cardiovascular examination
- Sarcoid examination
- Blood glucose level
- Vitamin B-12 levels
- Antinuclear antibody levels
- Homocysteine levels
- Antiphospholipid antibodies
- Venereal Disease Research Laboratory (VDRL)
Enzyme-linked immunosorbent assay (ELISA)
- Toxoplasmosis
- Rubella
- Cytomegalovirus
- Herpes simplex virus
Primary care eye doctors should communicate as specifically as possible regarding their suspicion of systemic involvement in a patient presenting with primary optic atrophy. This can and should be as detailed as recommending specific laboratory analysis and/or imaging based on the suspected systemic disease. In this presentation, based on the patient’s age, ethnicity, gender and past history, a high suspicion existed for traumatic optic neuropathy as the cause of the atrophy.
Magnetic Resonance Imaging (MRI)
Four days after the eye examination, an MRI without and with intravenous gadolinium was performed at a nearby imaging center. There was no prior examination for comparison.
Radiologist’s Findings:
- There is no restricted diffusion to suggest recent infarction
- There is no intracranial mass effect or midline shift
- The ventricular system, sulci, and cisterns are normal in size and morphology
- No brain parenchymal signal abnormality or abnormal enhancement is demonstrated
- No orbital mass or optic nerve enhancement is demonstrated
- There is no blooming artifact within the breain parenchyma on the gradient images to suggest blood products
- Minimal mucosal thickening involves the paranasal sinuses
Radiologist’s Impression:
- No intracranial abnormality demonstrated
All the diagnostic test results confirmed the clinical diagnosis of primary optic atrophy. Photographic documentation of the optic disc would be an additional medically necessary test that could be obtained at any follow-up evaluation.
According to Current Procedural Terminology, when eye doctors perform ophthalmological examinations, the complexity of medical decision-making is not separated from the examination techniques used. As a guideline to assist eye doctors in enhancing their decision-making skills, consider that the complexity of medical decision-making involves three components.
The first component concerns the number of possible diagnoses and treatment options that must be considered. Determination of the diagnosis of primary optic atrophy involves the determination of structural damage to the optic disc and the visual pathway, typically after some functional loss of vision.
The second component concerns the amount and complexity of medical records and diagnostic tests that have to be obtained, reviewed and analyzed. In addition to the eye examination, this visit required the review and analysis of a subjective refraction, a retinal laser scan, a threshold visual field, an electroretinogram, a visual evoked potential test and an extended color vision examination.
Third, the complexity of medical decision-making is affected by the risk of significant complications and/or morbidity associated with primary optic atrophy and the risks involved in any treatment options. This patient’s optic nerve condition was classified as a significant problem where the risk of central vision loss without treatment was possible. In addition, the treatment plan will involve ordering laboratory tests, imaging of the brain, coordination of care with the patient’s primary care physician as well as continued monitoring of the optic atrophy.
Treatment Guidelines
There is no local (retinal) treatment for primary optic atrophy so no referral to a retinal specialist is warranted.
The key to proper treatment is determining the etiology of the optic atrophy. For example, early diagnosis and aggressive treatment can prevent further damage in patients with compressive and toxic neuropathies. Intravenous steroids are helpful in some cases of optic neuritis or anterior ischemic optic neuropathy.
Treatment Program
An MRI of the brain with contrast was ordered to rule out various pathologies.
Next visit scheduled for 10 days.
Discussion
This case demonstrates several key aspects of providing eye care that optometrists and ophthalmologists encounter everyday. First and foremost, it demonstrates the key role of primary care eye doctors in the detection of serious, sight-threatening complications of neurologic or systemic disease. Second, it demonstrates how unwise it is to rely on patients to self-diagnose and report a chief complaint that makes our job easier.
Initially, it seemed as though this patient had no chief complaint and simply presented to the office for a “routine” eye examination for the purpose of receiving new prescription eyeglasses. However, after additional case history was obtained, the decreased vision in the left eye was revealed to be the true chief complaint. This points out the age-old addage that “the case history never ends”. To that end, the true reason for the visit or chief complaint may be hidden in what the patient wants us to hear or, more commonly, not elicitied initially by the patient because patients are not doctors and do not know what to tell us. It is the attending physicians job to ascertain what the true reason for the visit is, even if that may not become apparent until well into the examination process.
From a medicolegal perspective, all medical insurance plans require a chief complaint for services to be classified as medically necessary and will not pay for examinations where the purpose of the examination is to receive prescription eyeglasses. That being said, it is the responsibility of the eye doctor (not the staff) to document the patient’s medical and ocular history and to perform coverage decision-making regarding a patient’s insurance if necessary.
Based on patient history, the nature of the presenting problem, and my own clinical judgement this patient needed an evaluation of the complete visual system.
- Perform the eye examination that is medically necessary
- Provide the diagnostic tests or services that are medically necessary
- Properly document the services provided
- Code from the documentation
- Report the services to the payor
| Diagnosis Code | Procedure Code | Modifier | Quantity | Payor | Amount Allowed |
| H47.212 - Primary optic atrophy, left eye | 92004 - Medical eye examination | 1 | United Healthcare | 124.26 | |
| H47.212 - Primary optic atrophy, left eye | 92015 - Refraction | 1 | United Healthcare | 42.94 | |
| H47.212 - Primary optic atrophy, left eye | 92133 - Retinal laser scan | 1 | United Healthcare | 49.78 | |
| H47.212 - Primary optic atrophy, left eye | 92083 - Visual field examination | 1 | United Healthcare | 73.34 | |
| H47.212 - Primary optic atrophy, left eye | 92275 - Electroretinography | 1 | United Healthcare | 118.56 | |
| H47.212 - Primary optic atrophy, left eye | 95930 - Visual evoked potential | 1 | United Healthcare | 106.02 | |
| H47.212 - Primary optic atrophy, left eye | 92283 - Color vision examination | 1 | United Healthcare | 43.69 | |
| Total | $558.59 |
H47.212
Primary optic atrophy, left eye
92015
Refraction
92250
Fundus photography
92083
Visual field examination
95930
Visual evoked potential
92283
Color vision examination
92133
Retinal laser scan
92275
Electroretinography




 Print | Share
Print | Share