ICD-10 Diagnosis Codes:
T26.61XA–Corrosion of cornea and conjunctival sac,
right eye, Initial encounter
T26.61XD–Corrosion of cornea and conjunctival sac,
right eye, Subsequent encounter
T26.61XS–Corrosion of cornea and conjunctival sac,
right eye, Sequela
T26.62XA–Corrosion of cornea and conjunctival sac,
left eye, Initial encounter
T26.62XD–Corrosion of cornea and conjunctival sac,
left eye, Subsequent encounter
T26.62XS–Corrosion of cornea and conjunctival sac,
left eye, Sequela
Title
Alkaline Chemical Burn of Cornea and Conjunctival Sac
Category
Burn Confined To Eye And Adnexa
Description
Chemical agents that have a pH greater than 7 are alkaline and have a high likelihood for ocular damage.
Alkaline chemical burns can cause minor or irreversible damage to the ocular surface.
- Cornea
- Limbus
- Conjunctiva
The prognosis for recovery depends upon the following factors:
- Type of chemical
- Severity of the burn
- Type of treatment
- Intensity of treatment
Chemical burns damage the ocular surface through several mechanisms:
- Damage to the corneal epithelium
- Damage to the corneal stroma
- Damage to the limbus
- Conjunctivalization
Damage to the Corneal Epithelium
The corneal epithelium is involved in the following functions:
- Maintaining the integrity of the optical surface
- Maintaining stromal hydration
- Regulating the metabolism of stromal keratocytes
Damage to the Corneal Stroma
Keratocytes are required to maintain the corneal stroma because they synthesize the collagen required to regenerate the tissue. If the ciliary body is affected by the chronic inflammation associated with chemical burns, altered aqueous chemistry may lead to compromised keratocyte synthesis of collagen.
Damage to the Limbus
Limbal stem cells are found in the perilimbal conjunctiva. They create a barrier function against conjunctival epithelial cells and keep them from moving onto the cornea. If a chemical burn damages or destroys the limbus, it produces a condition called limbal stem cell deficiency.
Conjunctivalization
In patients with limbal stem cell deficiency, cells from the bulbar conjunctiva invade the cornea and produce the following abnormal findings:
- Chronic inflammation
- Neovascularization
- Loss of stromal transparency
- Stromal scarring
- Loss of vision
Natural History of Chemical Burns
After the ocular surface has been damaged from a chemical burn, the cornea attempts to repair itself through multiple mechanisms:
- Epithelial regrowth and migration
- Collagen synthesis and degradation
- Activation and migration of keratocytes
The clinical course of the chemical burn recovery process can be divided into three phases:
Acute Repair Phase
- Initial injury through day 7
- First inflammatory wave begins
- Reepithelialization begins if there is no limbal ischemia
- Treatment is directed at encouraging epithelial migration and controlling inflammation
- bandage contact lenses
- topical steroids
- use kerato-friendly topical antibiotics
Intermediate Repair Phase
- Days 7 through 21 after the initial injury
- Grade I burns are usually reepithelialized
- Second inflammatory wave begins
- Grade II burns may have persistent epithelial defects
- Grades III and IV burns will have little to no reepithelialization
- Collagenase activity peaks in the corneal stroma
- Treatment is directed at encouraging collagen synthesis and minimizing collagenase activity
Late Repair Phase
- After day 21 of the initial injury
- Grade I burns are usually reepithelialized
- Grade II burns may have focal limbal ischemia and focal conjunctivalization
- Grade III burns usually demonstrate delayed reepithelialization and conjunctivalization
- Grade IV burns will have a denuded cornea and possible corneal melt
The main goal of a diagnostic examination in a patient with a chemical burn is to accomplish the following:
- Neutralize the pH of the ocular surface
- Identify the chemical agent
- Control the inflammatory response
- Prevent infection
- Restore normal ocular surface anatomy
Patient History
Patients with chemical burns will present with some or all of the following abnormal signs and symptoms:
- Ocular redness
- Ocular pain
- Foreign body sensations
- Photophobia
- Ptosis
- Decreased vision
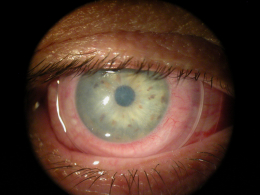
External Ocular Examination with Biomicroscopy
- Loss of the corneal epithelium
- Loss of stromal transparency
- Loss of conjunctival epithelium
- Loss of conjunctival vasculature
DIAGNOSTIC TESTS
External Ocular Photography
- To help plan a treatment program
- Document the delivery of treatment
- Document the response to treatment
Chemical burns may be classified based on the extent of the injury to the ocular surface.
- Corneal appearance
- Extent of limbal ischemia
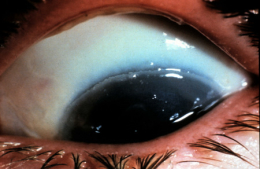
Grade I Chemical Burn
- Limbal stem cells not affected
- May be a large defect in the corneal epithelium
- Underlying corneal stroma remains clear
- Anterior segment structures easily visualized
- Excellent prognosis for full recovery
Grade II Chemical Burn
- Partial limbal ischemia (less than one-third of the limbus with stem cell damage)
- May be a large defect in the corneal epithelium
- May be a loss of stromal transparency
- Anterior segment structures typically visible
- Favorable prognosis for full recovery, but some long-term complications are possible
- persistent epithelial dysfunction
- conjunctivalization
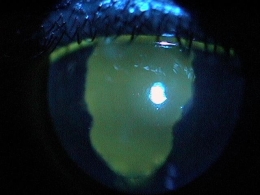
Grade III Chemical Burn
- Extensive limbal ischemia (one-third to one-half of the limbus with stem cell damage)
- May be a large defect in the corneal epithelium
- Loss of stromal transparency
- Visualization of anterior segment structures is limited
- Prognosis for full recovery is guarded
- Surgical treatment options may be required for maximum recovery
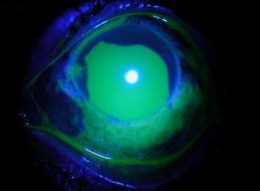
Grade IV Chemical Burn
- Severe limbal ischemia (greater than one-half of the limbus with stem cell damage)
- Complete loss of the corneal epithelium
- Focal loss of the conjunctival epithelium
- Loss of stromal transparency
- Unable to visualize anterior segment structures
- Prognosis for full recovery is poor
Because they damage the eye in different ways, it is important to know whether the insulting chemical agent was an acid or a alkaline.
Acid Chemicals
- Have a pH below 7
- As the pH moves towards 2.5, the risk for irreversible damage to the ocular surface increases
- When exposed to acid chemicals, corneal proteins in the stroma bind to the acids to create a barrier function
- protein barrier limitis further penetration of the acid
- superficial injury is most common clinical presentation
- nonprogressive injury is a common clinical features
Alkaline Chemicals
- Have a pH above 7
- Also called “base” chemicals
- Risk of irreversible damage to the ocular surface is high
- As the pH increases, the corneal barrier function is sloughed away
- loss of barrier function leads to further penetration of the alkaline
- increases the risk of damage to uveal structures
The goal of treating a chemical burn is to restore the health of the ocular surface.
Neutralization of pH
The initial treatment option is to neutralize the pH of the patient’s ocular surface by irrigating the chemical out of the eye with a balanced saline solution.
Inflammation
Chemical burns have two waves of inflammation that occur after the exposure.
First Inflammatory Wave
- 12 to 24 hours after exposure
- Immune system response cannot be prevented
- Aggressive treatment with high-dose steroids
Second Inflammatory Wave
- Typically begins at day 7
- Associated with corneal repair and degradation
- Most intense immune response occurs between days 14 through 21
- Prevention of corneal melt is a primary therapeutic goal
Topical Pharmaceutical Treatment
Kerato-friendly antibiotics
- Polytrim ophthalmic solution — 1 drop three to four times per day until reepithelialization occurs
- Fluoroquinolones — 1 drop four times per day until reepithelialization occurs
Non-preserved artificial tears
- Promotes reepithelialization
Topical cycloplegics
- 1% cyclogyl three times per day for several days
- 5% homatropine twice daily for several days
Topical steroids
- xxx
- xxx
Although their is a risk of corneal melting with steroid use, the activation of stromal collagenases usually does not occur until 10 to 14 days after the burn. Because of this, the first week of treatment is the most important time to maximize steroid therapy, and then change the frequency to twice daily for several weeks after the first week of steroid treatment. Monitor the patient frequently.
Autologous or umbilical cord serum
- Promotes reepithelialization
- Consider during acute phase
- Has anti-inflammatory and anti-scarring properties
Topical chemical supplementation
- Promotes collagen synthesis
- Consider during acute phase
- Compensates for altered aqueous chemistry — 10% sodium ascorbate, 10% sodium citrate
Avoid nonsteroidal anti-inflammatory medications because they are not kerato-friendly and they lack the potency required to control burn-induced inflammation. Also, avoid phenylephrine and OTC vasoconstrictors because they may increase limbal ischemia.
Mechanical Treatment
Promotes reepithelialization
- Pressure-patch
- Bandage contact lens — In the acute phase, patients with Grades II through IV burns usually cannot tolerate bandage contact lens wear
Surgical Treatment
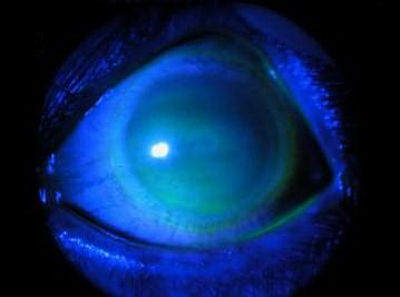
ProKera Amniotic Membrane Insert is a Class II medical device. It is composed of a cryopreserved amniotic membrane graft fastened to a thermoplastic 16mm symblepharon ring.
 |
ProKera Aminiotic Membrane Insert
|
Patient with chemical burn treated with ProKera Amniotic Membrane Insert
- Day 1 on the top row of images
- Day 5 on the bottom row of images
- Note the complete reepithelialization after only 5 days
1. Randleman, B. Ophthalmologic Approach to Chemical Burns. EMedicine/Medscape. 18 Sept 2014. http://emedicine.medscape.com/article/1215950-overview#showall. Last accessed November 16, 2014.
2. Hemmati, H. Colby, K. Treating Acute Chemical Injuries of the Cornea. American Academy of Ophthalmology. http://www.aao.org/publications/eyenet/201210/pearls.cfm. Last accessed November 16, 2014.
940.2
Alkaline chemical burn of cornea and conjunctival sac
92285
External ocular photography
92286
Specular endothelial microscopy
65778
Amniotic membrane placement
92071
Bandage contact lens




 Print | Share
Print | Share