ICD-10 Diagnosis Codes:
T15.11XA–Foreign body in conjunctival sac,right eye, initial encounter
T15.11XD–Foreign body in conjunctival sac, right eye, subsequent encounter
T15.11XS–Foreign body in conjunctival sac, right eye, sequela
T15.12XA–Foreign body in conjunctival sac, left eye, initial encounter
T15.12XD–Foreign body in conjunctival sac, left eye, subsequent encounter
T15.12XS–Foreign body in conjunctival sac, left eye, sequela
Title
Foreign Body in Conjunctival Sac
Category
Foreign Body On External Eye
Description
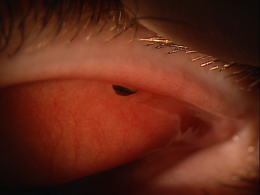
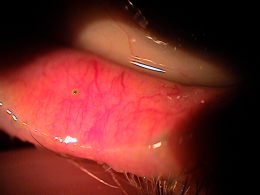
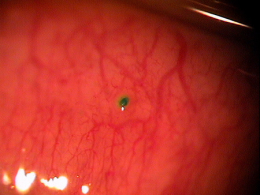
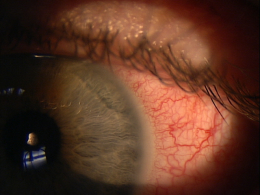
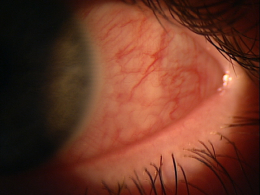
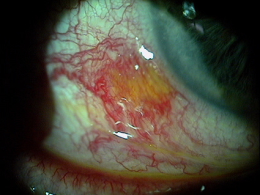
Conjunctival foreign body occurs when foreign material becomes lodged on or in the bulbar conjunctiva or the palpebral conjunctiva.
Structural Damage to the Eye
- Inflammatory cascade begins with damage to the conjunctival epithelium
- Inflamamtory mediators produce dilation of conjunctival blood vessels
- Mechanical trauma produces edema of the eyelids
- Conjunctival edema develops
Functional Damage to the Eye
- None
The main goal of the diagnostic evaluation in a patient with conjunctival foreign body is to accomplish the following:
- Ensure that a foreign body is the cause of the chief complaint
- Relieve ocular pain and discomfort
- Perform a preoperative assessment before removing the foreign body
Patient History
Patients with conjunctival foreign body may present with the following signs and symptoms:
- Blepharospasm
- Excessive watering of the eye
- Photophobia
- Conjunctival injection
- Mild foreign body sensation to severe pain
- Inability to localize the source of the foreign body sensation
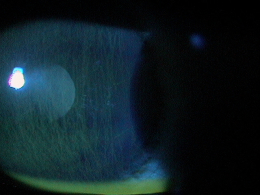
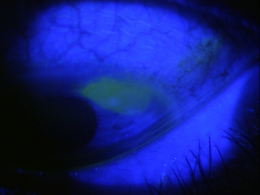
Clinical Appearance of the Cornea
- Look for epithelial damage
- Evaluate with fluorescein dye
There is no standard classification system for conjunctival foreign bodies. In a general sense, they can be classified by the type of material (e.g., glass, plastic, metal, wood, etc.) and/or by the depth of the object:
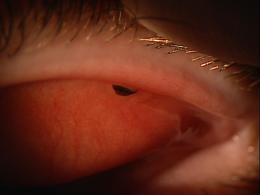
- Superficial foreign body
- Embedded foreign body
Patients with conjunctival abrasions and patients with conjunctival foreign bodies share a common history in that both groups have a history of recent ocular trauma.
The primary goals of treating a patient with a conjunctival foreign body includes the following:
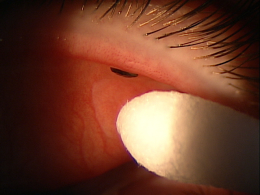
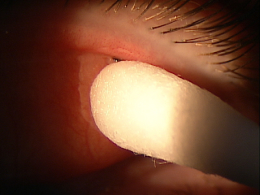
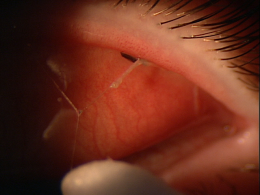
- Determine the number of foreign bodies (single or multiple)
- Identify the location (superior palpebral conjunctiva, bulbar conjunctiva, or inferior palpebral conjunctiva)
- Assess the degree of embeddedness of the foreign body
- Removal of foreign body
The use of topical ophthalmic anesthetic solution is avoided unless the patient is very uncomfortable and exhibits significant blepharospasm, or if the foreign body is substantially embedded. Topical anesthesia is avoided so that when the particle is located and removed, the patient will feel immediate relief, indicative that no foreign bodies remain in the eye.
On occasion the foreign body may irritate the cornea sufficiently so that, even following removal, the eye is still sensitive and uncomfortable. A thorough slit lamp examination with lid eversion will confirm that no other foreign bodies remain in the eye. If necessary, topical ophthalmic anesthetic solution is used to maximize patient comfort during the procedure.
1. Dahl A. Conjunctival Foreign Body Removal. Medscape. 8 Aug 2013. http://emedicine.medscape.com/article/1844102-overview. Last accessed August 8, 2014.
930.1
Foreign body in conjunctival sac
65205
Conjunctival foreign body removal
superficial removal
65210
Conjunctival foreign body removal
embedded removal
92285
External ocular photography
92071
Bandage contact lens




 Print | Share
Print | Share