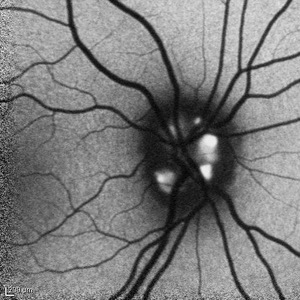
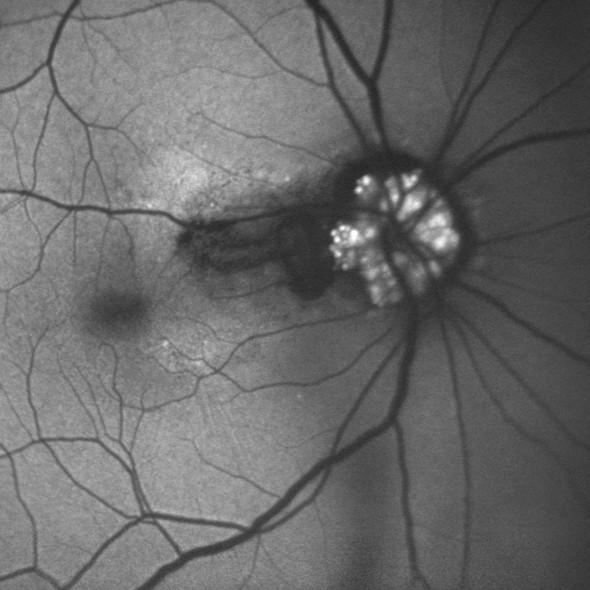
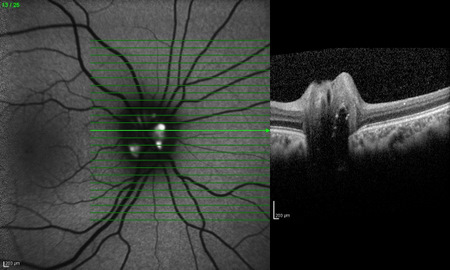
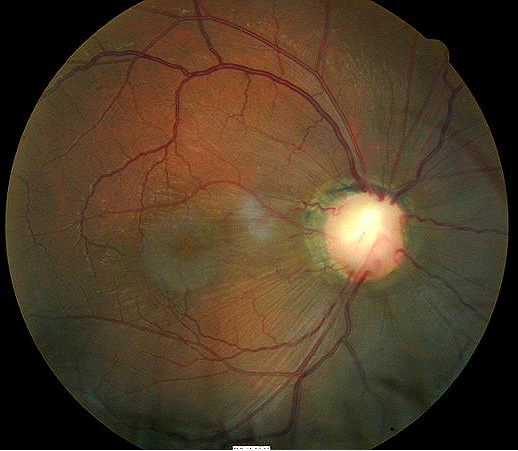
Optic nerve drusen imaged with Heidelberg
SPECTRALIS OCT using fundus autofluorescence
ICD-10 Diagnosis Codes:
H47.321–Drusen of optic disc, right eye
H47.322–Drusen of optic disc, left eye
H47.323–Drusen of optic disc, bilateral
Title
Optic Nerve Drusen
Category
Disorders Of The Optic Nerve And The Visual Pathways
Description
A condition involving superficial or buried calcium-like globular deposits anterior to the lamina cribrosa of the optic nerve head.
Optic nerve head drusen is characterized by the following clinical signs:
- Classic appearance involves bilaterally elevated optic discs with irregular or scalloped margins
- Small, refractile hyaline deposits visible on the surface of the optic disc and/or in the peripapillary area
- A small or nonexistent optic cup
- Unusual vascular branching patterns that stem from a central vessel core
- Drusen most often manifest on the nasal optic disc margin, but can be found within any part of the nerve head
 |
Common Names for Optic Nerve Drusen
|
Optic nerve drusen represent acellular laminated concretions, often partially calcified, possibly related to accumulation of axoplasmic derivatives of degenerating nerve fibers.
Structural Damage to the Eye
- Hyaline bodies confines anterior to the lamina cribrosa
- Drusen can compress the nerve fibers in the optic nerve head
- Drusen can compromise the vascular supply and lead to disc hemorrhages
- Drusen can be detected with fundus autofluorescence imaging as an increased signal is known as hyperautofluorescence
In extreme cases, drusen will produce the following abnormalities:
- Slowly developing optic atrophy
- Disruption of the juxtapapillary tissue
- Choroidal neovascular membrane formation
- Subretinal hemorrhage
- Disciform retinal scarring
 |
 |
Functional Damage to the Eye
- Mildly decreased visual acuity
- Reduced contrast sensitivity
- Abnormal color vision
- Visual field defects: inferonasal scotomas, arcuate scotomas, nasal steps, altitudinal defects, enlargement of the blind spot
The main goal of the evaluation of a patient with optic nerve drusen is to accomplish the following:
- Differentiate the condition from acquired optic disc edema
- Obtain baseline fundus photography and other diagnostic tests for future monitoring
- Prescribe a treatment program (e.g., patient education)
Patient History
Usually, patients with optic nerve drusen remain asymptomatic, and the condition is discovered only on routine ocular examination. Sometimes, the disease can present with mildly decreased visual acuity and visual field defects.
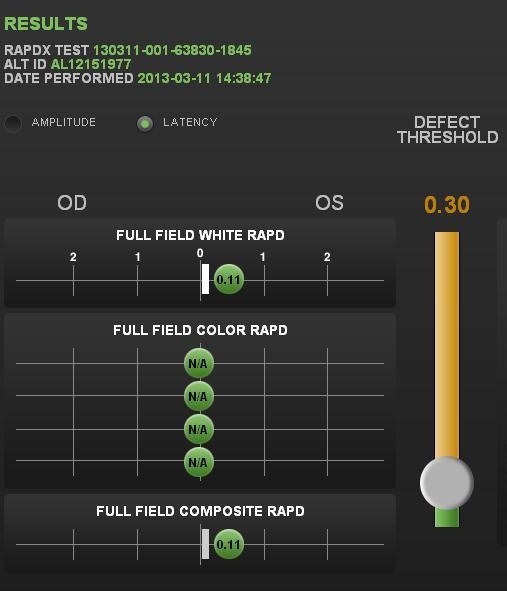
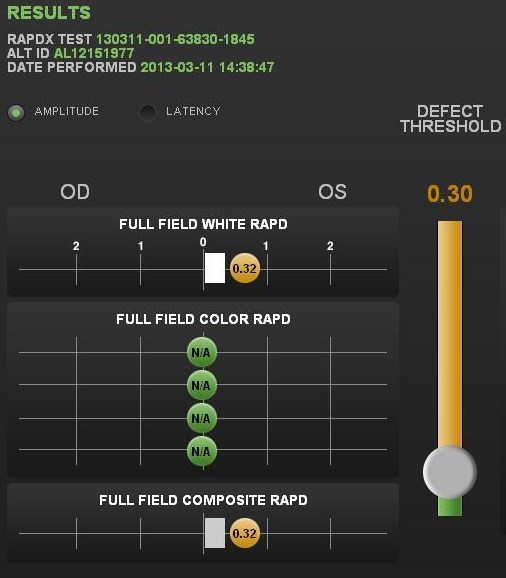
Pupillary Examination
An afferent pupillary defect may be noted if the condition is both significant and asymmetric.
- RAPDx automated pupillary examination
- Assessment of pupillary response amplitude and velocity
- Index of defect numbers above 0.30 are considered abnormal
- Abnormal amplitude in the left eye indicates an afferent pupillary defect is present
 |
 |
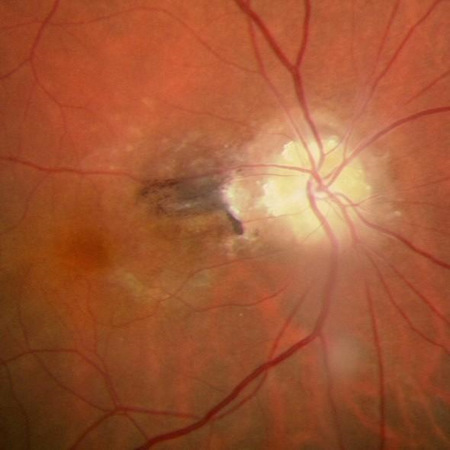
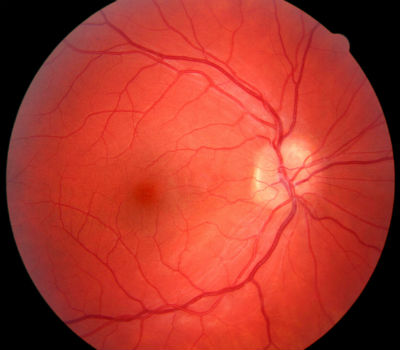
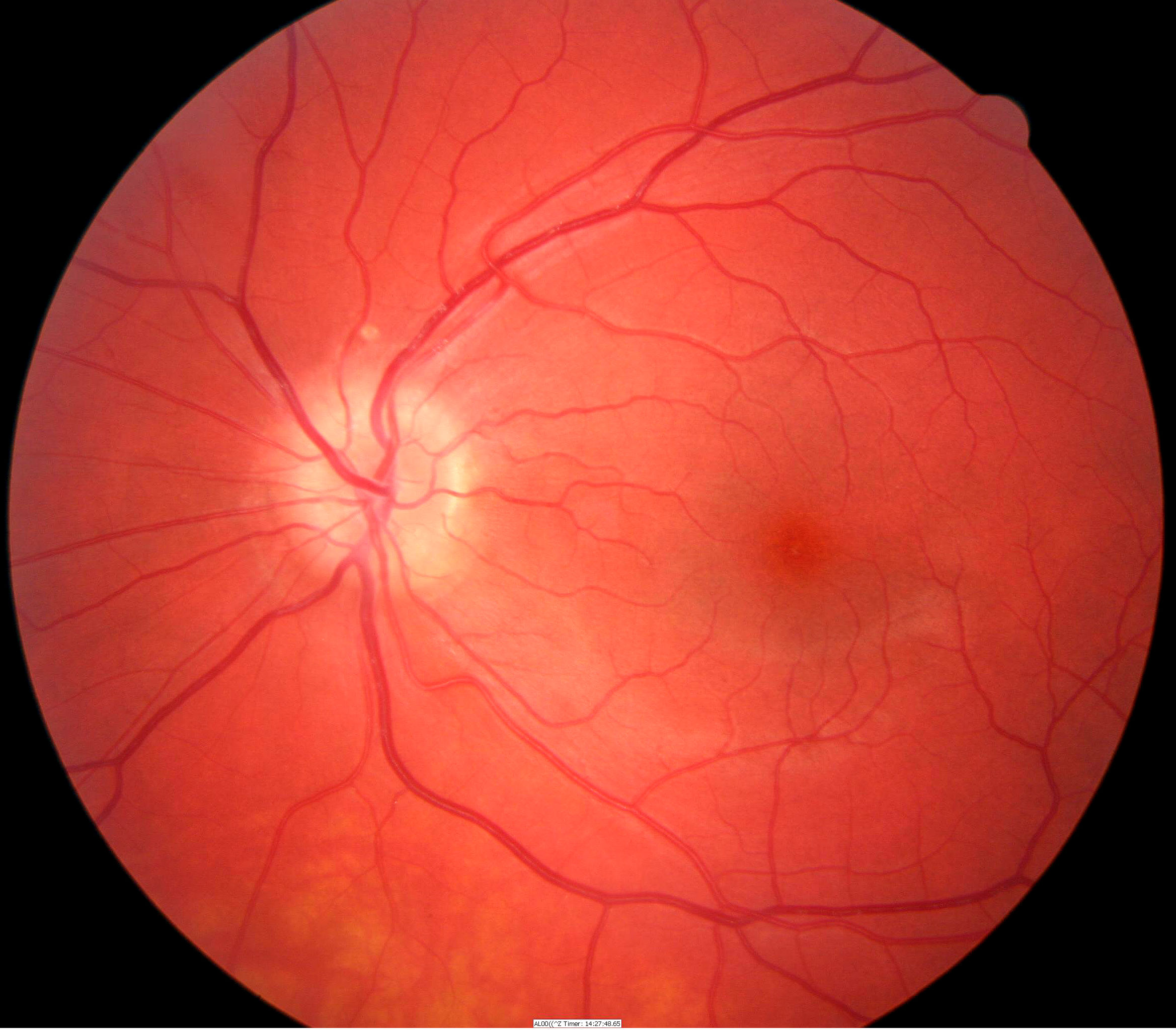
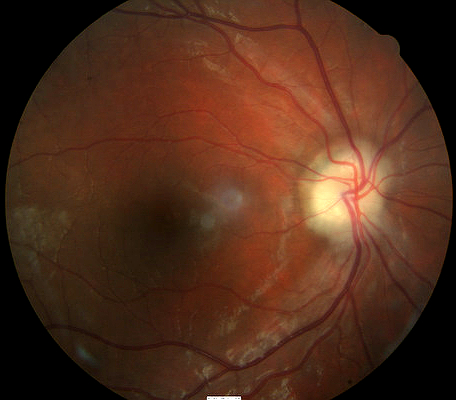
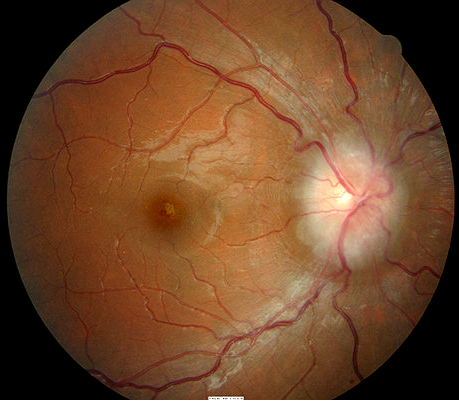
Clinical Appearance of the Retina
- 35-year-old white male
- Bilateral optic nerve drusen — Waxy pearl-like irregularities on the surface of the optic disc, drusen transilluminate as golden globes with slit-lamp beam
 |
 |
|
 |
 |
DIAGNOSTIC TESTS
B-Scan Ophthalmic Ultrasound
A readily available and reliable method for the definitive diagnosis of optic nerve drusen, especially when they are buried. Because optic nerve drusen are generally not calcified in children and adolescents, ultrasonography may prove to be of little assistance in diagnosing these cases.
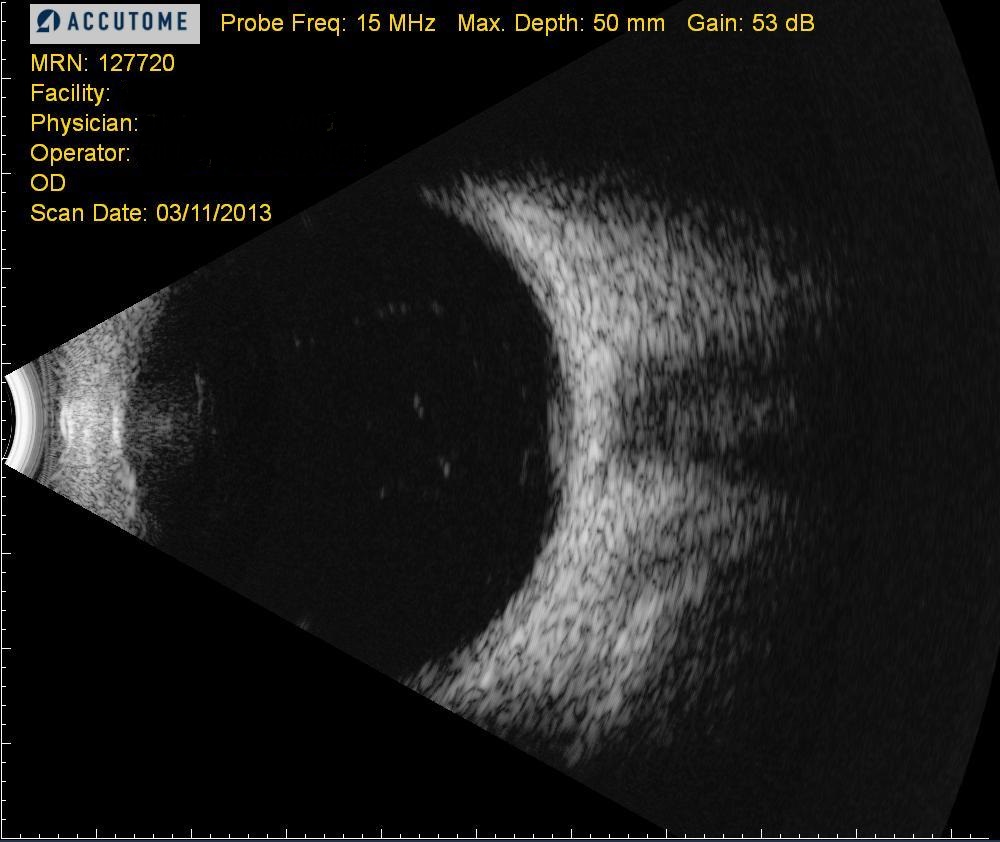 |
Optic Nerve Drusen
|
There are two types of optic disc drusen:
- Buried drusen
- Exposed drusen
In early childhood, buried optic disc drusen may be difficult to detect because they are deep beneath the surface of the disc. The appearance may mimic papilledema, presenting as a swollen disc. The drusen become slowly visible as they enlarge toward the disc surface and as the overlying retinal nerve fiber layer progressively thins.
Buried Optic Disc Drusen
Buried optic disc drusen are characterized by the following clinical signs:
- Presents as an elevated disc with a scalloped margin
- No physiological optic cup
- Hyperemia is absent and the surface vessels are not obscurred, despite disc elevation
Anomalous vascular patterns are also present.
- Early branching
- Increased number of major retinal vessels
- Tortuosity
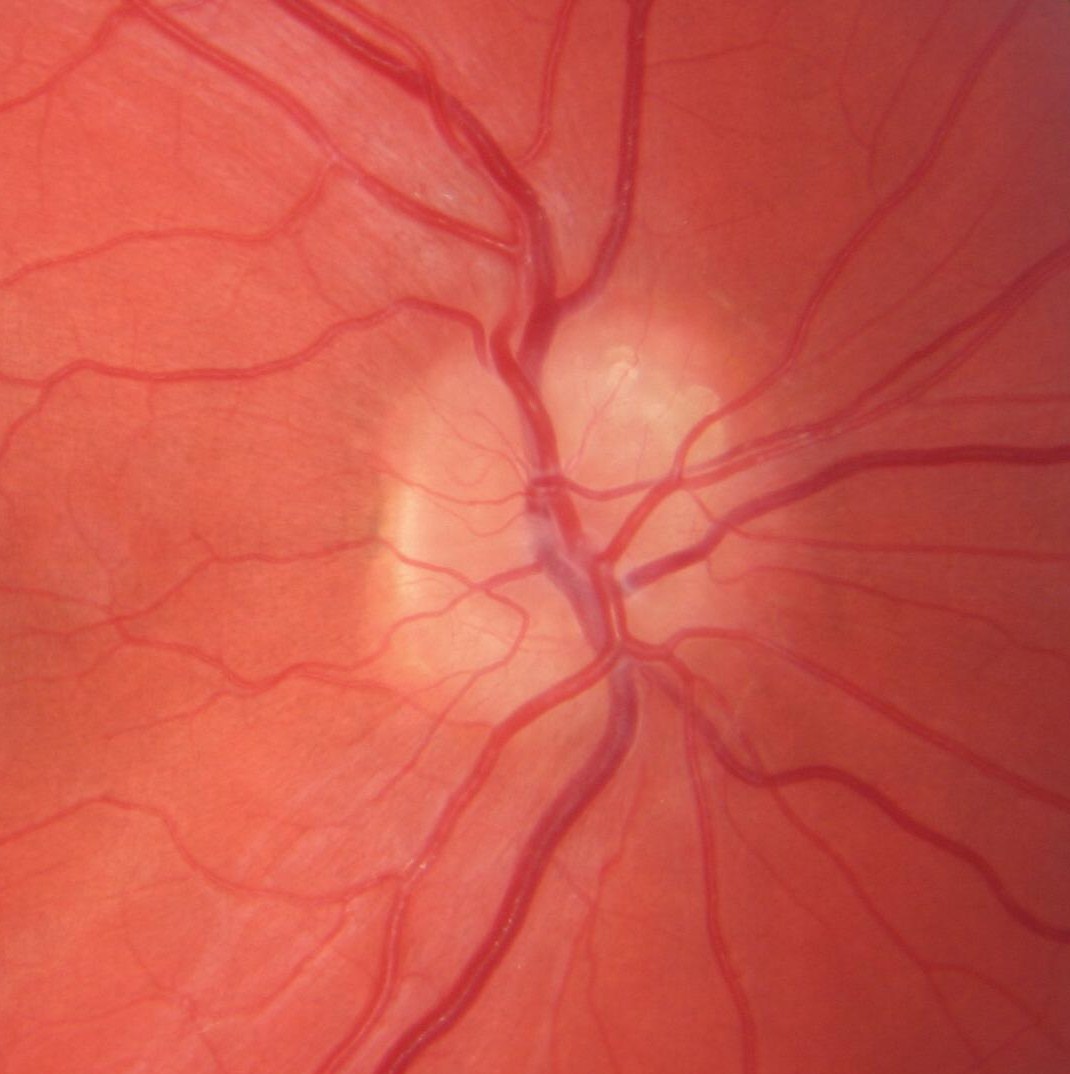
Exposed Optic Disc Drusen
In the early teenage years, optic nerve drusen typically emerge at the surface of the disc as waxy pearl-like irregularities. At this point, they are classified as exposed.
 |
Exposed Optic Disc Drusen
|
Recognize the clinical features associated with optic nerve drusen in comparison to those features indicative of true optic disc edema.
- In optic nerve drusen, expect a typically “normal” pink to pinkish-yellow color, rather than a pale waxy disc or a hyperemic disc
- A spontaneous venous pulsation is present in about 80% of patients with optic nerve drusen, but is absent in cases of true disc edema
- Most importantly, recognize that while the disc margins may be irregular in optic nerve drusen, rarely are they blurred or obscured.
The following diseases share some of the clinical signs of optic disc drusen:
- Optic papillitis
- Papilledema
- Optic nerve pit
- Glaucoma
- Toxic optic neuropathy
- Compressive optic neuropathy
- Anterior ischemic optic neuropathy
 |
Optic Papillitis
|
|
 |
Papilledema
|
|
 |
Optic Nerve Pit
|
The primary goal of treating a patient with optic nerve drusen is to make the correct diagnosis. If there are no macular complications, the best treatment option is observation with an annual surveillance examination.
Palliative Treatment
- Patient education regarding periodic self-monitoring of vision because of the risk of choroidal neovascular membrane formation
- An annual surveillance examination for optic nerve drusen may include the following service components:
- refraction
- dilated fundus examination
- visual field examination
- fundus photgraphy
- OCT imaging of the maculas
- pupillary examination
- electrodiagnostic testing
- visual evoked potentials
- electroretinogram
Preventive Treatment
Patients with optic nerve drusen are more susceptible to visual field compromise when intraocular pressure is artificially elevated during procedures such as cataract surgery and LASIK surgery. Likewise, a patient with optic nerve drusen is more susceptible to damage during an attack of ischemic optic neuropathy. Precautionary measures such as IOP lowering and neuroprotection should be considered in these patients.
Surgical Treatment
If choroidal neovascular membranes are noted or suspected, intravenous fluorescein angiography is recommemded, followed by laser photocoagulation as indicated.
1. Goodwin D. The Differential Diagnosis of an Optic Nerve Disorder. April 2010. http://www.reviewofoptometry.com/continuing_education/tabviewtest/lessonid/106713/. Last accessed January 22, 2015.
2. Kreda S. Diagnosis and Management of Optic Disc Elevation. Optometric Management. 1 June 2009. http://www.optometricmanagement.com/articleviewer.aspx?articleID=103086. Last accessed August 13, 2014.
377.21
Drusen of optic disc
92250
Fundus photography
92133
OCT scan of optic nerve
92083
Visual field examination
95930
Visual evoked potential
92275
Electroretinography
92283
Color vision examination
92225
Extended ophthalmoscopy
76512
B-scan ophthalmic ultrasound
Occurrence
The prevalence of optic nerve drusen is approximately 0.3 – 1% of the general population.
Distribution
Optic nerve drusen is not distributed evenly throughout the population.
- Caucasians are primarily affected
- Believed to demonstrate an autosomal irregular pattern of inheritance with incomplete penetrance




 Print | Share
Print | Share