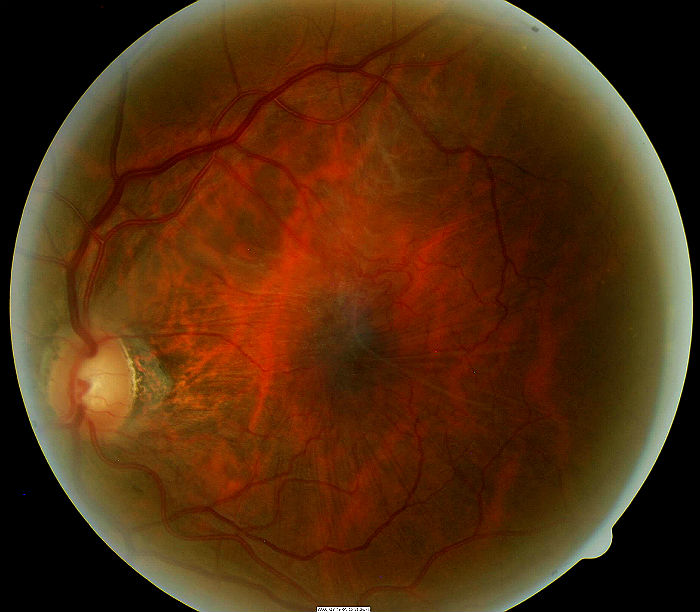
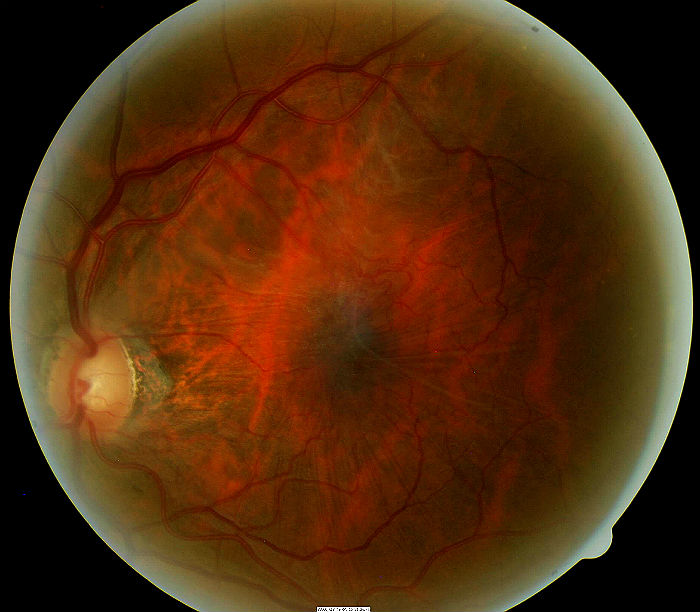
Epiretinal membrane encompassing the macula
ICD-10 Diagnosis Codes:
H43.311–Vitreous membranes and strands, right eye
H43.312–Vitreous membranes and strands, left eye
H43.313–Vitreous membranes and strands, bilateral
Title
Vitreous Membranes and Strands
Category
Disorders Of The Vitreous
Description
Vitreous membranes are collections of glial cells, collagen cells and inflammatory cells that form on the inner surface of the retina.
Vitreous membrane is the clinico-anatomic description of epimacular proliferation.
- Epimacular proliferation is characterized by the formation of collagenous membranes on the surface of the retina
- As the membranes grow, they can develop contractile properties that produce traction forces on the retinal surface
- Traction on the macula can result in traction maculopathies such as cellophane maculopathy, macular pucker, vitreomacular traction syndrome, or macular hole
 |
Common names for Epimacular Proliferation
|
The histopathological changes needed to create epiretinal membranes usually begins with trauma to the retina, the most common being a posterior vitreous detachment. In some people, it’s believed that the separation of the vitreous membrane from the retinal surface damages the retina structurally.
Structural Damage to the Eye
- Posterior vitreous detachment produces focal areas of damage on the inner retinal surface
- Immune system response to damaged areas results in inflammatory reaction on the inner retinal surface
- Glial cells from the neurosensory retina grow through breaks in the internal limiting membrane of the damaged retina
- Glial cells combine with inflammatory cells and collagen cells to form membranes
- Membranes form attachments to the inner retinal surface
- Membranes proliferate in the central retina and macula
- Membranes may contract over time and create traction forces on retinal tissue
- Underlying retina may become structurally damaged secondary to traction forces
Functional Damage to the Eye
- Traction on the macula produces decreased visual acuity based on the amount of disruption to the normal retina micro-structure
- Vascular imcompetence secondary to macular traction (especilally in diabetic patients) results in progressive loss of acuity
- Diffuse macular edema usually results in decreased vision
- Foveal cysts usually results in decreased vision
- Macular detachment results in decreased vision
The main goal of the diagnostic evaluation in a patient with epiretinal membrane is to accomplish the following:
- Evaluate epiretinal membrane density, thickness, and location in relation to the retina
- Determine the presence or absence of macular surface traction secondary to the epiretinal membrane
- Determine the presence or absence of vascular incompetence secondary to surface traction
- Determine the presence or absence of macular edema secondary to surface traction
- Prescribe a treatment program to manage any traction maculopathy and prevent permanent vision loss
Patient History
The symptoms of epiretinal membrane vary from no symptoms to severe visual impairment. Patients with early disease may report blurred vision, decreased vision, or mild visual distortion. More advanced presentations often produce metamorphopsia, micropsia, or other abnormal visual distortions of shape and size. Significant presentations can present with frank reduction is visual acuity.
Patients with epiretinal membrane usually present with the following range of decreased visual acuity:
- 20/25 acuity or better is present in 56-67% of patients
- 20/40 acuity or better is present in 75-85% of patients
- 20/400 acuity or worse is present in 2-5% of patients
Ophthalmoscopy
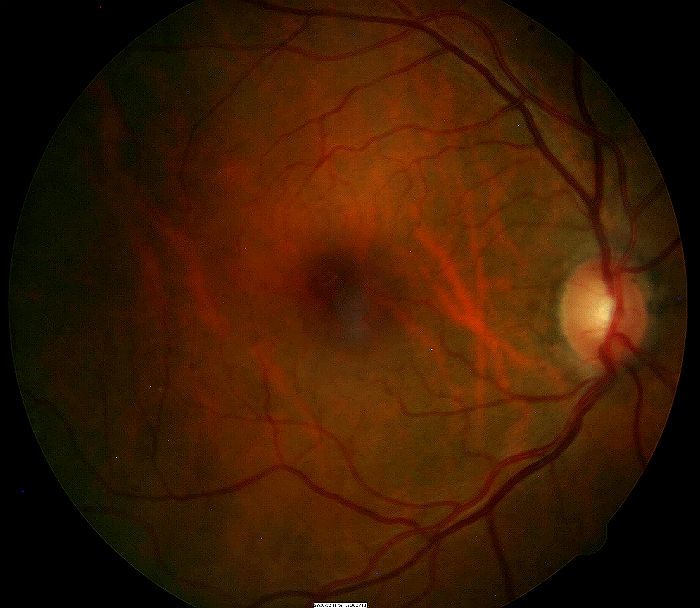
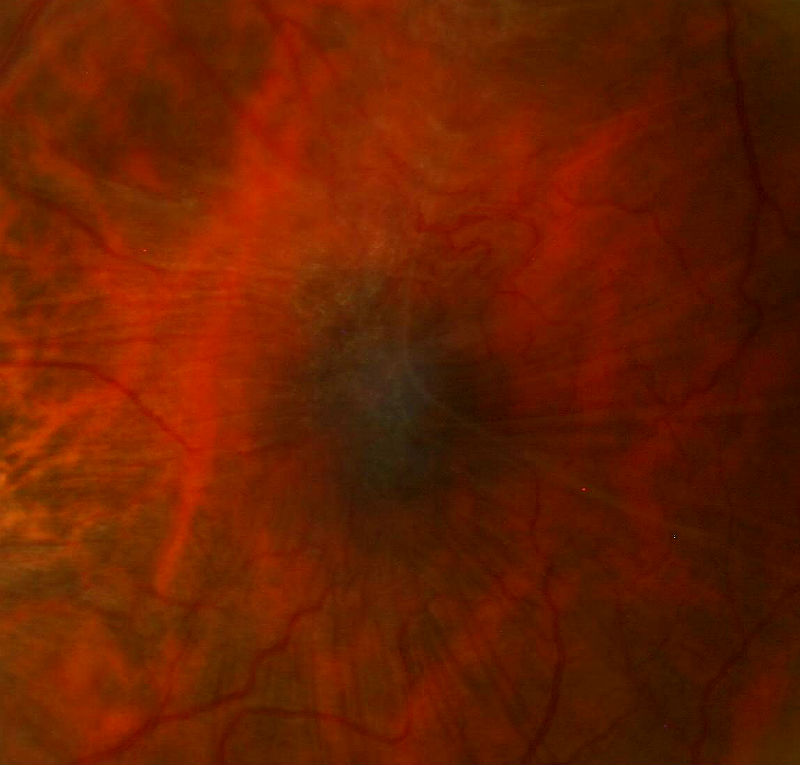
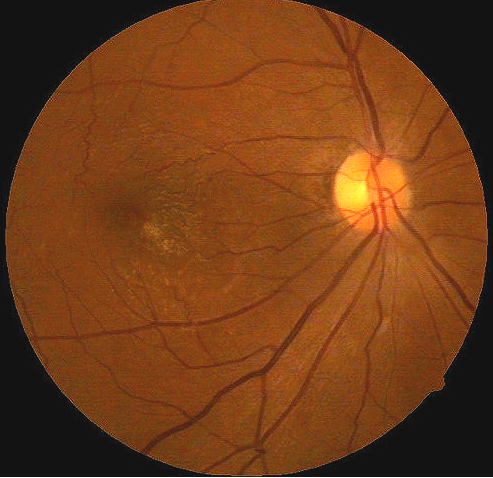
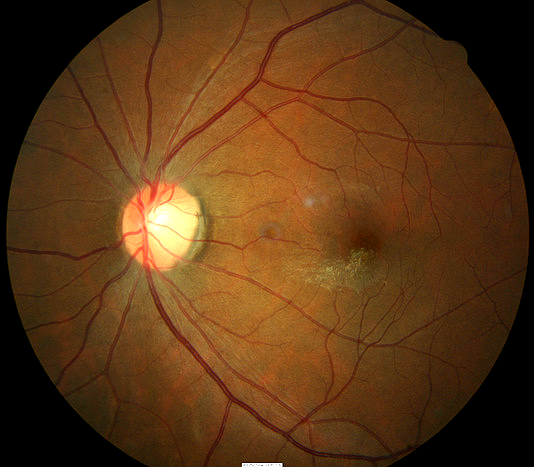
- A small epiretinal membrane adheres to the retinal surface over the left macula
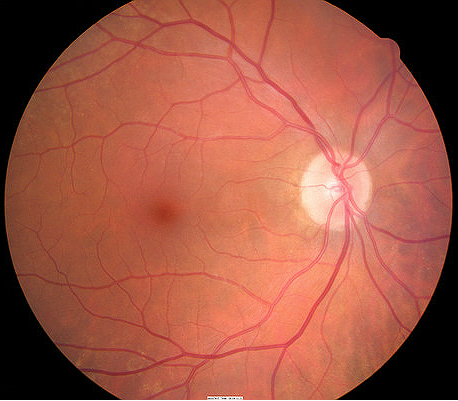
- The right eye’s retinal surface is normal
 |
 |
|
 |
 |
DIAGNOSTIC TESTS
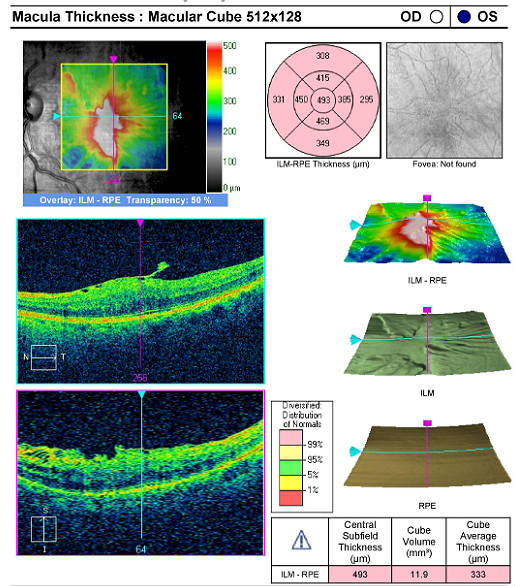
Retinal Laser Scan
- OCT testing can determine the presence or absence of an epiretinal membrane
- OCT testing can objectively measure the effects of the epiretinal membrane on the macular structure
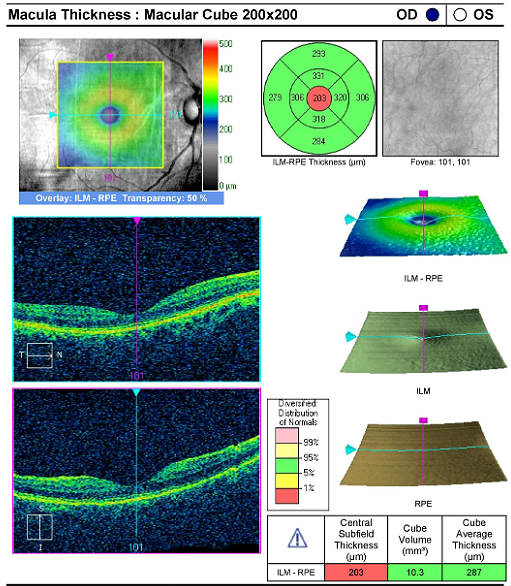 |
Right Eye — Normal Macular Structure
|
|
Left Eye — Epiretinal Membrane
|
 |
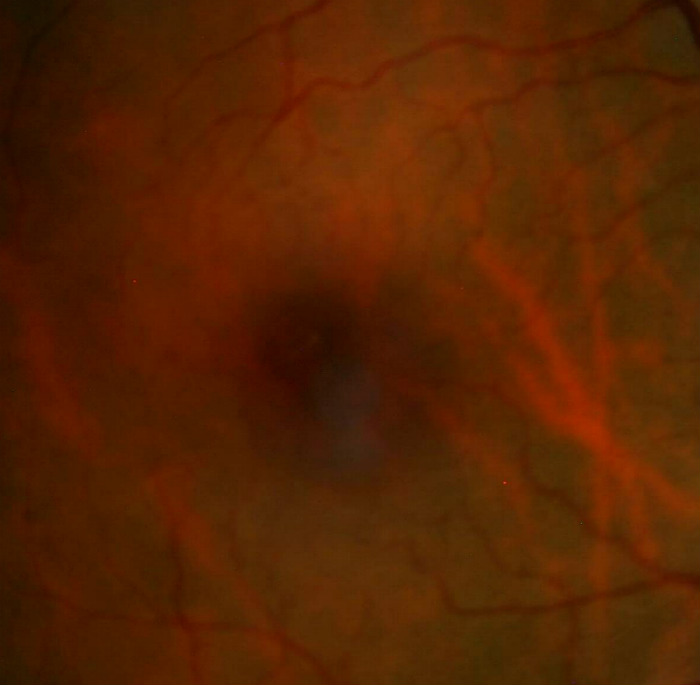
Classification of epiretinal membranes is based on the apperance of the membrane and the underlying retina and blood vessels.
 |
Grade 0 membranes
|
|
Grade 1 membranes
|
 |
|
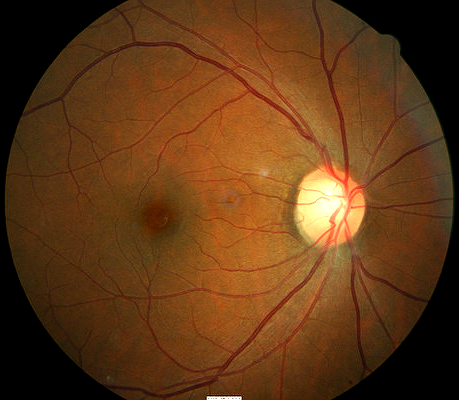
Right eye with normal appearance |
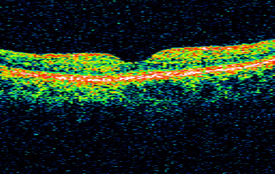
Normal OCT scan of right macula |
|
Optical Coherence Tomography
|
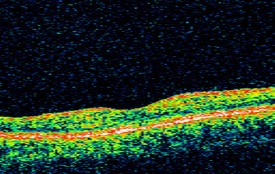
OCT scan of left macula |
|
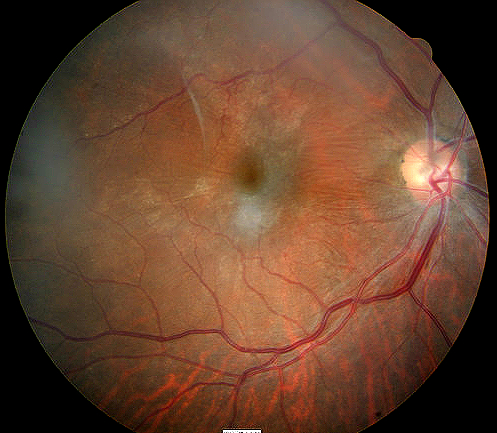
Right eye with epiretinal membrane |
Grade 2 membranes
|
|
Bilateral Presentation of Epiretinal Membrane
|
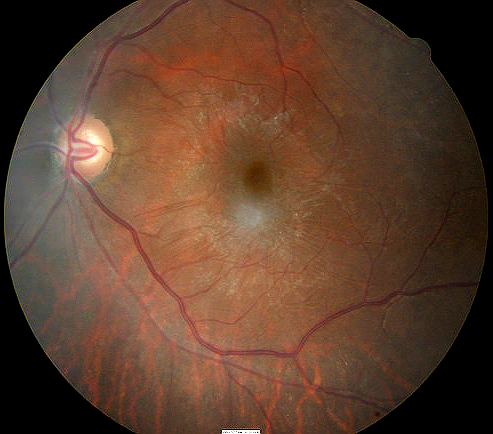
Left eye with epireinal membrane surrounding the macula |
Multiple events may mimick the presentation of epiretinal membranes but all lack the one factor that sets them apart – the presence of the actual membrane.
Retinal vascular occlusive disease
Retinal occlusvie disease can present with disruption of retinal structure secondary to fluid accumulation or ischemia. Retinal blood is uncommon with epiretinal membranes and ischemia is never a factor. Most notably, there is no epiretinal membrane.
Diabetic macular changes
More advanced retinopathy can produce all the signs seen in a macular changes associated with an epiretinal membrane, including preretinal fibroelastic tissue, retinal and vitreous hemorrhages and disruption (elevation) in the macula structure. The fibroelastic changes with diabetes are less common and the patient history is typically different (trauma vs systemic disease).
Cystoid macular edema (CME)
CME can produce elevation of macular structure through edema but is associated with cataract surgery and has no associated epiretinal membrane.
Observation
Most cases of vitreous membranes do not require treatment. The condition should be monitored by direct observation and scanning laser for changes in the macula that could increase the risk of more significant functional vision loss. In most cases, retinal surgeons will not consider surgical intervention until best corrected acuity is worse than 20/50-20/70. With the new option of Plasmogin vitreolysis, more aggressive treatment may be considered over time.
 |
 |
1. Vitreomacular traction syndrome. National Retina Institute. http://nationalretina.com/RetinalConditions/VitreomacularTractionSyndrome.aspx. Last accessed April 3, 2014.
2. Morris R, Witherspoon CD, Kuhn F, Nelson S, Priester B, Mayne R. Traction maculopathy. Retinology Today.
3. Vitreomacular traction. Williamson Eye Institute. http://www.williamsoneyeinstitute.com/retina-center/vitreomacular-traction. Last accessed April 3, 2014.
379.25
Vitreous membranes and strands
92225
Extended ophthalmoscopy
92015
Refraction
92250
Fundus photography
92134
Macula OCT scan




 Print | Share
Print | Share