ICD-10 Diagnosis Codes:
H46.11–Retrobulbar neuritis, right eye
H46.12–Retrobulbar neuritis, left eye
H46.13–Retrobulbar neuritis, bilateral
Title
Retrobulbar Neuritis (Acute)
Category
Disorders Of The Optic Nerve And The Visual Pathways
Description
Optic neuritis is an inflammation of the optic nerve. It is a variable condition and can present with any of the following symptoms: acute loss of vision, changes in color vision, pain behind the eye and complete or partial blindness.
Optic neuritis usually occurs secondary to a demyelination event along the optic nerve or the neural pathways in the brain. It is commonly associated with the following conditions.
- Autoimmune disorder (multiple sclerosis, sarcoidosis, Lupus)
- Infections (syphilis, mumps, measles)
- Diabetes
- Granulomatous diseases
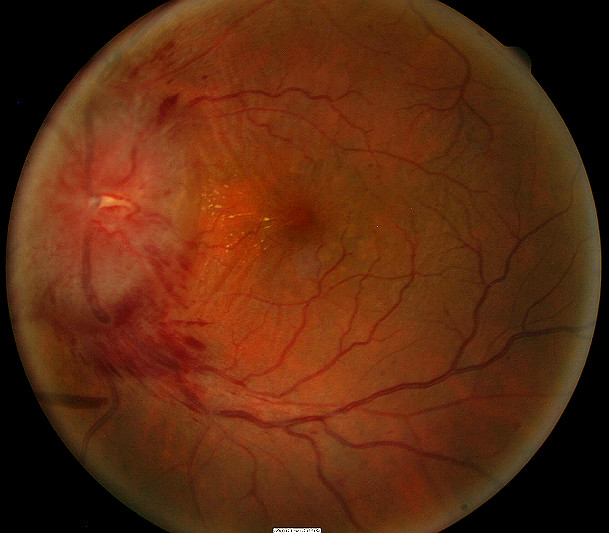
Some of the clinical signs of optic neuritis associated with multiple sclerosis include sudden onset of unilateral vision loss associated with retro-orbital pain that is aggravated by eye movement. Decreased vision following exercise, hot shower or bath or activities that elevate body temperature can also occur. Common symptoms patients report are tender or sore eyes. There can be a loss of color vision and contrast sensitivity. In addition, there may be a relative afferent pupillary defect present and optic disc hyperemia or swelling.
Since multiple sclerosis is the cause of demyelinating optic neuritits, it will be the focus of this disease glossary.
Structural Damage to the Eye
- Inflammation of the optic nerve
- Demyelination of the optic nerve
Functional Damage to the Eye
- Associated visual field defects
- Blurred vision
- Reduced color vision
- Reduced contrast sensitivity
- Abnormal VEP waveform
The main goal of the diagnostic evaluation in a patient with optic neuritis is to accomplish the following:
- Determine the etiology of the optic neuritis
- Identify and exclude any differential diagnosis
- Determine the monitoring schedule and prescribe a treatment program specific to the etiology
Patient History
Patients with optic neuritis may present with any of the following abnormal signs and sypmtoms:
- Sudden onset of unilateral vision loss
- Pain with eye movements
- Relative afferent pupillary defect
DIAGNOSTIC TESTS
The following diagnostic tests are used to determine the extent of structural and functional damage from the optic neuritis:
Refraction
- Measurement of visual function / visual acuity helps determine improvement of vision as the inflammation resolves
Visual Field Examination
- A visual field defect can be noted around the blind spot and the extent of edema corresponds to the visual field defect
- There may be an overall reduction in retinal sensitivity seen as well
Color Vision Examination
- Patients can also have a decrease in color perception especially red hues appear dimmer
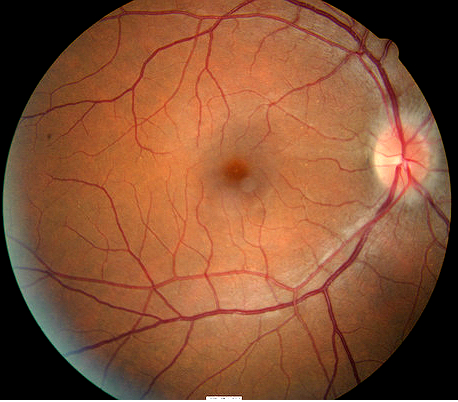
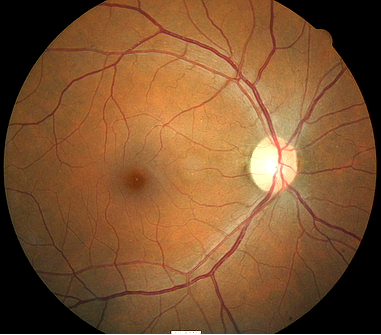
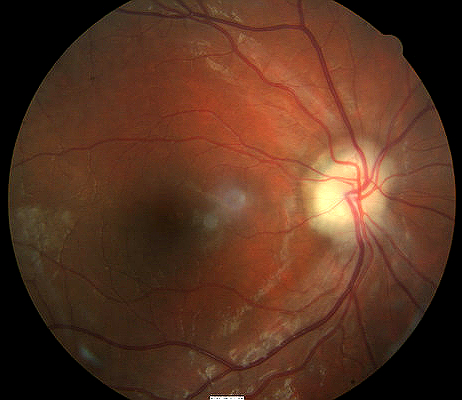
Extended Ophthalmoscopy
- Helps evaluate optic disc morphology and look for elevation of optic nerve
- Assist with documenting abnormal structural changes to the optic disc
Fundus Photography
- Another means to evaluate optic disc morphology and elevation of optic nerve
- It can also assist in document abnormal structural changes to the optic disc
Retinal Scanning Laser
- Provides detail of the excavation of the optic disc
There are four subtypes of optic neuritis:
- Retrobulbar optic neuritis
- Optic papillitis
- Perineuritis
- Neuroretinitis
Perineuritis
This type of optic neuritis is characterized by an inflammation of the optic nerve sheath. In this condition, the optic nerve is spared and vision loss is mild to moderate. Perineuritis usually affects older people and is commonly associate due to infectious or inflammatory conditions (e.g., sarcoidosis). Perineuritis is not associated with multiple sclerosis.
Neuroretinitis
This type of optic neuritis may occur at any age. It is characterized by concomitant swelling of optic disc and macula. In severe presentation, exudates form around the macula to give the appearance of a macular star. Neuroretinitis is not associated with multiple sclerosis.
Orbital infection
- Orbital infections can cause inflammation and edema to occur at the optic nerve.
Sinusitis
- Can mimic pain with ocular eye movements.
Tuberculosis
- Patients on tuberculosis treatment can sometimes develop inflammation of the optic nerve.
Ischemic optic neuropathy
- Ischemia can cause the optic nerve to look inflamed and edematous.
Acute angle-closure glaucoma
- Acute rise in intraocular pressure can produce ocular pain and loss of vision similar to that seen in retrobulbar optic neuritis
Compressive optic neuropathy
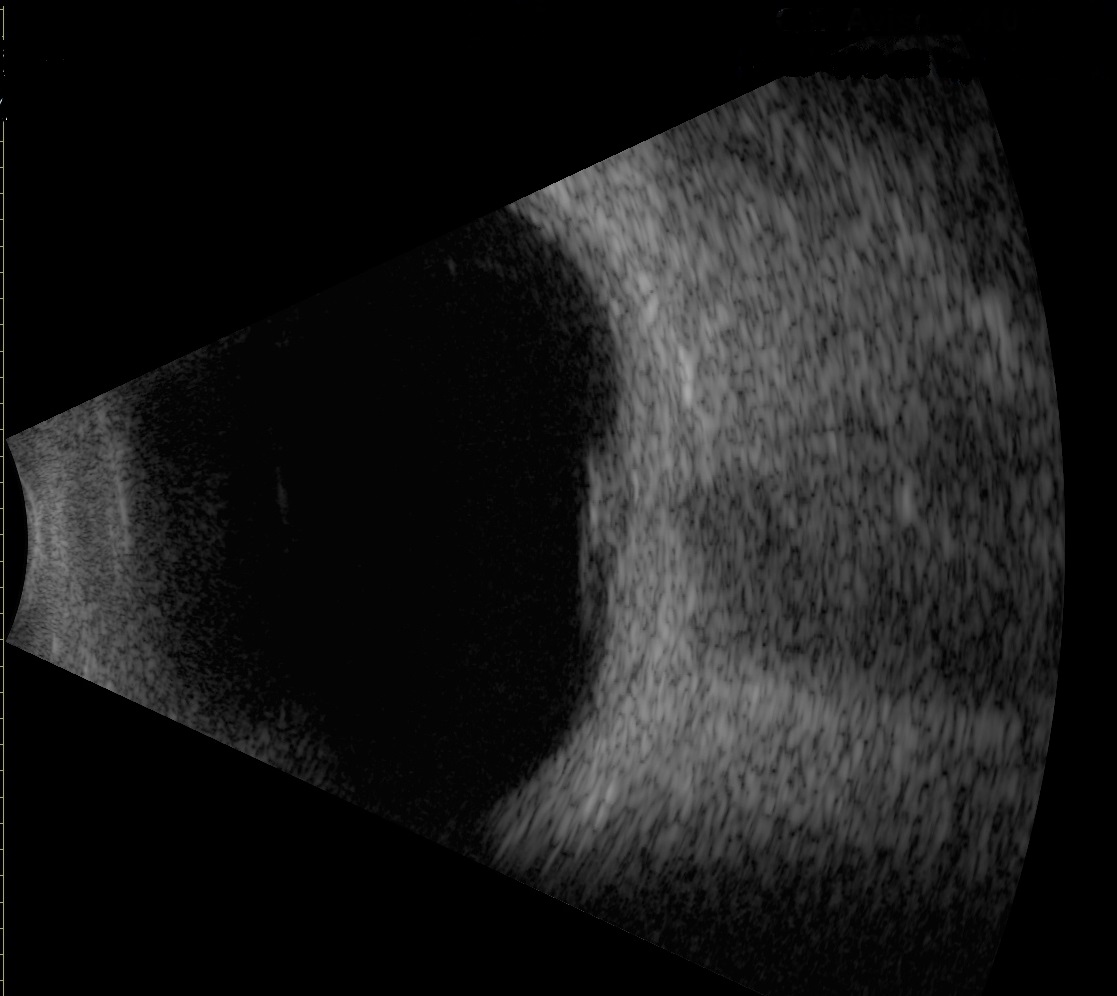
- Compression of the optic nerve can cause the optic nerve to become edematous
- Elevation of the optic nerve head imaged on B-scan ultrasound
 |
 |
Palliative Treatment
- Monitor the patient and allow the optic neuritis to resolve on it’s own
- Vision generally improves over 2-3 weeks if left untreated
Pharmacologic Therapy
- Since 20-25% of patients with an initial diagnosis of optic neuritis develop multiple sclerosis, treatment should be considered if a patient has had symptoms of optic neuritis in the past that are undiagnosed or patient has other neurological symptoms associated with ocular manifestations or patient has a family history of multiple sclerosis.
- The Optic Neuritis Treatment Trial (ONTT) supports the administration of intravenous methylprednisolone sodium succinate (Solumedrol, 250 mg. every 6 hours) for three days. Then followed by oral prednisone (1 mg/kg per day) for 11 days accelerates vision recovery, but does not affect the extent of vision that is recovered. So the combination therapy does not improve visual outcome to optimal vision before the vision loss, but it does increase the rate the vision recovers.
- The study also showed the use of oral prednisone (1 mg/kg per day) alone for 14 days is contraindicated. Patients receiving this therapy have a higher chance of new attacks of ON in both the initially affected and fellow eyes in comparison to the combination therapy or the placebo group.
If the combination of intravenous and oral steroids does not work and vision loss persists, then plasma exchange therapy may help recover vision.
1. Ergene E. Adult Optic Neuritis. Medscape/EMedicine. 19 Mar 2014. http://emedicine.medscape.com/article/1217083-overview. Last accessed August 13, 2014.
2. Menon V. Saxena R. Misra R. Phuljhele S. Management of Optic Neuritis. National Library of Medicine. 10 Nov 2010. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3116540/. Last accessed August 13, 2014
377.32
Retrobulbar neuritis (acute)
92015
Refraction
92083
Visual field examination
92250
Fundus photography
92133
Retinal laser scan
95930
Visual evoked potential
92283
Color vision examination
Optic neuritis secondary to multiple sclerosis
Occurence
The prevalence of optic neuritits is closely tied to the prevalence of mulitple sclerosis which is 0.1% of the population.
Distribution
Optic neuritis is not distributed evenly throughout the population.
- Females are affected more
- Caucasians are 8 times more likely to develop optic neuritis than African Americans and Asians
- Age of onset from 20-40 years old
Risk Factors
- Age
- Sex
- Autoimmune diesease
- Infections
- Diabetes
- Tuberculosis




 Print | Share
Print | Share