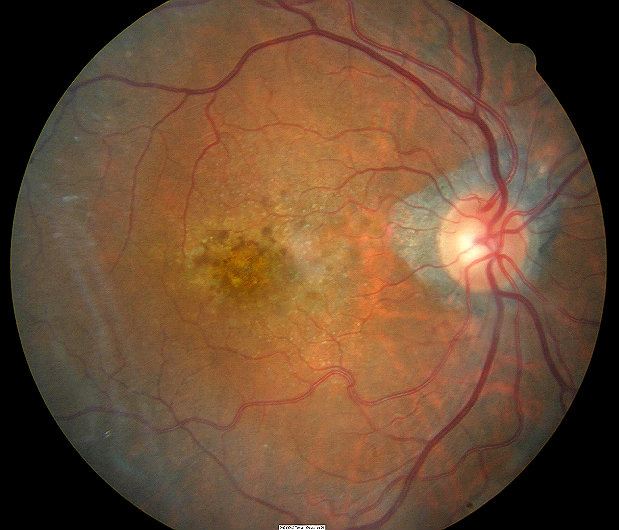
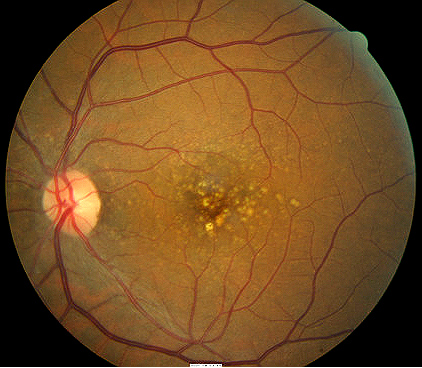
Dry age-related macular degeneration in a 91-year-old
ICD-10 Diagnosis Code:
H35.31–Nonexudative age-related macular degeneration
Title
Nonexudative Senile Macular Degeneration of Retina
Category
Other Retinal Disorders
Description
Nonexudative senile macular degeneration or dry macular degeneration is a condition that affects the macula region of the retina resulting in central vision loss.
Age-related macular degeneration describes any type of acquired maculopathy that affects people over 50-years old. These macular diseases are collectively known as age-related macular degeneration (AMD) are are separated into two main forms:
Dry Macular Degeneration: The atrophic form of the disease is characterized by a gradual breakdown of cells in the macula, resulting in a gradual blurring of central vision. Single or multiple, small, round, yellow-white spots called drusen are the key identifiers for the dry type. Patients may still have excellent vision and no symptoms. Most people with age-related macular degeneration begin with the dry form.
The dry form of macular degeneration is much more common than the wet form. Advanced dry macular degeneration is known as geographic atrophy, and its development is the culmination of prolonged, progressive changes in the nerves and sensory retina. Geographic atrophy is the main cause of vision loss in dry AMD, not drusen.
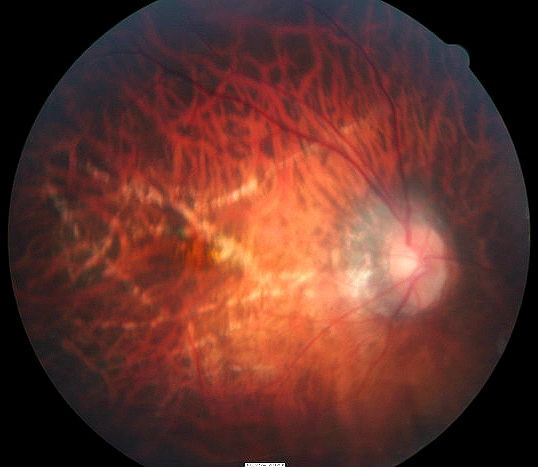
Wet Macular Degeneration: The exudative form of the disease is characterized by neovascularization under the macula. These abnormal blood vessels leak, bleed, and scar the retina, distorting or destroying central vision. Visual distortion tends to be unilateral and may progress to affect the other eye later. Vision loss may be rapid in the wet type of macular degeneration in comparison to the dry form.
Structural Damage to the Eye
- Drusen causes structural changes to the retina in the dry form
- Progressive atrophy of the nerves and sensory retina over time in the dry form
Functional Damage to the Eye
- Sudden or gradual blurred or distorted central vision
- Patient reports difficulty seeing faces or doing normal tasks like reading
- Sudden or gradual decreased visual acuity
- Patient reports straight lines appear crooked, wavy or distortedects appear smaller in one eye than the other
The main goal of the diagnostic evaluation in a patient with macular degeneration is to accomplish the following:
- Evaluate the extent of structural changes such as exudates, edema or atrophy in the macula
- Determine the presence or absence of vascular abnormalities secondary to the macular degeneration
- Determine the presence or absence of atrophy secondary to the macular degeneration
- Determine whether the macular degeneration is in the dry or wet form
- Prescribe a treatment program to manage the macular degeneration and slow the vision loss
Patient History
Patients present with symptoms of unilateral central vision loss which is usually gradual, but can be sudden if it is the wet form of macular degeneration. Most of the time, patients describe the vision loss as distortions of faces, lines or metamorphopsia.
| Ophthalmoscopic Examination
Ophthalmoscopy will reveal the following clinical signs:
|
 |
DIAGNOSTIC TESTS
The clinical application of the following test can be utilized in the documentation, monitoring and treatment of any pathological condition that affects the internal structures of the eye.
Refraction
- Allows for the measurement of visual function
Fundus Photography
- To document the progress or lack of progress of macular degeneration
- To document the delivery of medical treatment
- To document the response to treatment
- To help plan a treatment program
- Fundus autofluorescence imaging can be used to detect structural abnormalities and predict functional deficits before the defects appear on standard color fundus photography
- Multi-spectral imaging with the Annidis RHA System can be used to detect structural abnormalities and predict functional deficits before the defects appear on standard color fundus photography
 |
 |
Extended Ophthalmoscopy
- Patients with miotic pupils and dense cataracts may not allow a good view of the internal structures with fundus photography (extended ophthalmoscopy may be an alternative to view internal structures)
- Document any other associated structural changes to the macula
- Help plan a monitoring and treatment program for the macular degeneration
Retinal Scanning Laser – Macula
- Document the location and extent of the macular degeneration at a structural level
- Document any other associated structural changes to the macula
- Help plan a monitoring and treatment program for the macular degeneration
Visual Field Examination
- Used to determine the extent of functional damage to vision in comparison to structural damage
The information provided by these tests are used for medical decision-making in the following manner:
- To document the progress of the macular degeneration
- To document the delivery of the medical treatment
- To document the response to treatment
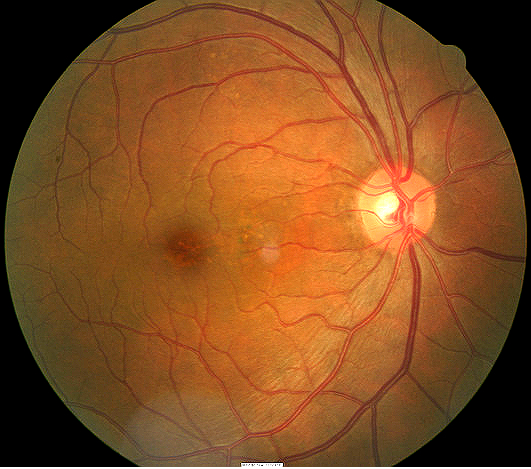
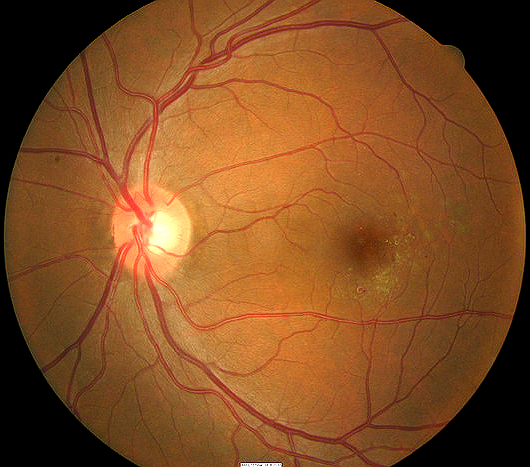
Dry age-related macular degeneration has three stages: early, intermediate and advanced.
 |
Early Age-Related Macular Degeneration
|
|
Intermediate Dry Age-Related Macular Degeneration
|
 |
|
 |
Advanced Dry Age-Related Macular Degeneration
|
Conditions that affect the retinal pigment epithelium and chorio-capillaries
- Herditary diseases (Stargardt’s disease, Best’s disease)
- Angiod streaks
- Bilataral idiopathic juxtafoveal telangiectasis
- Toxic lesion (plaquenil, chloroquine, phenothiazines, canthaxanthin)
Conditions that cause choroidal neovascularization
- Herditary diseases (Best’s disease, Angiod Streaks)
- Ocular histoplasmosis
- Toxoplasmosis retinochoroiditis
- Traumatic choroidal rupture
- Sarcoidosis
- Multifocal choroiditis
Other causes of subretinal hemorrhages
- Macroanerysms along the retinal arterioles
- Choroidal rupture
Other causes of subretinal fluid
- Central serous retinopathy
Environmental Changes
- Maintain healthy lifestyle (eat diet high in leafy vegetables and fish, do not smoke, maintain normal blood pressure, maintain weight, and exercise)
Phamacologic Treatment
For those who have the dry AMD and are at high risk for developing either advanced dry or wet AMD should consider taking vitamin supplements. Specific daily amounts of antioxidants and zinc may help slow the progression of AMD into the advance stages. The formula used in the AREDS study was 500 milligrams of vitamin C, 400 International Units of vitamin E, 15 milligrams of beta-carotene (label as 25,000 International Units of vitamin A), 80 milligrams of zinc as zinc oxide, and two milligrams of copper as cupric oxide. The AREDS formulation is specific and different from a regular daily multivitamin. Ocuvite PreserVision (Bausch & Lomb), ICaps (Alcon), and Macular Protect Complete (Science Based Health) are products that contain the AREDS formulation.
1. Maturi R. Nonexudative ARMD. Medscape/EMedicine. http://emedicine.medscape.com/article/1223154-overview. Last accessed August 17, 2014.
2. Richer S. Assessing Dry Macular Degeneration. Optometric Management. 1 Jan 2009. http://www.optometricmanagement.com/articleviewer.aspx?articleid=102509. Last accessed August 17, 2014.
362.51
Nonexudative Senile
Macular Degeneration
92250
Fundus photography
92225
Extended ophthalmoscopy
92134
Macula OCT scan
92083
Visual field examination
92283
Color vision examination
92275
Electroretinography
Occurence
- The prevalence of age-related macular degeneration is almost 1.5% of the population over 40 years old
- The prevalence increases drastically with age
- For example, 15% of caucasian women over the age of 80 will have age-related macular degeneration.
Distribution
Age-related macular degeneration is not distributed evenly throughout the population.
- Women are at a greater risk than men
- Caucasians are more likely to have vision loss from AMD than African Americans
Risk Factors
- Age
- Family history
- Gender
- Smoking
- Obesity
- High degree of myopia
- Lifelong exposure to sunlight
- Lighter iris color and light skin pigmentation
- Medications for osteoporosis may cause predisposition




 Print | Share
Print | Share