
Retinal hemorrhages indicate
Stage 3 hypertensive retinopathy
ICD-10 Diagnosis Codes:
H35.031–Hypertensive retinopathy, right eye
H35.032–Hypertensive retinopathy, left eye
H35.033–Hypertensive retinopathy, bilateral
Title
Hypertensive Retinopathy
Category
Other Retinal Disorders
Description
Hypertensive retinopathy is damage to the retina from high blood pressure.
Hypertension produces many ophthalmic manifestations. Because of the structural differences between the retina, the choroid, and the optic nerve, the vascular response to systemic hypertension varies according to the anatomic region.
Retinal response to chronic hypertension:
- Arteriolosclerosis (generalized narrowing of the retinal blood vessels)
- Copper wiring and silver wiring of retinal arterioles secondary to arteriosclerosis
- Arteriovenous nicking secondary to arteriosclerosis
- Retinal hemorrhages
- Nerve fiber layer fallout
- Increased tortuosity of retinal blood vessels
- Remodeling of blood vessels due to capillary nonperfusion
Choroidal response to chronic hypertension:
- Areas of the retinal pigment epithelium (RPE) atrophy and form focal white lesions
- Choroidal ischemia
- Serous retinal detachment secondary to retinal pigment epithelial necrosis
Hypertensive retinopathy is a risk factor for systemic morbidity and mortality. The Atherosclerosis Risk in Communities (ARIC) study demonstrated that hypertensive retinopathy is strongly associated with elevated blood pressure, but variable in its association with elevated cholesterol and other risk factors for atherosclerosis.
Mild hypertensive retinopathy (focal arteriolar narrowing and arteriovenous nicking) are weakly associated with systemic vascular disease. More severe presentations (microaneurysms, hemorrhages and cotton-wool spots) have astrong association with subclinical cerebrovascular disease, stroke, congestive heart failure and cardiovascular mortality.
Structural Damage to the Eye
|
 |
Functional Damage to the Eye and Visual System
- No visual, physical or ocular symptoms
- Headaches
- Blurred vision
The main goal of the diagnostic evaluation in a patient with hypertensive retinopathy is to accomplish the following:
- Determine the presence or absence of hypertensive retinopathy
- Classify the hypertensive retinopathy
- Identify and exclude differential diagnosis
- Determine if the retinopathy is clinically significant and/or vision threatening
- Prescribe a treatment program
Patient History
The severity of the symptoms or signs is varied and depends on severity of the retinal/choroidal changes. Patients can present with the following abnormal symptoms:
- Blurred vision (sudden or gradual)
- Distorted vision (sudden or gradual)
- Difficulty driving at night
- Floaters or dark spots in their field of view
Clinical Appearance of the Retina
The retinal changes associated with hypertensive retinopathy include the following:
- Hemorrhages
- Microaneurysms
- Cotton-wool spots
- Edema
- Ischemia
- Venous beading
- Intraretinal microvascular abnormalities
- Retinal thickening
- Increased retinal vessel tortuosity
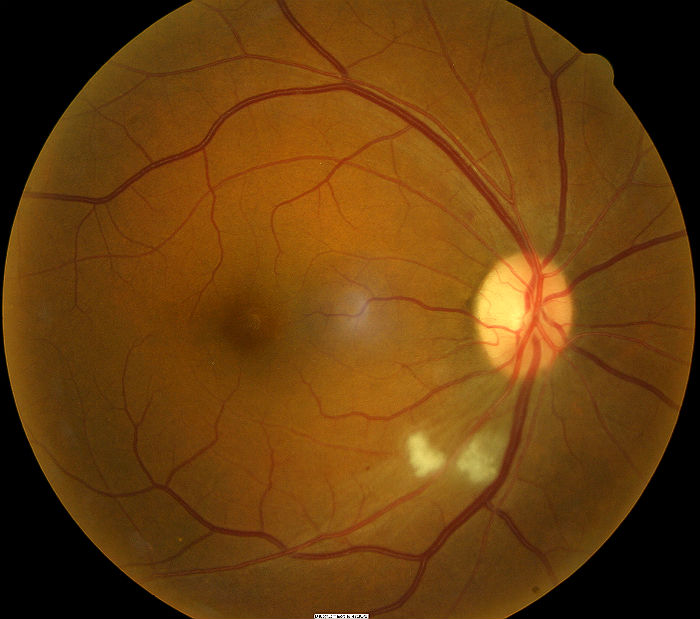 |
Grade 3 Hypertensive Retinopathy
|
DIAGNOSTIC TESTS
Fundus Photography
- To document the progress or lack of progress of hypertensive retinopathy
- To document the delivery of medical treatment
- To document the response to treatment
- To help plan a treatment program
- Fundus autofluorescence imaging can be used to detect structural abnormalities and predict functional deficits
 |
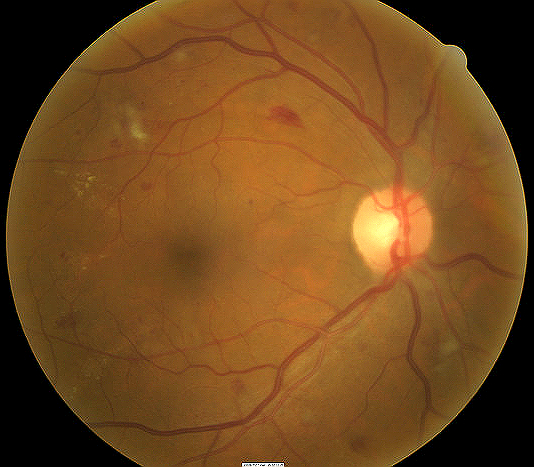
Retinal Hemorrhage Secondary to Hypertensive Retinopathy — Initial Visit
Optic Disc Hemorrhage May Be Associated With The Following:
|
|
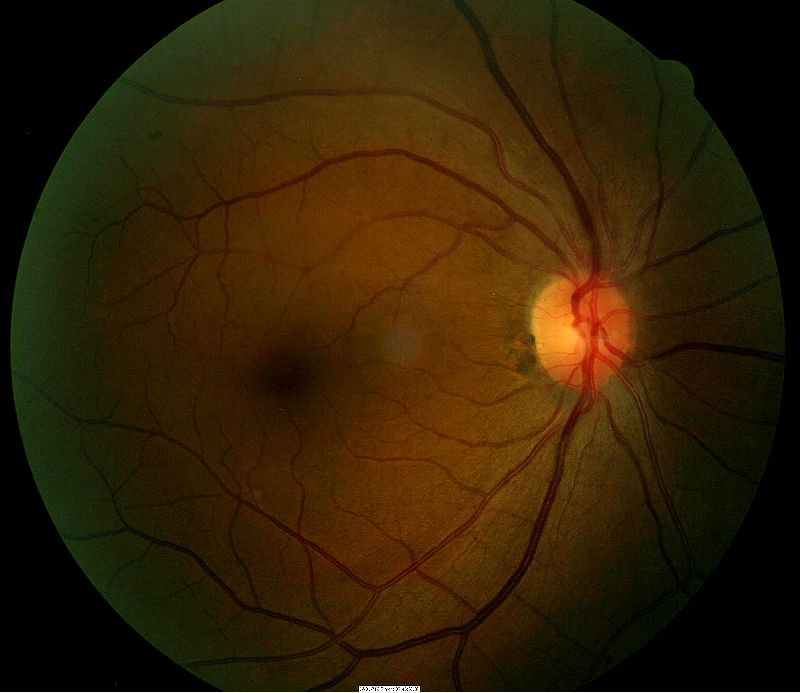 |
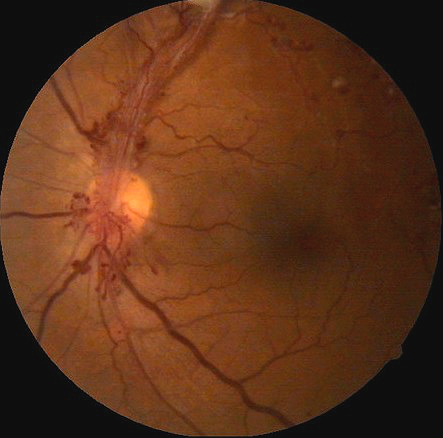
Same Patient As Above — 8 Days Later
Optic Disc Hemorrhage — Pathophysiology
|
Retinal Scanning Laser
- To measure the microscopic anatomy of the retina and vitreoretinal interface
- To measure the effectiveness of therapy
- To help in determining the need for ongoing therapy
- To determine the safety of cessation of therapy
Visual Field Examination
- Used to assess visual function and determine the size of any associated visual field defects
- Visual field may be affected depending on the size and location of retinal hemorrhaging the extent of the visual field defect depends on size of macular edema
B-Scan Ophthalmic Ultrasound
- A two-dimensional ultrasonic scanning procedure used to produce cross-sectional images of the eye and orbit
- B-scan ophthalmic ultrasound can be used to assess internal structures of the eye when a vitreous hemorrhage prevents proper visualization and examination of the retina
- The test results are used to determine whether the retina is attached or detached
In 1953, Scheie developed a staging system for hypertensive retinopathy ranging from normal to the most severe retinal changes.
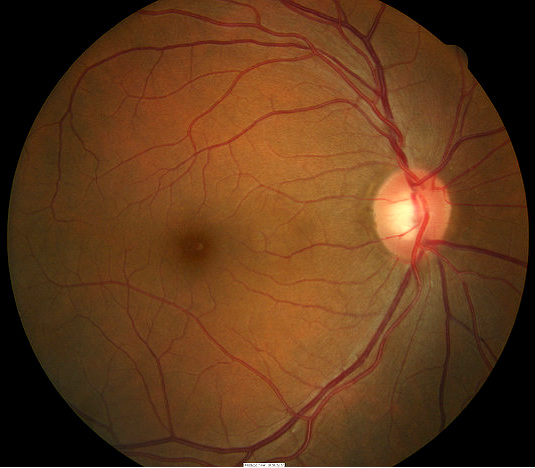 |
Grade 0 Hypertensive Retinopathy
|
|
 |
Grade 1 Hypertensive Retinopathy
|
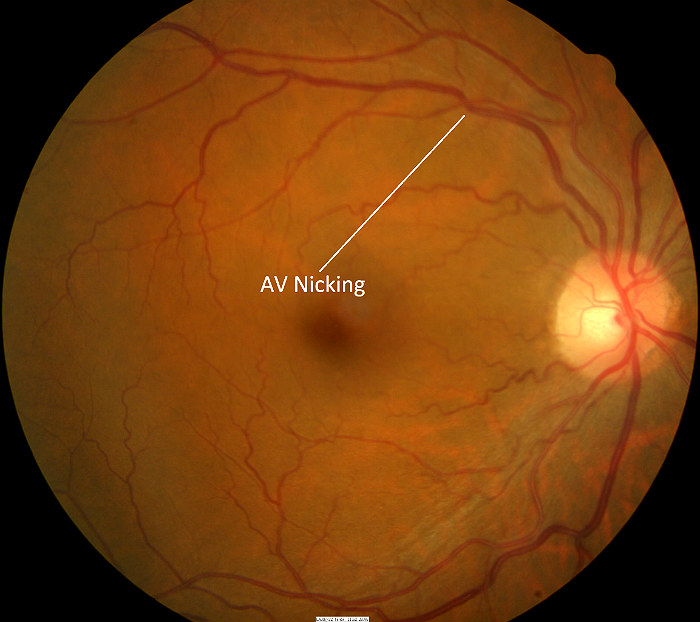 |
Grade 2 Hypertensive Retinopathy
|
|
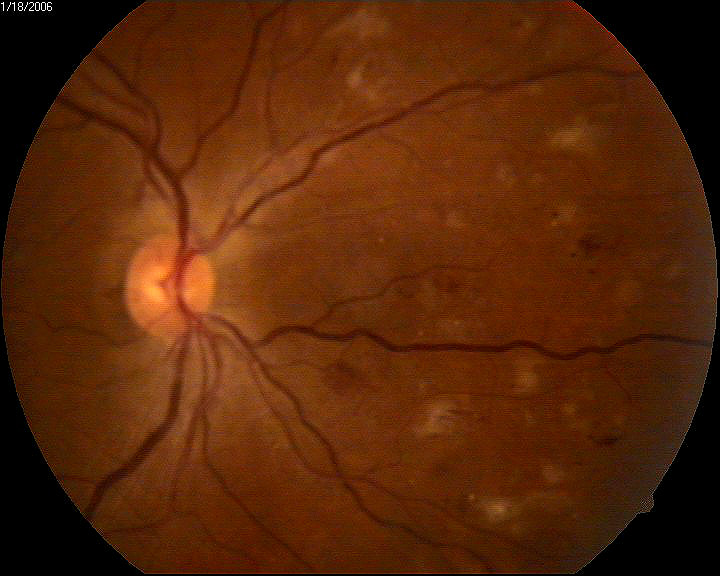 |
Grade 3 Hypertensive Retinopathy
|
|
 |
Grade 4 Hypertensive Retinopathy
All of the previously listed retinal abnormalities may be present in addition to the following:
|
 |
Diabetic Retinopathy
|
 |
Optic Disc Hemorrhage Secondary to Vitreopapillary Detachment
|
|
 |
Retinal Venous Obstruction
|
|
 |
Retinal Telangectasia
|
|
 |
Leukemia
Ocular manifestations of leukemia can produce the following retinal vessel changes
|
 |
Ocular Manifestations of HIV
|
Treatment for hypertensive retinopathy involves evaluation of secondary causes and appropriate medical co-management with the patient’s primary care doctor. Lowering blood pressure would be the primary course of action in reducing the risk of further retinal changes.
Several studies report that hypertensive retinopathy may regress over a 6-12 month period with control of elevated blood pressure.
- Patients with mild clinical signs can usually be managed with with routine care and the target blood pressure range should be based on established guidelines
- Patients with moderate clinical signs may benefit from additional assessment of vascular risk (e.g., measurement of cholesterol levels) and appropriate risk reduction therapy
- Patients with severe clinical signs need urgent anti-hypertensive treatment (e.g., intravenous medication)
The following systemic medications can be used to lower blood pressure:
- Calcium channel blockers
- Diuretics
- Angiotensin receptor blockers
- Angiotensin converting enzyme (ACE) inhibitors
- Anti-andrenergics
- Vasoconstrictors
- Renin inhibitors
And, of course, exercise and proper diet have long been a means of improving cardiovascular health.
1. Suhr C. How hypertension and high cholesterol harm the eye. RevOptom. 2014 April 15; 151(4): 34-41. http://www.revoptom.com/content/c/47790/. Last accessed August 10, 2014.
2. O’Toole L. Hypertensive Retinopathy. Optometry Today. http://www.optometry.co.uk/uploads/exams/articles/cet_02_09_2011_otoole.pdf. Last accessed July 9, 2014.
3. Theng K. Ophthalmologic Manifestations of Hypertension. Emedicine/Medscape. 2014 Mar 21. http://emedicine.medscape.com/article/1201779-overview. Last accessed July 9, 2014.
4. Hypertensive Retinopathy. Handbook of Ocular Disease Management. http://cms.revoptom.com/handbook/sect41b.htm. Last accessed July 9, 2014.
5. Wong T. McIntosh R. Hypertensive Retinopathy Signs as Risk Indicators of Cardiovascular Morbidity and Mortality. Br Med Bull (2005). http://bmb.oxfordjournals.org/content/73-74/1/57.full. Last accessed August 10, 2014.
6. Bourke K. Patel M. Prisant M. Marcus D. Journal of Clinical Hypertension. 2004 August; 6(8): 471-472. http://onlinelibrary.wiley.com/doi/10.1111/j.1524-6175.2004.3749.x/pdf. Last accessed August 10, 2014.
7. Copeland R. Ocular Manifestations of HIV Infectrion. Emedicine/Medscape. 2013 Oct 18. http://emedicine.medscape.com/article/1216172-overview#aw2aab6b5. Last accessed August 10, 2014.
362.11
Hypertensive retinopathy
92250
Fundus photography
92083
Visual field examination
92283
Color vision examination
92275
Electroretinography
92225
Extended ophthalmoscopy
92134
Macular OCT scan
Occurrence
- Hypertensive retinopathy is seen in 3-14% of adult individuals over age 39
Distribution
- Hypertensive retinopathy has no distribution characteristics
Risk Factors
- Hypertension
- Age
- Family history
- Obesity
- Smoking
- African-American




 Print | Share
Print | Share