Central retinal vein occlusion
ICD-10 Diagnosis Codes:
H34.811–Central retinal vein occlusion, right eye
H34.812–Central retinal vein occlusion, left eye
H34.813–Central retinal vein occlusion, bilateral
Title
Central Retinal Vein Occlusion
Category
Other Retinal Disorders
Description
Central retinal vein occlusion occurs when the circulation of the central retinal vein becomes obstructed.
Retinal vein occlusion is a common retinal vascular disorder. Swelling and ischemia (lack of oxygen) of the retina and glaucoma are common complications as a result. Visual symptoms can vary in severity.
Structural Damage to the Eye
- Can be an ischemic event causing retinal tissue to not be well-perfuse causing nerve fiber layer damage.
- In ischemic CRVO neovascularization of the angle and iris can result in increase pressure and complications of neovascular glaucoma creating a further insult to the nerve fiber layer over time.
- Macular edema can result as a complication.
Functional Damage to the Eye
- Vision loss and a painful eye may become permanent if the complications are not managed.
The main goal of the diagnostic evaluation for a patient with CRVO or BRVO is to accomplish the following:
- Determine the etiology of vascular disease
- Determine the extent of structural and functional damage to the eye
- Evaluate a treatment plan
Patient History
Patients with CRVO or BRVO will present with the following clinical symptoms or signs:
- Painless, gradual to sudden vision loss
- Visual disturbances such as flashes of light or floaters
- An abnormally intraocular pressure (IOP) will help differentiate CRVO versus ocular ischemic syndrome from a carotid occlusive disease. Patients with ocular ischemic syndrome will have lower IOP than patients with CRVO
- Ischemic CRVO will have a relative afferent pupillary defect
DIAGNOSTIC TESTS
Refraction
- Measurement of visual function / visual acuity
- Visual acuity of 20/400 or worse with correction along with signs of an afferent pupillary defect and visual field constriction are signs of an ischemic CRVO.
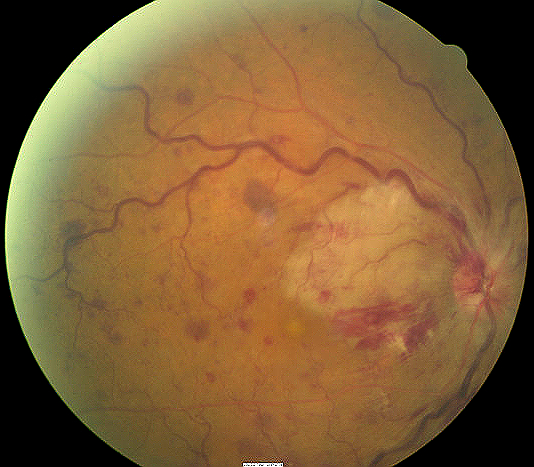
Fundus Photography
- To evaluate the optic nerve, macula and the retina
 |
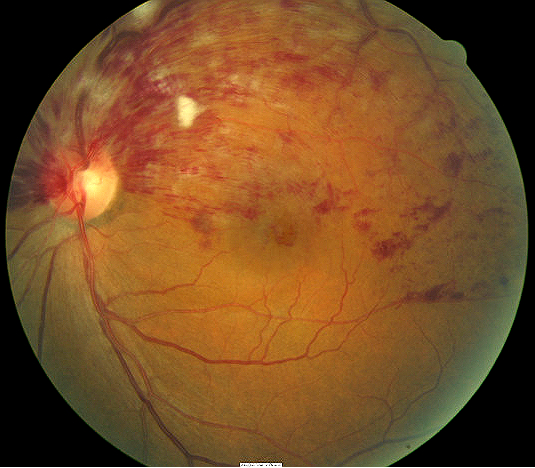 |
Extended Ophthalmoscopy
- To evaluate the optic nerve, macula and the retina
Visual Field Examination
- Visual field constriction is present
Retinal Scanning Laser
- Attenuation of the retinal nerve fiber layer
- Changes to the retinal and choroidal blood vessels
Gonioscopy
Any patient with a history of ischemic eye disease should receive a gonioscopic examination of the anterior chamber angle to look for any of the following:
- Look for abnormal angle structures
- Rule out neovascularization of the iris or angle
Systemic Evaluation
Eye doctors should consider a systemic evaluation in cases of central retinal vein occlusion. A typical investigative protocol would include the following tests:
Blood Work
- Complete blood count (CBC)
- Westergren sedimentation rate (ESR)
- Lipid profile
- Fasting blood sugar/HbA1C
- Fasting treponemal antibody absorption test (FTA-Abs)
- Reactive plasma reagin (RPR)
- Homocysteine
- Protein S and C
- Lupus anticoagulant
- SickleDex
- Rheumatoid factor
- Purified protein derivative (PPD)
- Lyme titer
- Angiotensin converting enzyme (ACE)
- Antinuclear antibody (ANA)
Ancillary Testing
- Carotid Doppler
- Electrocardiogram (EKG)
- Chest X-ray
Two types of central retinal vein occlusion are identified:
 |
Nonischemic Central Retinal Vein Occlusion
The milder form of the disease. Patients present with good vision, few retinal hemorrhages and cotton-wool spots, no relative afferent pupillary defect, and good perfusion to the retina. Nonischemic CRVO may resolve fully with good visual outcome or may progress to the ischemic type. |
|
 |
Ischemic Central Retinal Vein Occlusion
The severe form of the disease. CRVO may present initially as the ischemic type, or it may progress from nonischemic. Usually, ischemic CRVO presents with severe visual loss, extensive retinal hemorrhages and cotton-wool spots, presence of relative afferent pupillary defect and poor perfusion to retina. Other complications may arise such as neovascular glaucoma and a painful blind eye. Ischemic CRVO can be better distinguished with fluorescein angiography. |
Ocular Ischemic Syndrome (Carotid Occlusive Disease)
Patient will have dilated and irregular veins, but they will not be tortuous like in CRVO. Neovascularization is present in a third of patients, but disc edema and hemorrhage are not common. Retinal hemorrhages are found in the mid-periphery of the retina. There will be a history of transient ischemic attacks, amaurosis fugax and orbital pain. Intraocular pressures are is usually low.
Diabetic Retinopathy
The hemorrhages and microaneurysms are concentrated in the posterior pole and exudates are more common. It is usually bilateral.
Papilledema
There will be bilateral disc swelling with flame-shaped hemorrhages around the disc, but not into the peripheral retina. Etiology is caused from increased intracranial pressure rather from a vascular etiology
Radiation Retinopathy
There is a history of radiation therapy. Patients will have disc swelling and retinal neovascularization, and cotton wool spots.
No known effective medical treatment is available for either the prevention of or the treatment of central retinal vein occlusion (CRVO). Identifying and treating the systemic medical problems is the best treatment to reduce further complications from CRVO.
Vein occlusions are often associated with systemic disease, so co-manage these patients with an internist. Since the exact pathogenesis of CRVO is unknown, various medical modes of treatment are available with varying success in preventing complications and in preserving vision.
The following treatments are advocated:
- Aspirin
- Anti-inflammatory agents
- Isovolemic hemodilution
- Plasmapheresis
- Systemic anticoagulation with warfin, heparin and alteplase
- Fibrinolytic agents
- Systemic corticosteroids
- Local anticoagulation with intravitreal injection of alteplase
Although fluorescein angiography is the gold standard in assessing retinal vascular disease, it is not indicated initially for CRVO patients because the fresh hemorrhage will block transmission and reveal no useful information. In the later course of the occlusion, fluorescein angiography will give information about retinal capillary perfusion and whether or not the occlusion is ischemic and therefore more likely to develop neovascularization.
Laser Therapy
Laser photocoagulation is the treatment of choice in complications associated with retinal vascular diseases (i.e. diabetic retinopathy, branch retinal vein occlusion). Panretinal photocoagulation (PRP) has been used in the treatment of neovascular complications of CRVO for a long time. However, no definite guidelines exist regarding exact indication and timing of PRP.
Pan-retinal photocoagulation: Research shows that ischemic retinal vein occlusion does not benefit from prophylactic pan-retinal photocoagulation. Use this procedure only if the patient develops neovascularization of the iris, disc or retina.
Monitor patients with serial ophthalmoscopy, fundus photography and gonioscopy monthly until things start to resolve. Observe the patient for neovascularization of the disc, retina, iris and angle. Follow patients with ischemic CRVO every two weeks looking for neovascularization in the iris. After three months, follow patients monthly. If neovascularization develops, pan-retinal photocoagulation is recommended.
Focal laser photocoagulation: If patient has a BRVO and vision is reduced between below 20/40 because of macular edema, then patients may benefit from focal laser photocoagulation at 3-18 months after the onset of the occlusion. CRVO patients with reduced vision due to macular edema do not benefit from focal laser photocoagulation.
Intravitreal Injection
Intravitreal injection of triamcinolone (0.1 mL/4 mg) shown to be effective in resolving the edema and in improvement of the vision. Complications with injection of triamcinolone include cataract, glaucoma, retinal detachment, vitreous hemorrhage, and endophthalmitis.
Intravitreal injection of bevacizumab (0.05 mL/1.25 mg) has been effective in improving the edema and the vision. It can also decrease angle neovascularization and improved intraocular pressure control for patients with neovascular glaucoma. Complications with injection of triamcinolone include cataract, glaucoma, retinal detachment, vitreous hemorrhage, and endophthalmitis.
Intraocular Surgery
Radial optic neurotomy (RON) is a new surgical technique in which a microvitreoretinal blade is used during pars plana vitrectomy to relax the scleral ring around the optic nerve. The central retinal artery and vein passes through the narrow openings of the cribriform plate in the optic disc. If the procedure is successful, it decompresses the closed compartment and leads to an improvement in venous outflow and a reduction of macular edema. This procedure may work better for patients with nonischemic CRVO. Complications such as significant hemorrhage and neovascularization at the incision site can occur.
Chorioretinal venous anastomosis is performed by creating an anastomosis to bypass the site of venous occlusion. Using a laser or surgery, retinal veins are punctured through the retinal pigment epithelium and the Bruch membrane into the choroid, therefore developing other channels into the choroid. This procedure reduces macular edema and may improve vision in nonischemic CRVO. The success rate is low and the complication rate can be quite high. Complications include vitreous hemorrhages and choroidal neovascularization at the anastomosis site. The exact indication and timing of the procedure has not been clearly studied.
Vitrectomy is a technique in which the vitreous is surgically removed along with the posterior hyaloid. One theory is a vitrectomy may help reduce traction on the macula and this in turn reduces the macular edema. Another theory hypothesis that removing the vitreous removes the cytokines and VEGF associated with a venous occlusive episode. There is no evidence that a vitrectomy is the best treatment.
1. Kooragayala L. Central Retinal Vein Occlusion. Medscape/EMedicine. 20 Feb 2014. http://emedicine.medscape.com/article/1223746-overview. Last accessed August 17, 2014.
2. Retinal Vein Occlusion. Handbook of Ocular Disease Management. http://www.reviewofoptometry.com/cmsdocuments/2010/4/ro0410_hndbk.pdf. Last accessed January 21, 2015.
3. Sowka J. Kabat A. Occlusion Conclusions. RevOptom. 14 May 2010. http://www.revoptom.com/content/d/therapeutic_review/i/1104/c/20809/. Last accessed August 17, 2014.
362.35
Central retinal vein occlusion
92250
Fundus photography
92225
Extended ophthalmoscopy
92083
Visual field examination
92134
Macula OCT scan
92283
Color Vision Examination
92275
Electroretinography
Occurrence
- The prevalence of central retina vein occlusion is about 0.5% of the population
- CRVO is the second most common retinal vascular disorder
Distribution
- CRVO is distributed evenly throughout the population
Risk Factors
- CRVO occurs in all age groups, but more than 90% of CRVO cases occur in patient after the age of 50
- CRVO occurs slightly more frequently in males than in females




 Print | Share
Print | Share