ICD-10 Diagnosis Codes:
H33.011–Retinal detachment, single break, right eye
H33.012–Retinal detachment, single break, left eye
H33.013–Retinal detachment, single break, bilateral
Title
Retinal Detachment with Retinal Defect
Category
Retinal Detachments And Defects
Description
Retinal detachment is a separation of the inner layers of the retina from the underlying retinal pigment epithelium (RPE) and the choroid.
Retinal detachment is a separation of the inner layers of the retina from the underlying retinal pigment epithelium (RPE) and the choroid. Three basic mechanisms can cause the separation of the sensory retina from the underlying RPE.
- Rhegmatogenous retinal detachment
- Exudative or serous retinal detachment
- Tractional retinal detachment
Structural Damage to the Eye
- Separation of sensory retinal tissue to underlying retinal pigment epithelium and choroid due to holes, tears or breaks
- Accumulation of subretinal fluid in inappropriate places
- Traction from inflammatory or vascular fibrous membranes causes adhesions between the vitreous gel and the retina leading to detachments
- Note any history of trauma or injuries to the eye or head
- Note any recent or past eye surgeries
The main goal of the diagnostic evaluation in a patient with retinal detachment is to accomplish the following:
- Determine if the location of the retinal detachment
- Determine the underlying cause or etiology of the retinal detachment
- Determine the severity and assess the time frame of the referral
Patient History
Patients with retinal detachments will present with one or more of the following symptoms:
- Increase of floaters
- Flashes of light
- Black curtain or film over their eye
The following clinical signs may be abnormal:
- Look for an abnormal pupil response (i.e., a fixed pupil can mean previous trauma)
- Gross visual fields may be affected if the retinal detachment is large enough
- Intraocular pressure may decrease by > 4-5 mm Hg in the affected eye in comparison to the unaffected eye
- Biomicroscopy may show an absence of orange light reflex
DIAGNOSTIC TESTS
The following diagnostic tests can provide clinical information in the evaluation of the extent and location of the retinal detachment.
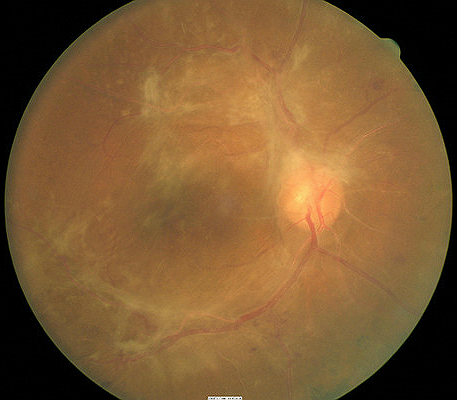
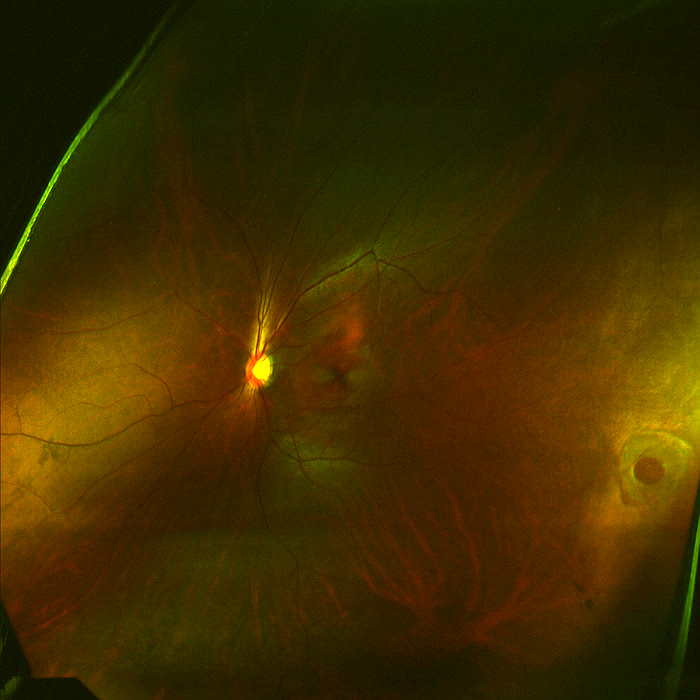
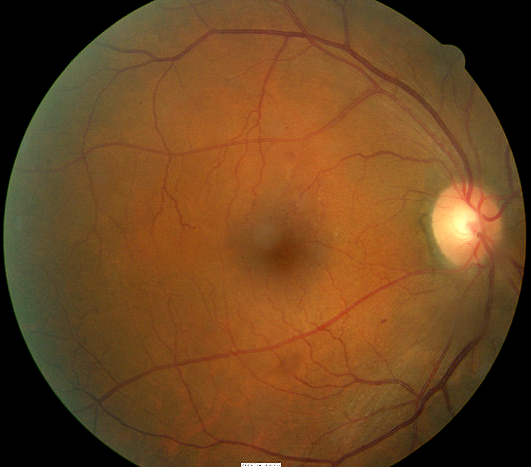
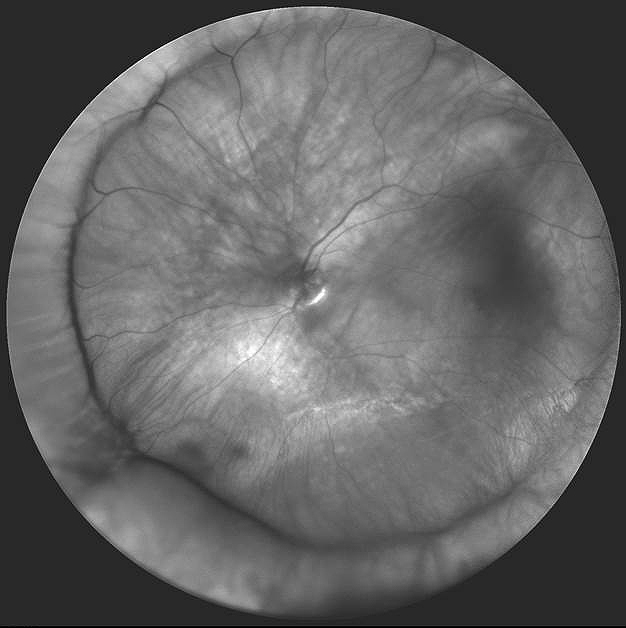
Fundus Photography
- Document the location of the retinal detachment
- Helps document retinal appearance preoperatively and postoperatively
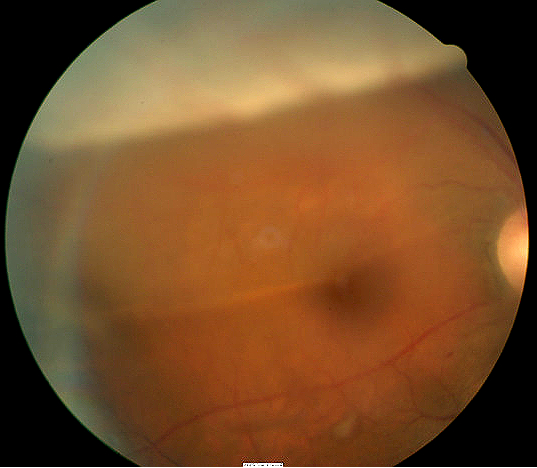
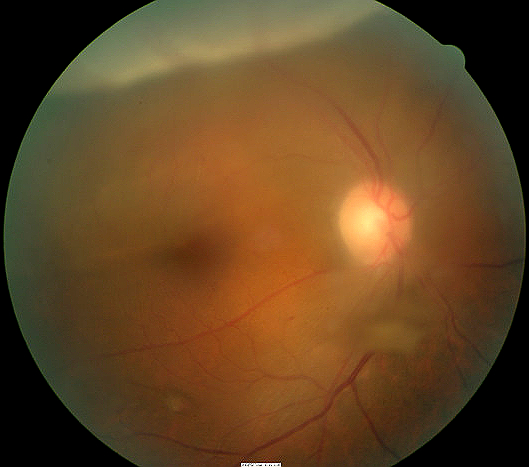
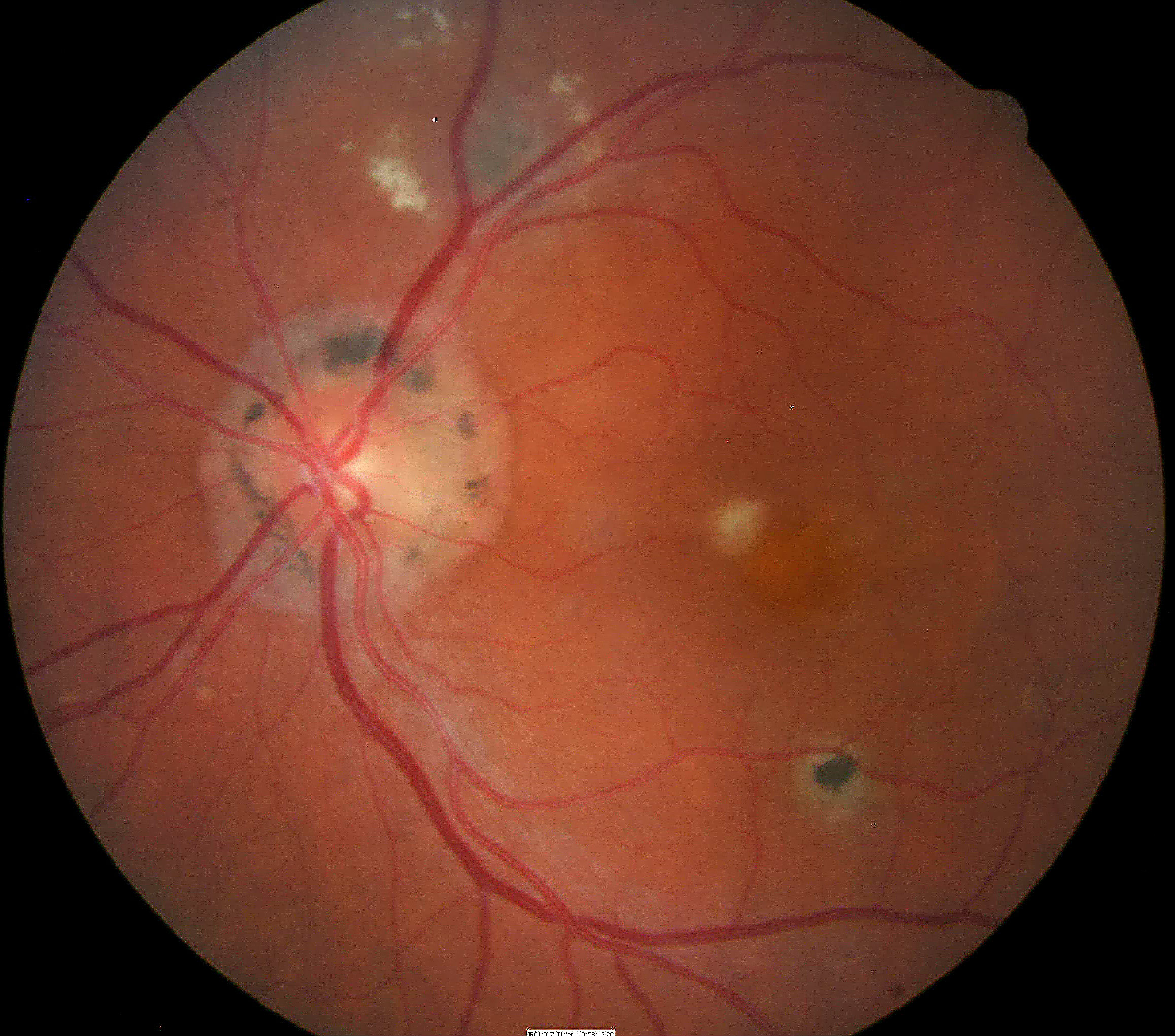
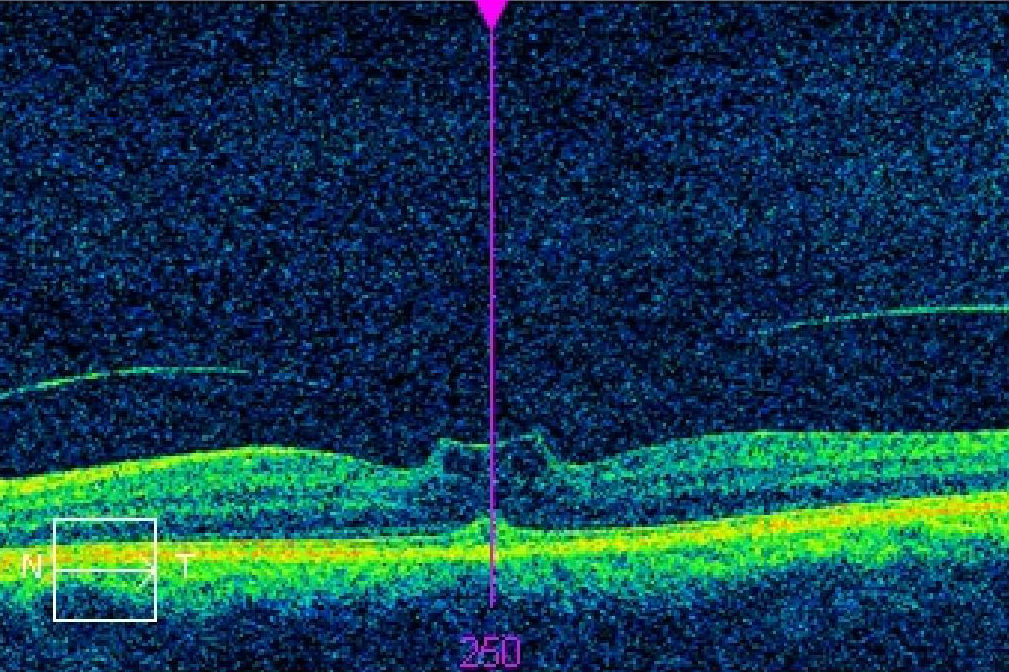
Retinal detachment in the right eye — preoperative |
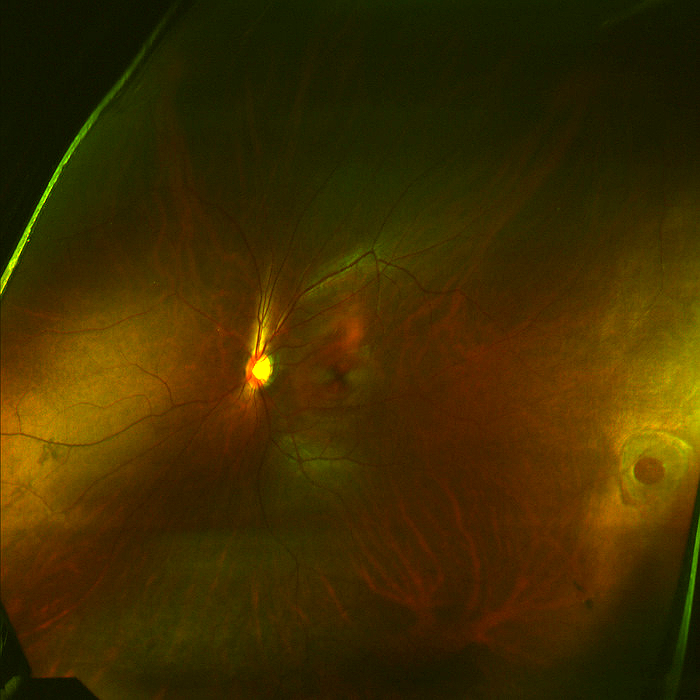
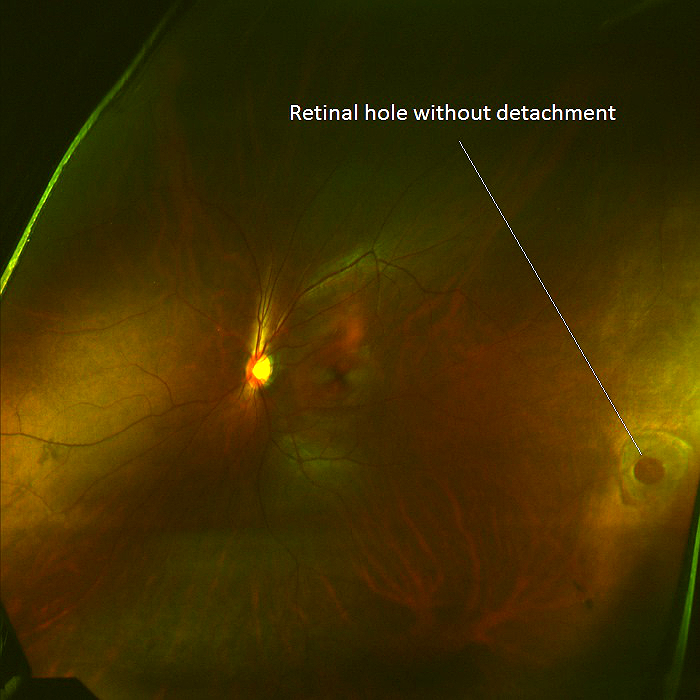
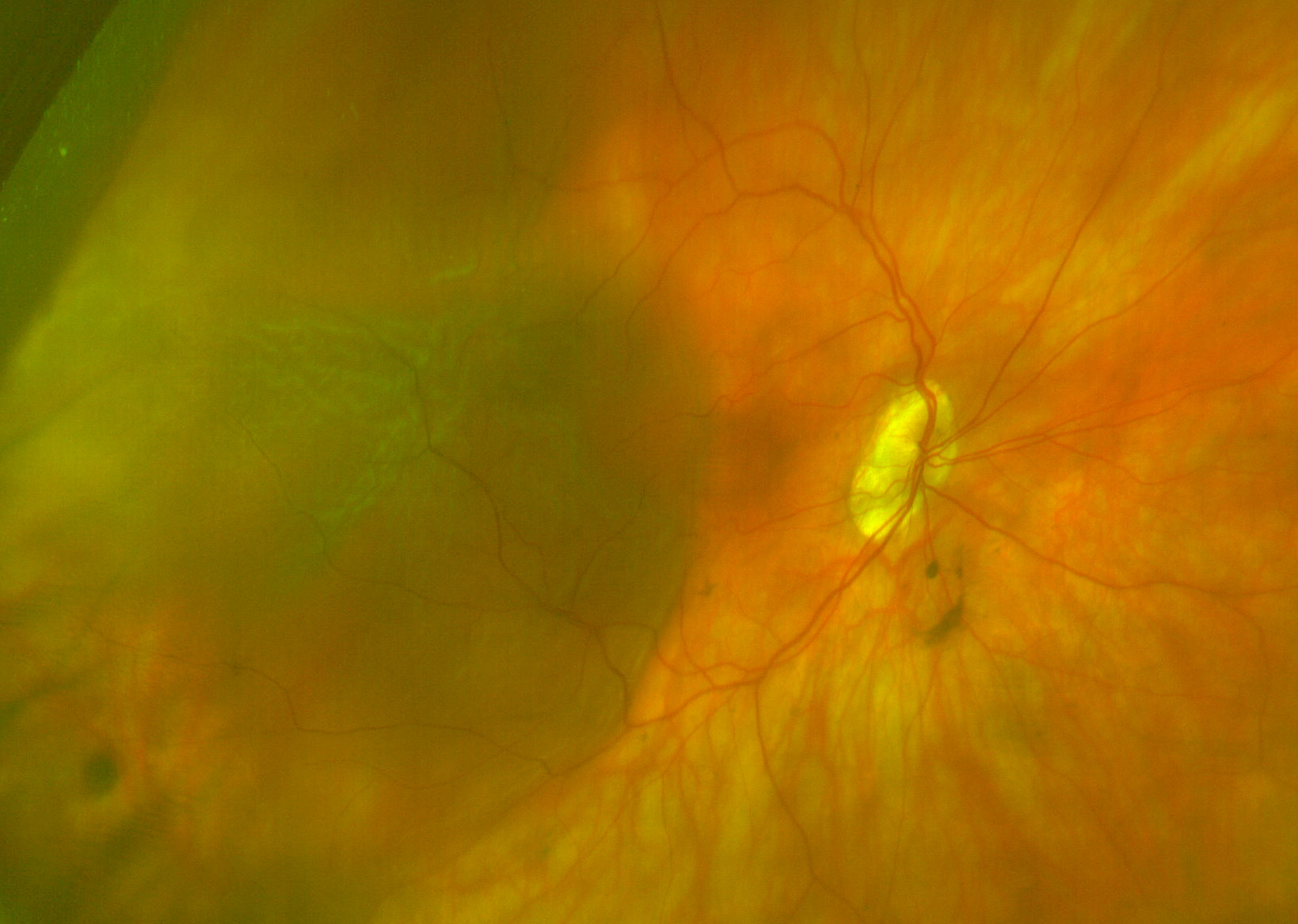
Postoperative appearance after surgical reattachment |
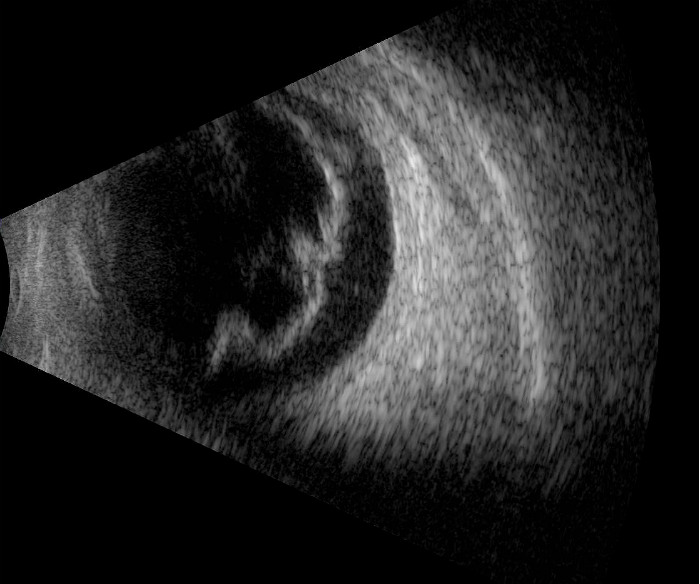
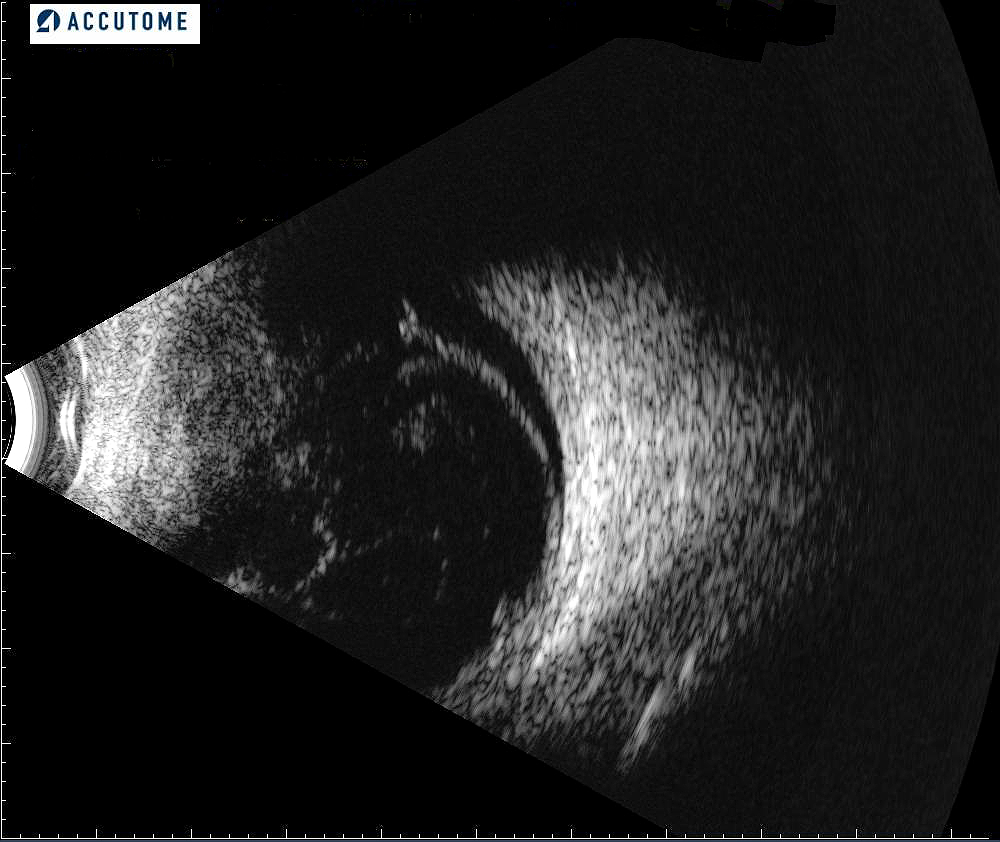
B-Scan Ophthalmic Ultrasound
B-scan ultrasound uses transducer scanning and electronic processing to “image” the internal structures of the eye and orbit.
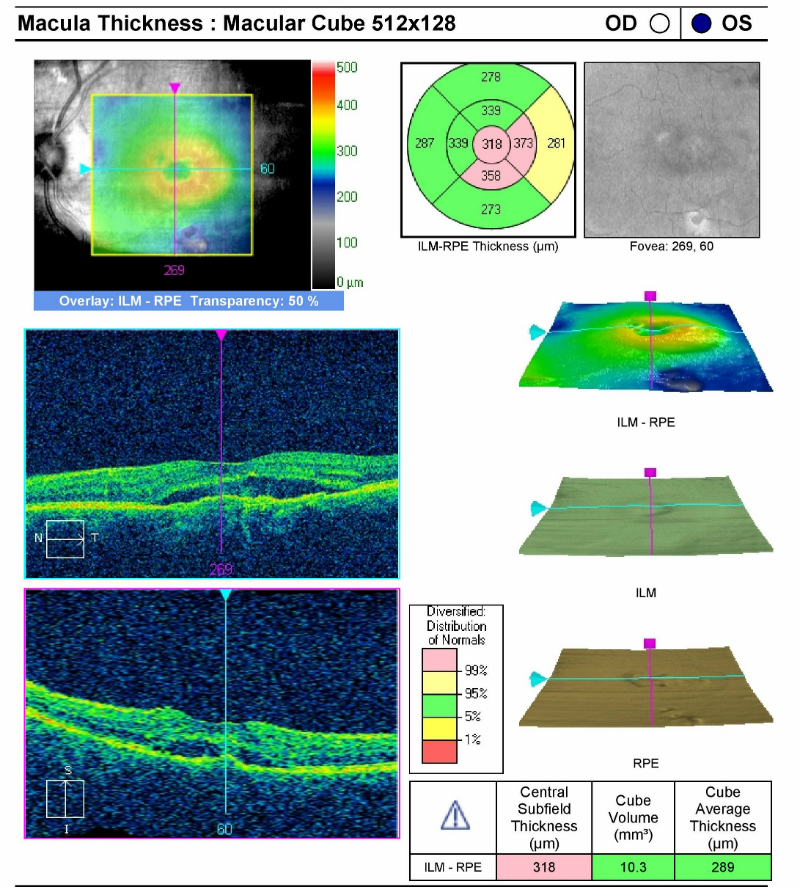
Retinal Scanning Laser
This test can show the separation of the sensory retina and reveal the presence of fluid in the retina.
Extended Ophthalmoscopy
This test can be use to document holes, tears or breaks in the peripheral retina with or without scleral depression.
There are three categories of retinal detachments:
For Rhegmatogenous Retinal Detachment
- Posterior vitreous detachment
- Peripheral retinal lesions (i.e., lattice degeneration, cystic retinal tufts)
- Colobomas of the choroid and retina
- Intraocular inflammation and/or infection
- cytomeglavirus retinitis
- ocular toxocariasis
- ocular toxoplamosis
- pars planitis
For Exudative Retinal Detachment
- Primary tumors (i.e., choroidal malignant melanoma, choroidal hemagioma, retinoblastoma)
- Metastatic carcinoma to the choroid (i.e., breast cancer, lung cancer)
- Inflammation (i.e., choroiditis, retinitis)
- Vascular disease
- Telangiectasia retina
- Juvenile and Adult Coat’s disease
- Retinal vein occlusion
- Optic nerve disease
- Optic disc pit with serous detachment of the macula
- Nerve head drusen with detachment of adjacent retina
- Macular disease
- Central serous chorioretinopathy
- Age-related macular degeneration
- Ocular histoplasmosis
- Angioid streaks, high myopia (>6 diopters)
- Systemic diseases (i.e., systemic lupus erythematosus, leukemia)
For Tractional Retinal Detachment
- Proliferative diabetic retinopathy
- Sickle cell disease
- Retinopathy of prematurity
- Cataract surgery with vitreous loss
Lesions that Simulate Retinal Detachment
- Transient ischemic attack or cerebrovascular episodes
- Retinal artery occlusion
- Optic neuritis
- Atypical migraine
- Vitreous (i.e., membranes, hemorrhages, inflammation)
- Choroidal detachment
Retinal diseases:
- Primary and secondary retinoschisis
- Retinopathy of prematurity
- Diabetic retinopathy
- Retinal artery occlusion
Surgery for Retinal Tear
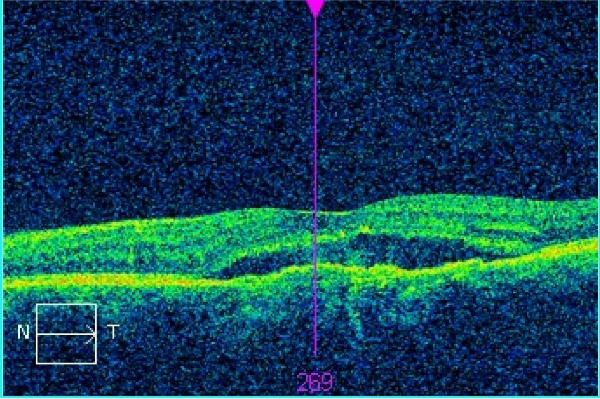
For retinal holes or tears that have not advanced to a retinal detachment, preventative measures can be taken with the following procedures:
Laser Photocoagulation
- A laser is used to make burn marks around the retinal hole or tear to encourage scarring
- This scarring welds together the underlying tissue and prevents the tear from developing into a retinal detachment
Freezing (cryopexy)
- A freezing probe applied to the outer surface of the eye is used to freeze the retina around the retinal tear
- This technique freezes the area around the hole, leaving a scar to secure the retina to the eye wall
- It is generally used for hard-to-reach tears
Surgery for Retinal Detachment
If a retinal attachment has occurred the following procedures are utilized. The type, size and location of any retinal detachment determines the technique used.
Pneumatic Retinopexy
This procedure is used for an uncomplicated detachment with the tear located in the upper region of the retina.Cryopexy is used to treat the retinal tear first. A bubble of expandable gas is injected into the vitreous cavity. Over the course of a few days, the gas bubble expands sealing the retinal tear by pushing against it and the detached area surrounding the tear. Since no new fluid is passing through the retinal tear, the previously accumulated fluid is absorbed, and the retina is able to reattach itself to the back wall of your eye. The gas eventually disappears on its own in several weeks.
Scleral Buckling
This is the most common technique for repairing retinal detachment. Cryopexy is used to treat the retinal tear first. Then a small piece of silicone sponge or silicone rubber is attached to the sclera over the affected area. The silicone material indents the wall of the eye, therefore, creating a buckling effect and reducing traction of the vitreous on the retina. The silicone material is stitched to the outer surface of the sclera. A small cut in the sclera can be made to drain any fluid collected under the detached retina before tying the sutures to hold the buckle in place. The scleral buckle remains in place for the rest of the patient’s life.
Scleral buckle |
Scleral Buckle
|
Vitrectomy
Sometimes removing part of the vitreous is necessary when vitreous clouding prevents a view of the detached retina or retinal scarring limits the effectiveness of pneumatic retinopexy or scleral buckling. Scar tissue or opaque areas of the vitreous are removed, while the volume of removed tissue is balanced with salt solution to maintain the normal pressure and shape of the eye. After the vitrectomy, other surgical techniques are used to repair the retinal tear or detachment.
Pharmacologic Treatment for Retinal Detachment
Anti-VEGF Therapy
In patients with retinal disease and subsequent subretinal fluid accumulation, intraocular injectables such as Lucentis, Avastin, or Eylea may be the best treatment options
1. Fabrykowski, MC. Evolving therapies for diabetic macular edema. Rev Optom 2013 Dec 15; 150(12): 52-56.
361.00
Retinal detachments and defects
92015
Refraction
92083
Visual field examination
92250
Fundus photography
76512
B-Scan ophthalmic ultrasound
92225
Extended ophthalmoscopy
92134
Macula OCT scan
Occurrence
The prevalence of retina detachments is 0.3% of the population.
Distribution
- Retinal detachments are not distributed evenly throughout the population
- Retinal detachments are more common in people older than age 40
- Jewish decent have a higher risk
Risk Factors
- High myopia ( >6 diopters)
- Age (more common in people older than age 40)
- Previous retinal detachment in one eye
- A family history of retinal detachment
- Previous eye surgery, such as cataract removal
- Previous severe eye injury or trauma
- Weak areas in the peripheral retina




 Print | Share
Print | Share