Hyphema secondary to blunt ocular trauma
ICD-10 Diagnosis Codes:
H21.01–Hyphema, right eye
H21.02–Hyphema, left eye
H21.03–Hyphema, bilateral
Title
Hyphema of Iris and Ciliary Body
Category
Disorders Of The Iris And Ciliary Body
Description
Hyphema is a condition where blood from the iris or ciliary body hemorrhages into the anterior chamber. A hyphema may appear as a few red blood cells or it can completely fill the anterior chamber
Hyphema is a condition where blood from the iris or ciliary body hemorrhages into the anterior chamber. A hyphema may appear as a few red blood cells or it can completely fill the anterior chamber.
 |
Traumatic Hyphema
|
1. Traumatic hyphema is usually a result of blunt force injury to the eye or orbit. In addition to the original hemorrhage, a secondary hemorrhage can occur at an time up to one week after the original injury.
2. Iatrogenic hyphema can occur intraoperatively during a surgical procedure or at any time postoperatively.
3. Non-traumatic hyphema can occurs spontaneously if it is associated with the following conditions:
- Neovascularization of the iris
- Neovascularization in the anterior chamber angle
- Iris lesions
- Malpositioned/loose intraocular lens
Structural Damage to the Eye
1. Blood in the trabecular meshwork can result in slowed aqueous drainage
2. Obstruction to aqueous outflow can produce a secondary glaucoma
3. Methods of hyphema formation during intraocular surgery include the following:
- Intraoperative bleeding — ciliary body or iris gets injured during a peripheral iridectomy, cataract extraction, cyclodialysis, or filtration procedure
- Early postoperative bleeding — a traumatized uveal blood vessel in spasm earlier and suddenly dilates or conjunctival bleeding that makes its way into the anterior chamber via a corneoscleral wound or sclerostomy
- Late postoperative bleeding — new blood vessels growing across the corneoscleral wound that bleed when manipulated; a uveal wound that is reopened; an intraocular lens that is causing chronic iris erosion
Functional Damage to the Eye
- Transient vision loss
- Permanent vision loss secondary to corneal blood staining
- Permanent vision loss secondary to glaucoma
The main goal of the diagnostic evaluation in a patient with hyphema is to accomplish the following:
- Identify the cause of the hyphema
- Evaluate any structural damage to the orbit and the eye
- Identify and exclude differential diagnoses
- Prescribe a treatment program
The patient history, a general medication observation, an examination of the gross visual fields, a basic sensorimotor examination, the adnexal examination, the external examination with biomicroscopy and ophthalmoscopy will be necessary to gain all the information required to make a clinical diagnosis of hyphema and its potential complicatons.
Patient History
Patients with hyphema may present with any of the following abnormal clinical signs and symptoms:
- Recent history of trauma
- Pain
- Blurred vision
- Swelling of the lids
- Foreign body sensation
- Redness of the eye
- Transient blurred vision
- Loss of vision
- Double vision
Adnexal Examination
Trauma to the adnexa will have all the signs and symptoms associated with blunt trauma to the eyelids or the orbit. To rule out orbital fracture or extraocular muscle entrapment, X-ray or CT scan may be necessary.
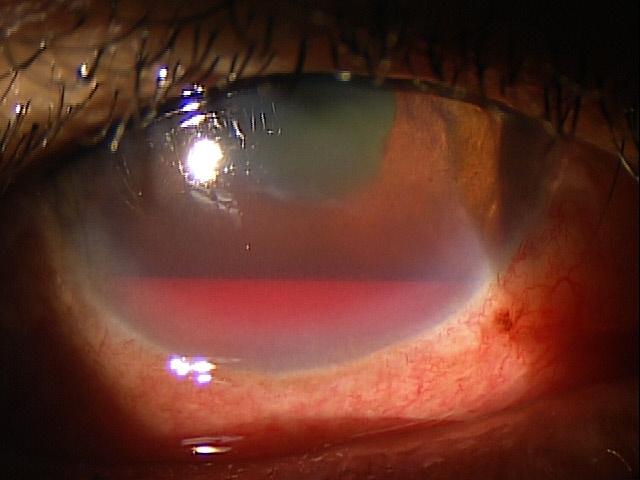
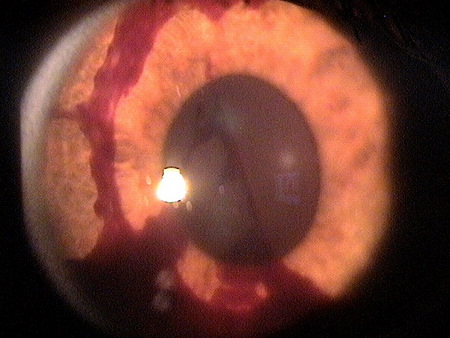
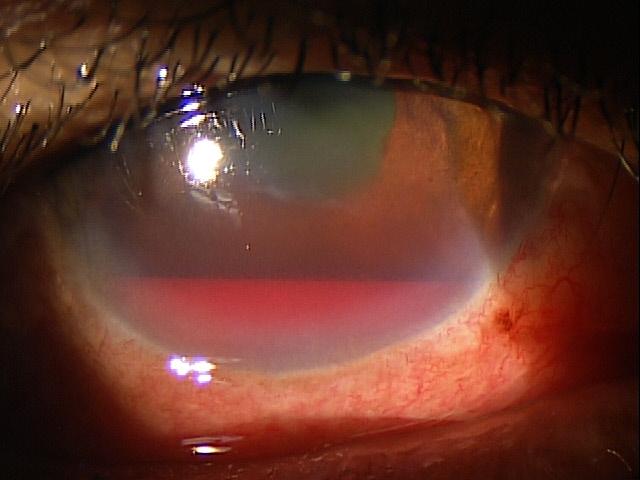
| External Ocular Examination with Biomicroscopy
The external ocular examination with biomicroscopy may reveal many of the clinical signs of a hyphema.
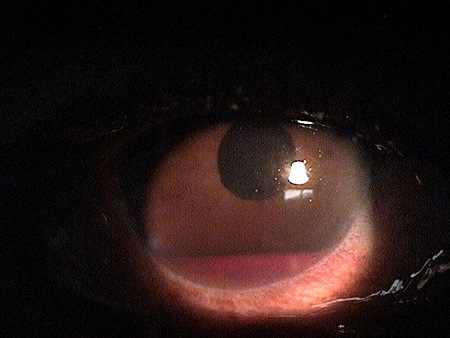
Hyphema with secondary hemorrhage 1 day after initial blunt trauma to the eye. |
 |
 |
Clinical Appearance of the Cornea
|
|
Clinical Appearance of the Anterior Chamber
|
 |
Ophthalmoscopic Examination
In cases of blunt ocular trauma, a dilated fundus examination without scleral depression is needed to rule out retinal detachment or other contusion damage to the retina.
DIAGNOSTIC TESTS
External Ocular Photography
The clinical application of external ocular photography is the documentation, monitoring and treatment of any pathological conditions that affect the external structures of the eye and the anterior segment of the eye.
- Document the location and extent of the hyphema.
- Document any other associated structural changes to the cornea and the eyelids.
- Help plan a treatment program for hyphema.
The information provided by external ocular photography is used for medical decision-making in the following manner:
- To document the progress or lack of progress of the hyphema
- To document the delivery of medical treatment
- To document the response to treatment
Gonioscopy
The clinical application of gonioscopy is the documentation, monitoring and treatment of any pathological conditions that affect the anterior segment of the eye.
- Document the location and the extent of the hyphema
- Document any structural changes to the iris or the anterior chamber angle of the eye
- Document any obstruction to aquesous outflow secondary to the hyphema
- Help plan a treatment program for hyphema
The information provided by gonioscopy is used for medical decision-making in the following manner:
- To document the progress or lack of progress of the hyphema
- To assess the risk of developing secondary glaucoma
- To document the delivery of medical treatment
- To document the response to treatment
B-Scan Ophthalmic Ultrasound
The clinical application of B-scan ophthalmic ultrasound is the documentation, monitoring and treatment of any pathological conditions that affect the external structures of the eye, the anterior segment of the eye or the posterior segment of the eye. B-scan is used when the hyphema or a vitreous hemorrhage prevents the proper visualization and examination of the retina.
- Document the status of the retina after blunt ocular trauma
- Document any other associated structural changes to the eye, extraocular muscles or the orbit
- Identify and exclude other causes of the hyphema such as intraocular foreign body or intraocular tumor
- Help plan a treatment program for the hyphema
Information provided by the B-scan ophthalmic ultrasound is used for medical decision-making in the following manner:
- To document the level of structural damage to the eye following blunt ocular trauma
- To assist in identifying and excluding differential diagnoses
- To document the delivery of medical treatment
- To document the response to treatment
There are two broad ways to classify blood in the anterior chamber — microhyphema and hyphema. Microhyphema is suspended red blood cells in the anterior chamber seen with a slit-lamp examination. Hyphema is a layer or clot of blood easily seen without a slit-lamp examination.
In addition, the Hyphema Clinical Grading System classifies hyphemas by the height of the blood in the anterior chamber.
| Hyphema Clinical Grading System
Grade 1 — Layered blood occupying less than 1/4 of the anterior chamber Grade 2 — Blood filling 1/4 to 1/2 of the anterior chamber Grade 3 — Layered blood filling 1/2 to 3/4 of the anterior chamber Grade 4 — Total clotted blood (referred to as a “blackball” or “eight-ball” hyphema |
 |
|
|
|
Sickle Cell Traits/Disease
African-American and Mediterranean patients should be screened for systemic disease if a spontaneous hyphema is diagnosed.
Juvenile Xanthogramuloma
A dermalogical disorder primarily in infants and children can have manifestations of recurrent, spontaneous hyphemas due to uveal tract involvement.
Retinoblastoma
Microhyphemas may be present due to the intraocular tumor.
Most clinicians can manage patients with hyphema with one or more of the following treatment options:
Palliative Treatment
- Confined bed rest to limited activity depending on the severity of the hyphema
- Elevate head 30 degrees
- No strenuous activity permitted
- Place clear plastic shield over eye at all times
- NO aspirin-containing products or NSAIDs
Pharmacological Treatment
- Mild analgesic for pain and discomfort – no sedatives (acetaminophen)
- Cycloplegia (1% cyclogyl, 5% homatropine, 1% atropine)
- Topical steroid (prednisolone acetate 1%)
- Beta-blocker if the pressure is above 27mm Hg
- Carbonic anhydrase inhibitor (oral acetazolamide 250mg) if the pressure is above 35mm Hg until the pressure is adequately controlled
- Topical antibiotic prophylactically if corneal epithelial defects is present
- Follow up daily until condition shows improvement and taper medications accordingly
Surgical Treatment
If the hyphema does not resolve as expected, the following surgical procedures can be performed:
- Hyphema evacuation with closed vitrectomy instrumentation
- Paracentesis
- Irrigation and aspiration through a small incision
- Clot irrigation with trabeculectomy
1. Sheppard J. Hyphema. Medscape/EMedicine. http://emedicine.medscape.com/article/1190165-overview. Last accessed August 16, 2014.
2. Hyphema. Handbook of Ocular Disease Management. http://www.reviewofoptometry.com/cmsdocuments/2012/6/ro0612_hndbk_em.pdf. Last accessed August 16, 2014.
364.41
Hyphema of iris and ciliary body
92285
Extrernal ocular photography
92020
Gonioscopy
76512
B-scan ophthalmic ultrasound
76513
Anterior segment ultrasound
92286
Specular endothelial microscopy
Occurrence
The frequency of hyphema is about 17-20 per 100,000 people per year.
Distribution
Hyphemas are distributed evenly throughout the population.
Risk Factors
- Young males have a higher tendency to be involved in blunt ocular trauma
- Older patients are at a higher risk due to intraocular surgeries
- Sickle cell anemia
- Blood dyscrasias and coagulopthies




 Print | Share
Print | Share