ICD-10 Diagnosis Codes:
H18.731–Descemetocele, right eye
H18.732–Descemetocele, left eye
H18.733–Descemetocele, bilateral
Title
Descemetocele
Category
Corneal Opacity And Other Disorders Of Cornea
Description
Descemetocele involves the anterior bulging or rupture of an intact Descemet’s membrane through a defect of the overlying corneal stroma and epithelium.
A corneal descemetocele can be associated with any corneal disease or injury that produces a defect in the corneal stroma and epithelium. The following traumatic, infectious or inflammatory conditions can all produce a corneal descemetocele with secondary corneal perforation:
Corneal Trauma
- Refractive surgery
- Penetrating injury
- Chemical injury
Bacterial Infection
- Pseudomonas aeurginosa
- Staphylococcal species
- Streptococcus species
- Moraxella species
- Salmonella species
Viral Infection
- Herpes simplex
- Herpes zoster
Fungal Infection
- Fusarium solani
- Aspergillus fumigatus
- Penicillium citrinum
- Candida albicans
- Cephalosporium
- Curvularia
Inflammatory Disease
- Rheumatoid arthritis
- Systemic lupus erythematosus
- Wegener’s granulomatosis
- Polyarteritis nodosa
- Sarcoidosis
- Inflammatory bowel disease
- Mooren’s ulcer
Other Corneal Diseases
Exposure keratitis
Degeneration and ectasia
- Keratoconus
- Terrien’s marginal degeneration
- Pellucid marginal degeneration
Dry eye and xerosis
- Keratoconjuncitivis sicca
- Vitamin A deficiency
- Ocular cicatricial pemphigoid
- Stevens johnson syndrome
- Sjogren’s syndrome
- Graft-versus-host disease
Other Causes
- xxxx
- xxxx
Structural Damage to the Eye
- Disease or injury produces a defect in the corneal stroma and epithelium
- Intact Descemet’s membrane bulges through the overlying corneal defect
- Descemet’s membrane ruptures
- Corneal edema
- Corneal perforation
- Loss of the eye
Functional Damage to the Eye
- None
- Decreased visual acuity
Care should be taken to minimuze pressure on the eyeball while examining a patient with a descemetocele or a suspected descemetocele.
The main goal of the diagnostic evaluation in a patient with a descemetocele is to accomplish the following:
- Determine if corneal perforation is imminent
- Decide on the best treatment option or combination of options
Patient History
- Sudden decrease in visual acuity
- Ocular pain
- Increased tear production
External Ocular Examination with Biomicroscopy
- Look for folds in Descemet’s membrane at the base of any corneal ulceration
- Look for a central clear zone within areas of corneal thinning
Look for clinical signs of corneal perforation
- Uveal prolapse
- Positive Seidel test
- Flat or shallow anterior chamber
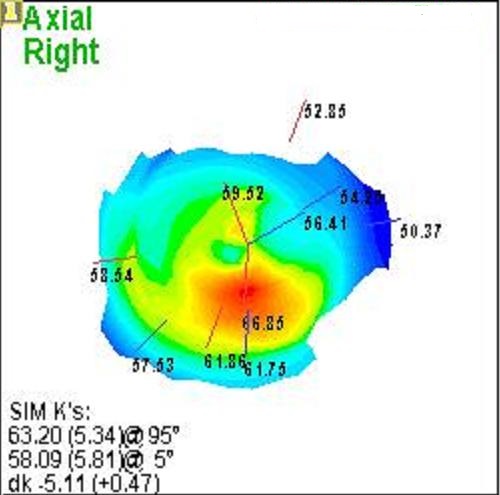
Anterior Segment Imaging
- xxxx
- xxxxx
 |
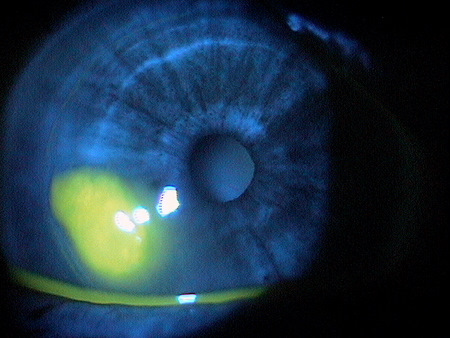
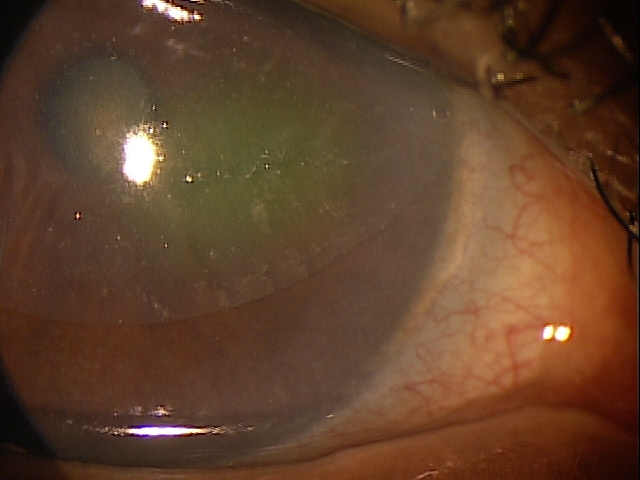
Pre-Descemetocele Image of Cornea
|
|
 |
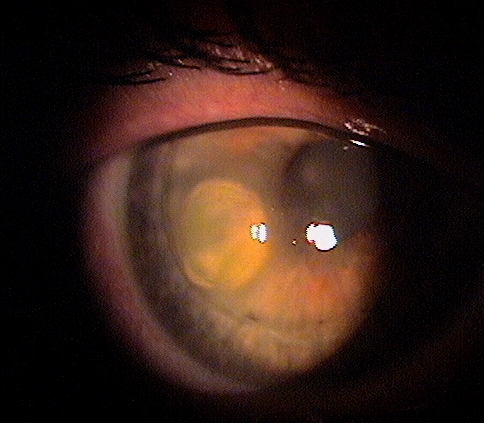
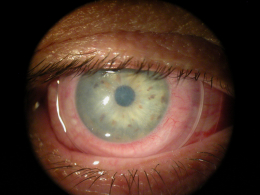
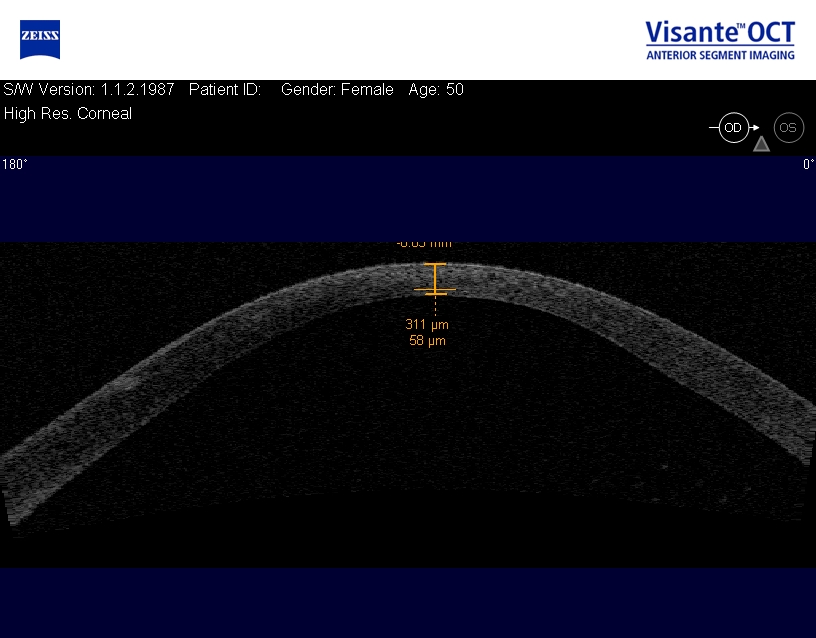
Corneal Descemetocele with Secondary Corneal Edema
|
|
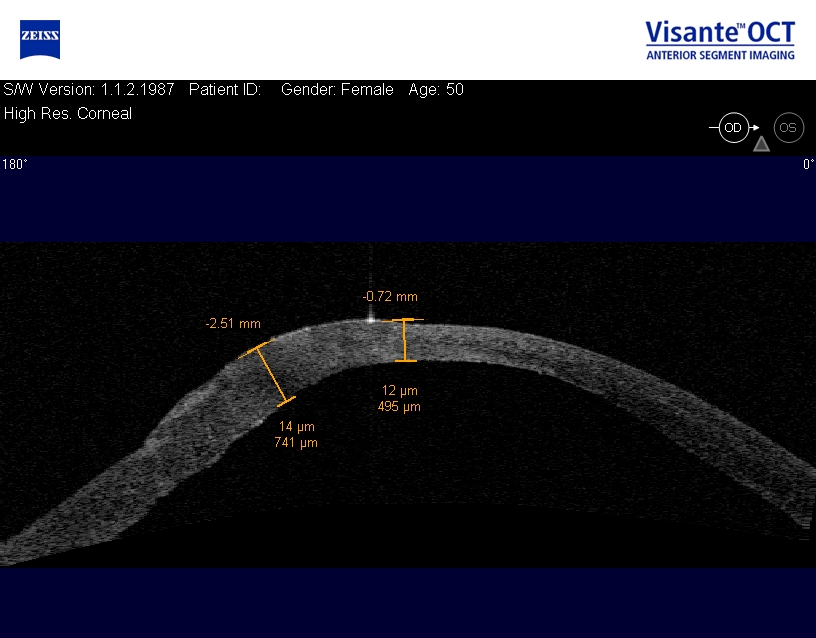 |
Corneal Descemetocele with Secondary Corneal Edema
|
There is no classification system in place for Descemetocele.
The following differential diagnoses can be considered when evaluating a Descemetocele:
- Corneal Melt, Postoperative
- Dermatitis, atopic
- Dry eye syndrome
- Episcleritis
- Giant cell arteritis
- Herpes simplex
- Herpes zoster
- HLA-B27 syndromes
- Keratitis
- Keratoconjunctivitis
- Keratopathy
- Ocular rosacea
- Pellucid marginal degeneration
- Peripheral ulcerative keratitis
- Scleritis
Available treatments of descemetoceles and corneal perforations range from temporary or short-term solutions to more definitive repair. The choice of treatment will depend on the underlying disease in addition to the size, extent of stromal involvement, location of the perforation and visual potential. Multiple treatments are often employed at the same time or in a staged process.
Medical Therapy
Lubrication
- Frequent lubrication, punctal occlusion and/or tarsorrhaphy can promote re-epithelialization in cases of aqueous deficient dry eye related corneal ulceration and impending corneal perforation
Antibiotics
- Topical and/or systemic antibiotics are often used for prophylaxis or therapeutically in cases of infections
Aqueous Suppressant
- Aqueous suppressant topical medications can reduce intraocular pressure, decrease outflow from the site of defect and encourage healing in cases where the anterior chamber is formed
Bandage Contact Lens
- Can promote corneal healing and re-epithelialization by protecting new epithelial cells from repeated disturbances from eyelid blinking and eye movements
- Useful in non-infectious impending or small corneal perforations or lacerations that have good apposition of edges and alignment, and no prolapse of uveal tissue
- Useful in peripheral defects or dry eye cases related to aqueous deficiency
- Soft, hydrophilic contact lenses can be kept in place for 4 to 7 days, however, they can be kept in place for longer periods of time if needed and used in conjunction with topical (preferably) and/or systemic antibiotics and topical aqueous suppressant medications
Anti-collagenase Medications
- Can be considered as an adjunctive treatment in cases of corneal ulceration (e.g., systemic tetracyclines)
- Systemic tetracyclines inhibit matrix metalloproteinases produced by neutrophils, epithelial gelatinases, α1-antitrypsin degradation and scavenge reactive oxygen species that can potentiate further collagen breakdown and retard corneal healing
Anti-inflammatory Medications
- Can be a useful adjunct for corneal ulcers with concomitant inflammation (e.g., topical steroids)
- Steroids may help dampen inflammation by blocking the entry of polymorphonuclear lymphocytes and prevent the accumulation of collagenases and ultimately promoting re-epithelialization and possibly improving final best-corrected visual acuity by reducing scarring
Vitamin C
- Vitamin C, topical and systemic, stimulate collagen production and can been used as an adjunct for the treatment of corneal ulceration
Immunosuppressive Agents
- May be helpful to control the underlying disease process in cases of progressive non-infectious corneal ulceration secondary to corneal inflammatory diseases
- Are often used in conjunction with systemic steroids and/or non-steroidal anti-inflammatory medications
Surgery
Suturing
- Direct suturing, using 10-0 monofilament nylon sutures, for small defects or lacerations in cases of trauma related corneal perforations
Corneal Gluing
- Corneal gluing with cyanoacrylate glue or fibrin glue can be considered for impending corneal perforations or frank corneal perforations that are small (< 3 mm), concave, and located away from the limbus
- Gluing is also a useful technique as a temporary measure for infectious perforations to allow for antimicrobial treatment prior to more definitive management with penetrating keratoplasty
- Cyanoacrylate glue has the advantage of being bacteriostatic and longer lasting than fibrin glue and it is also believed to inhibit polymorphonuclear lymphocytes and the production of collagenases, which may halt the corneal melting process
Amniotic Membrane Transplant
- Amniotic membrane transplant (AMT) in combination with fibrin glue or 10-0 polyglactin sutures can be used for impending or small frank corneal perforations (< 3 mm)
- AMT can be useful in cases of more peripherally located defects and is currently reserved for cases of refractory corneal ulceration or perforations that have failed medical treatment
Human placental amnion is composed of a single layer of epithelial cells, a basement membrane and a layer of avascular stroma. It has been found to have multiple growth factors including fibroblastic growth factor, hepatocyte growth factor and transforming growth factor β that may help promote tissue repair, remodeling, and epithelial healing and reduce inflammation, vascularization and scarring.
Multiple techniques have been described:
- Overlay AMT uses a single layer graft, 12 to 14 mm in diameter, and fashioned in place with 10-0 polyglactin sutures to cover the entire corneal, limbal and prelimbal surfaces
- Inlay AMT uses a single layer graft that is cut to size to fit the area of the defect and fashioned in place with 10-0 polyglactin sutures
- AMT fashioned in place with human fibrin glue
- Multilayer AMT technique fills the defect by stacking several small cut pieces of AMT prior to coverage with a larger piece of AMT and fashioned in place with 10-0 nylon sutures
- “Swiss roll” technique fills the defect by rolling a piece of AMT and fashioning it in place with 10-0 nylon sutures
Corneal Transplantation
- Corneal transplantation includes full thickness (penetrating) keratoplasty, corneal patch grafts and partial thickness (lamellar) keratoplasty
- Penetrating keratoplasty are reserved for large corneal perforations (> 3 mm) not amenable to other treatments, flat anterior chamber with iris prolapse, or failure of medical treatment or corneal gluing
- If cornea ulceration is due to infection, it is beneficial to delay penetrating keratoplasty until aggressive topical fortified antibiotics has been started 24 to 48 hours prior, however, this must be balanced with impending perforation with its risk of endophthalmitis or lateral extension with the risk of infectious scleritis
Temporizing measures including corneal glue or BCL should be considered until infection or inflammation can be controlled prior to performing a penetrating keratoplasty. Corneal patch grafts, either lamellar or full-thickness, can be used temporarily for central corneal perforations or permanently for peripheral corneal perforations or descemetoceles.
Conjunctival Flaps
- Partial or total conjunctival flaps are reserved for chronic, indolent ulcers that do not heal despite medical or surgical interventions
- Total conjunctival flaps such as the Gundersen flap are usually considered for eyes that have poor visual potential
Conjunctival flaps helps to promote healing, control pain and decrease the need for frequent medication. A thin flap of conjunctiva is freed up from the underlying tissues, avoiding Tenon’s capsule, pulled over the affected cornea and secured into place using sutures.
Conjunctival resection
- Can be considered for treating marginal corneal ulcerations secondary to autoimmune diseases such as those related to collagen vascular diseases or Mooren’s ulcer
- Approximately 3 mm of conjunctiva is excised posterior to the corneoscleral limbus and parallel to the ulcer
1. Cheung N, Sayegh R, Gupta P. Management of Descemetocele and Corneal Perforation. Eyewiki. http://eyewiki.aao.org/Management_of_Descemetocele_and_Corneal_Perforation. Last accessed January 4, 2015.
2. Sivakumar M, Tan D. Descemetocele following a simple avulsion procedure for pterygium. Br J Ophthalmol 1997;81:252 doi:10.1136/bjo.81.3.252c http://bjo.bmj.com/content/81/3/252.4.full. Last accessed January 6, 2015.
371.72
Descemetocele
92285
External ocular photography
92132
Anterior segment imaging
76513
Anterior segment ultrasound
76514
Corneal pachymetry
92025
Corneal topography
92286
Specular microscopy




 Print | Share
Print | Share