
Congenital optic pit with associated macular edema
ICD-10 Diagnosis Codes:
H47.391–Optic pit, right eye
H47.392–Optic pit, left eye
H47.393–Optic pit, bilateral
Title
Crater-like Holes of the Optic Disc
Category
Disorders Of The Optic Nerve And The Visual Pathways
Description
Optic pits are excavations of the optic nerve head.
| Optic nerve pits are developmental anomalies that result from an imperfect closure of the superior edge of the embryonic fissure.
|
 |
Structural Damage to the Eye
- Imperfect closure of embryonic fissure
- Congenital optic pit is formed
- Average optic pit is about 500 microns in size
- Over 60% are located on the temporal side of the optic disc
- Bilateral in 10-15% of patients
- Optic pit maculopathy is thought to occur when fluid moves from the optic pit into the retina: macular edema, macular schisis, serous macular detachment
Functional Damage to the Eye
- None
- Decreased vision
- Metamorphopsia
- Micropsia
- Visual field defects: arcuate scotoma, enlarged blind spot, central scotoma
The main goal of a diagnostic evaluation in a patient with congenital optic nerve pits is to accomplish the following:
- Determine if the optic pits are asymptomatic
- Determine if the optic pits are complicated by macular lesions
- Obtain baseline automated visual field testing
- Obtain baseline OCT scans
- Prescribe a treatment program
Patient History
Patients with congenital optic nerve pits may present with any of the the following symptoms:
- None
- Decreased vision
- Metamorphopsia
- Abnormal “blind spot”
- Relative afferent pupillary defect
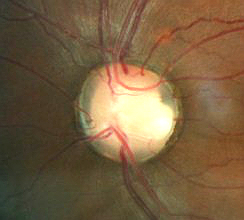
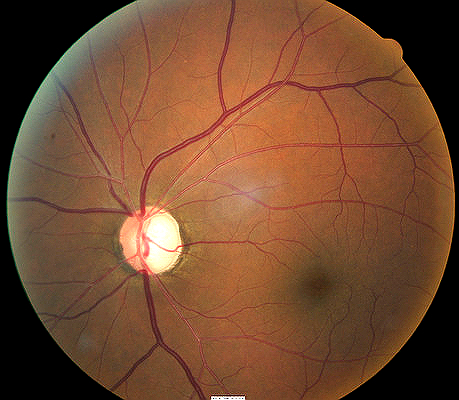
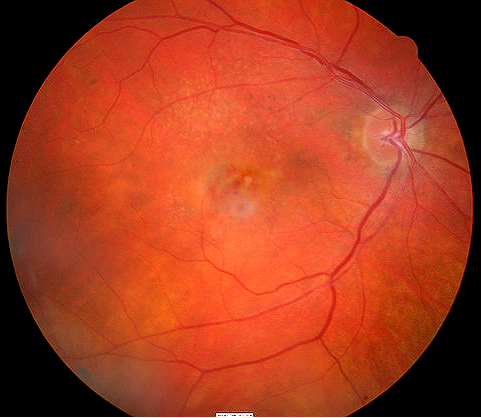
Ophthalmoscopy
- 27-year-old black male
- Bilateral congenital optic nerve pits
Optic pits along the optic disc rim are most likely to produce the following clinical abnormalities:
- Serous retinal detachments
- Full-thickness retinal holes
- Laminar retinal holes
- Retinal pigment epithelium mottling
- General cystic changes
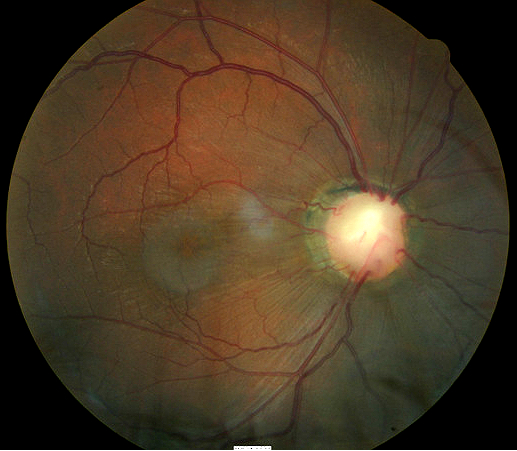 |
Clinical Appearance of the Retina
|
|
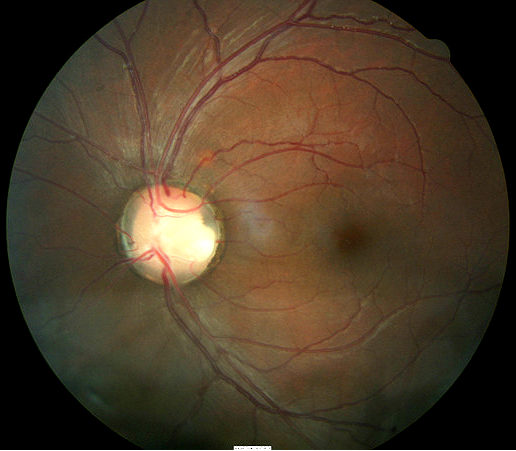 |
Clinical Appearance of the Retina
|
DIAGNOSTIC TESTS
Retinal Laser Scan — Optic Disc Cube
- Cirrus OCT by Carl Zeiss Meditec
- Retinal nerve fiber layer thickness
- Sector plot analysis
- TSNIT curve profile analysis
- Cup-to-disc ratio
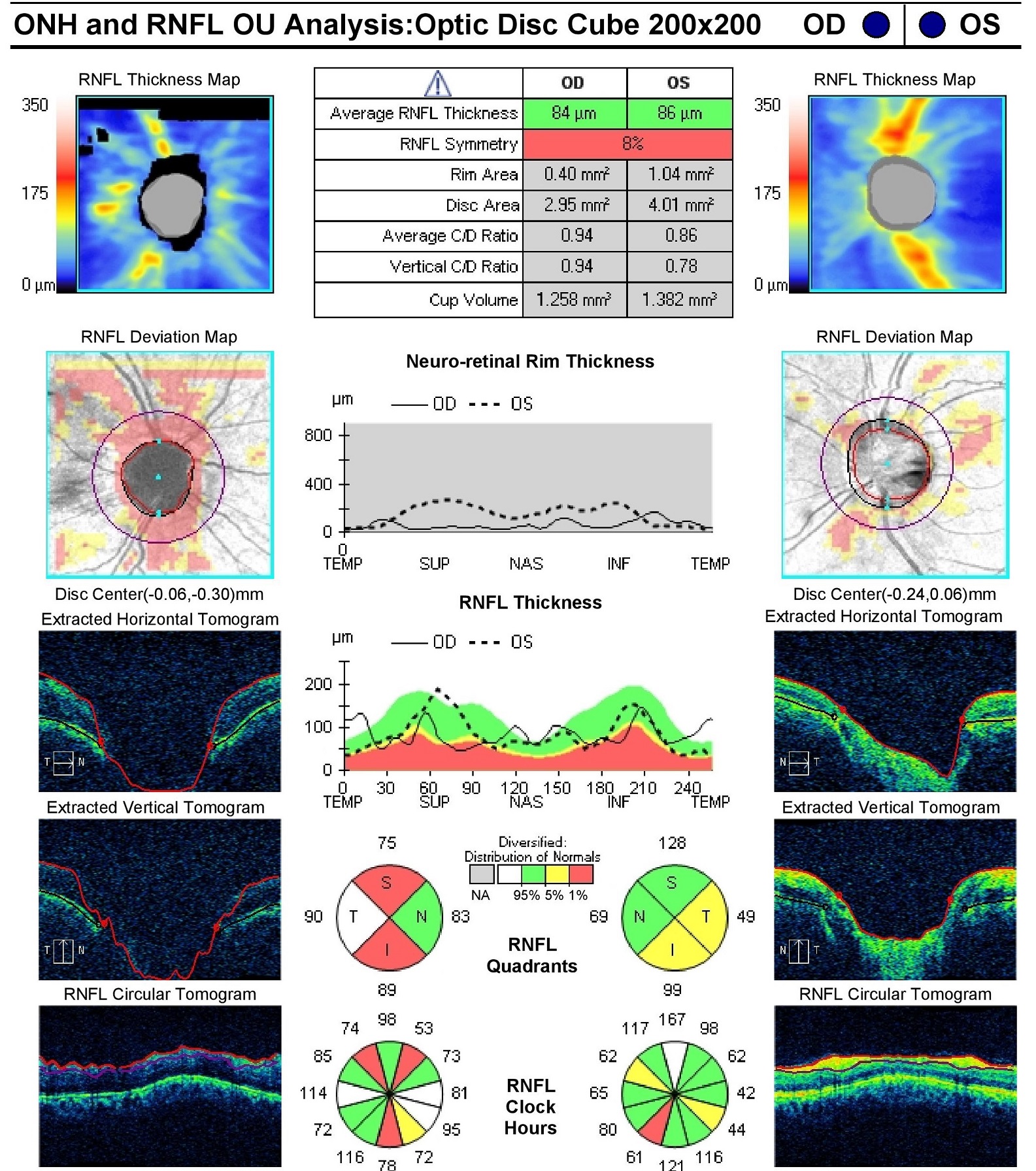 |
Optical Coherence Tomography
|
Retinal Laser Scan — Macular Cube
- Abnormal macular thickness — right eye
- Primary inner retinal layer schisis — right eye
- Neurosensory serous retinal detachment occurs secondary to the schisis; the retinal detachment is confined between the superior and inferior vascular arcade and is contiguous with the optic disc — right eye
- Normal macular thickness — left eye
- No vitreomacular traction syndrome; vitreomacular traction is an important factor in the development of optic pit-related serous macular detachment
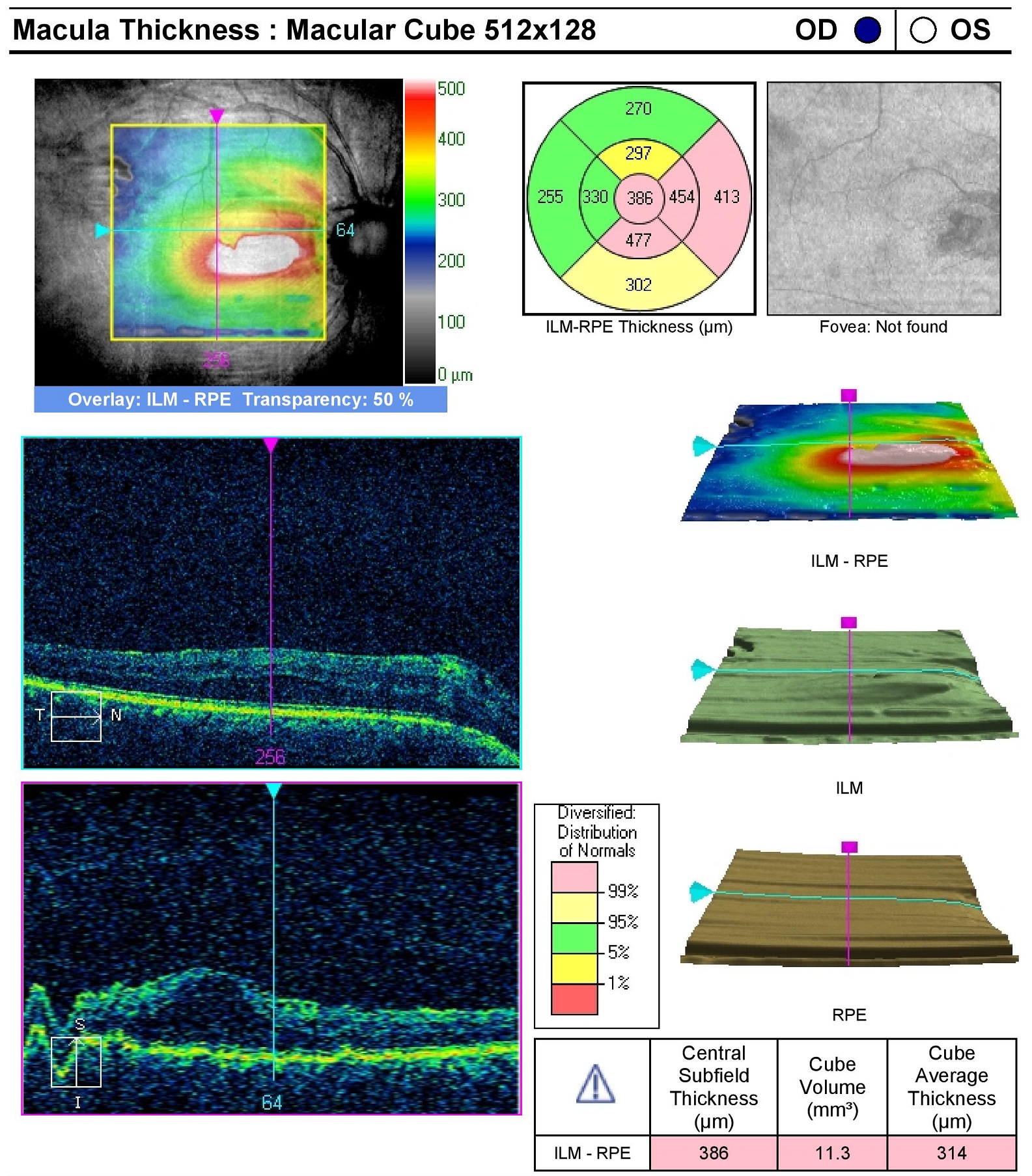 |
 |
Visual Field Examination
Optic pits produce visual field changes as the lesion displaces nreve fibers in the optic nerve head. There is usually no absolute central scotoma in optic pit-induced maculopathy.
- Enlarged blind spot — right eye
- Inferior nasal arcuate sotoma — right eye
- Superior nasal paracentral scotoma — right eye
- Superior temporal paracentral scotoma — left eye
 |
 |
Electrodiagnostic Testing
Electroretinogram (ERG) — When macular schisis and serous detachment are present, the ERG waveform may be poorly defined with reduced amplitudes.
- Preoperative evaluation of macular function is used to predict the degree of central vision recovery after macular reattachment surgery.
- Patients with a severely abnormal ERG have a lower likelihood of visual recovery after macular reattachment surgery.
Visual Evoked Potential (VEP) — When macular schisis and serous detachment are present, the VEP waveform may reveal delayed P100 peak times and wave shape perturbation.
 |
Visual Evoked Potential Testing
|
There is no classification system for congenital optic nerve pits.
The following disease share some of the clinical signs of optic nerve pits:
- Central serous retinopathy
- Glaucomatous optic neuropathy
- Subretinal neovascular membrane
- Tilted disc syndrome
- Circumpapillary staphyloma
- Hypoplastic optic disc
- Choroidal or scleral cresent
 |
Central Serous Retinopathy
|
|
Glaucomatous Optic Neuropathy
|
 |
|
 |
Subretinal Neovascular Membrane
|
The primary goal of treating a patient with congenital optic pit is to determine whether or not macular complications exist. If there are no macular complications, the best treatment option is observation with an annual surveillance examination.
Palliative Treatment
- Annual observation, if no macular complications exist
- Observation at 3-month intervals for spontaneous resolution of macular complications
- Up to 25% of optic pit-induced serous macular detachments will spontaneously re-attach
- Consider surgical treatment for macular complications if visual acuity is declining
An annual surveillance examination for optic pit-induced maculopathy may include the following service components:
- Dilated fundus examination
- Intraocular pressure
- Visual field examination
- OCT imaging of the maculas
- Electroretinogram
Maximum surveillance for optic pit-induced maculopathy is achieved with a patient-oriented monthly visual assessment program:
- Amsler grid to monitor for early metamorphopsia
- Home visual acuity measurement
Surgical Treatment
1. Laser photocoagulation — Used to produce laser burns between the area of serous retinal detachment and the optic disc.
- Most common surgical treatment for serous detachment of the macula
- Follow-up examination 3-4 weeks after treatment to evaluate the resorption of subretinal fluid
2. Macular buckling — Procedure converts vitromacular traction from an inward to an outward vector, promoting macular reattachment.
3. Vitreal surgery and internal tamponade — Combination of posterior vitrectomy, laser photocoagulation and gas tamponade used to promote macular reattachment in refractory cases.
1. Singh R. Scott I. Diagnosis and Management of Congenital Optic Pit. Oct 2006. http://www.aao.org/publications/eyenet/200610/pearls.cfm. Last accessed August 13, 2014.
2. RevOptom. Handbook of Ocular Disease Management. Optic PIt. http://www.reviewofoptometry.com/cmsdocuments/2013/7/hod0613i.pdf. Last accessed August 13, 2014.
377.22
Crater-like holes of optic disc
92015
Refraction
92250
Fundus photography
92083
Visual field examination
92283
Color vision examination
92275
Electroretinography
92225
Extended ophthalmoscopy
92134
Macula OCT scan




 Print | Share
Print | Share