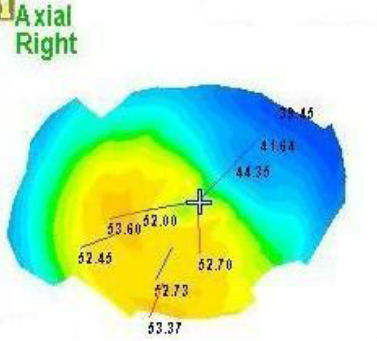
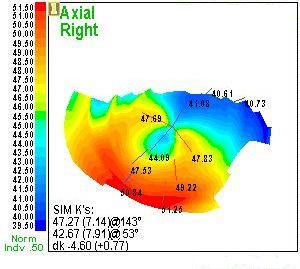
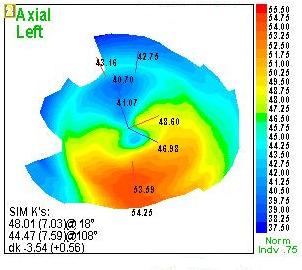
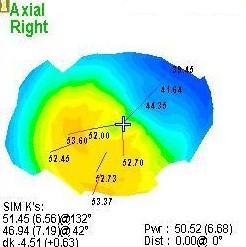
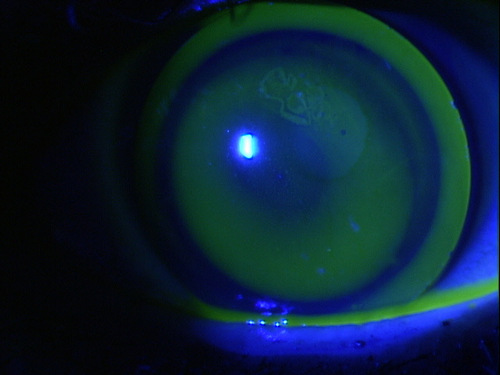
Corneal ectasia in advanced PMD is revealed on
corneal topography map
ICD-10 Diagnosis Codes:
H18.711–Corneal ectasia, right eye
H18.712–Corneal ectasia, left eye
H18.713–Corneal extasia, bilateral
Title
Pellucid Marginal Degeneration
Category
Corneal Opacity And Other Disorders Of Cornea
Description
Pellucid marginal degeneration is a condition characterized by peripheral corneal thinning and corneal ectasia.
Pellucid marginal degeneration (PMD) is a non-inflamatory thinning of the peripheral cornea. It is usually bilateral, but is often asymmetric. The area of corneal thinning is usually inferior and the distribution of the corneal degeneration is arcuate-shaped like a “crab’s claw” or “kissing dove” appearance.
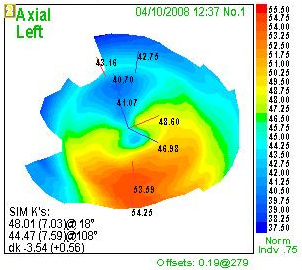 |
Corneal Topography Characteristics
|
Pellucid marginal degeneration is an idiopathic corneal disease that is not associated with any systemic conditions.
Structural Damage to the Eye
- Possible increase in mucopolysaccharides in the corneal stroma
- Thinning of the cornea in the peripheral region
- The area of thinning is usually 1-2 mm wide and 1-2 mm from the limbus
- Steepening of the cornea (corneal ectasia) usually occurs in the inferior region
- Corneal protrusion may occur just above the area of corneal thinning
- Breaks in the posterior cornea lead to severe stromal edema – although rare (acute corneal hydrops)
- Breaks in the anterior cornea lead to corneal perforation (very rare)
Functional Damage to the Eye
- Decreased vision
- Glare
- Halos around lights
- Monocular diplopia
- Ghost images
- Multiple unsatisfactory attempts in obtaining good visual acuity with eyeglasses or contact lenses
The main goal of the diagnostic evaluation in a patient with pellucid marginal degeneration is to accomplish the following:
1. Determine the correct diagnosis with corneal topography
- Corneal topography reveals an arcuate-shaped area of corneal ectasia
- Central corneal region measures normal thickness
- Inferior, peripheral corneal region reveals corneal thinning
2. Determine if the patient can function with eyeglasses
3. If necessary, prescribe contact lenses to improve visual function
4. In rare cases of significant progression, prescribe surgical treatment to improve visual function
Patient History
Patients with pellucid marginal degeneration may present with any of the following signs and symptoms:
- None
- Photophobia
- Halos around lights
- Monocular diplopia
- Variable and inconsistent refractions
- History of multiple spectacle prescriptions in a short period of time
- History of unsuccessful contact lens wear
- Complaints of distortion rather than blurred vision and both distance and near
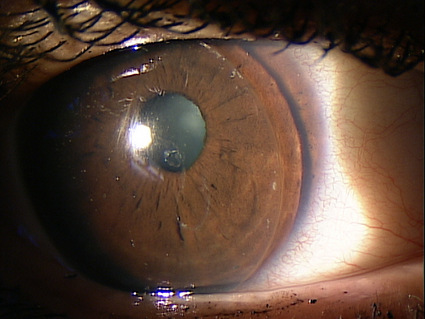
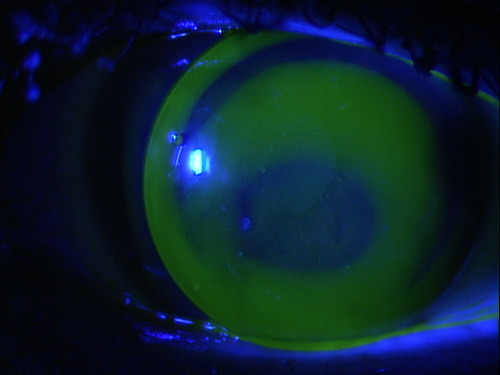
External Ocular Examination with Biomicroscopy
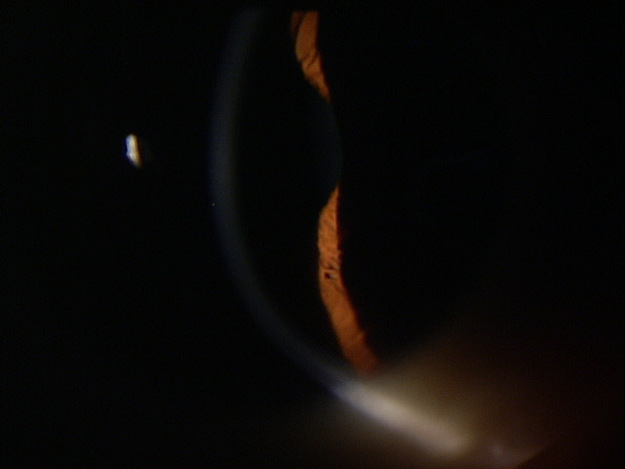 |
Clinical Appearance of the Cornea
|
DIAGNOSTIC TESTS
Computerized Corneal Topography
- Document the shape and physical features of the anterior corneal surface
- Identification and follow-up for pellucid marginal degeneration
- The distribution of the degeneration is arcuate or crescent-shaped
- Corneal thinning results in advanced against-the-rule astigmatism
 |
 |
Corneal Pachymetry
- Measurement of corneal thickness
- Pellucid marginal degeneration is suspected in any cornea where the peripheral corneal region is thinner than the central region
There is no classification system in place for pellucid marginal degeneration.
The main differential diagnosis with pellucid marginal degeneration lies in its similarity to keratoconus. The following table marks the major differences between the diseases.
| Clinical Feature | Keratoconus | Pellucid |
| Onset | Typically younger | Young to middle age |
| Progression | Likely | Variable |
| Effect on vision | Usually significant effect | Variable but milder effect |
| K steepening | Central to mid-peripheral | Peripheral steepening |
| K thinning | Over apex of cone | Peripheral thinning |
| Topographic distortion | Central to slightly inferior cone | Arcuate (kissing doves) |
Treatment with Eyeglasses
- Patients with mild pellucid marginal degeneration may obtain functional vision with eyeglasses
- As the disease progresses, patients may need frequent changes in their eyeglass prescriptions
Treatment with Contact Lenses
- Soft contact lenses
- Gas permeable lenses
- Hybrid lenses
- Scleral lenses
- Kerasoft IC contact lenses
- Piggyback lens system
 |
Pellucid Marginal Degeneration
|
|
 |
TruPMD Gas Permeable Contact Lens
|
|
 |
Intra-Limbal Gas Permeable Lenses
|
|
 |
Intra-Limbal Gas Permeable Lenses
|
1. Rasheed K. Pellucid marginal degeneration. July 2012. http://emedicine.medscape.com/article/1196382-overview. Last accessed March 30, 2014.
371.71
Corneal ectasia
92020
Computerized corneal topography
92285
External ocular photography
76514
Corneal pachymetry
92132
Anterior segment imaging
76513
Anterior segment ultrasound
Occurence
Incidence and prevalence of pellucid marginal degeneration is unknown.
Distribution
Some studies suggest men are slightly more affected than women.
Risk Factors
No casual relationships between other diseases and pellucid marginal degeneration have been established.




 Print | Share
Print | Share