H16.231–Neurotrophic keratoconjunctivitis, right eye
H16.233–Neurotrophic keratoconjunctivitis, bilateral
Title
Neurotrophic Keratoconjunctivitis
Category
Keratitis
Description
Neurotrophic keratoconjunctivitis is a degenerative disease of the corneal epithelium resulting from impaired corneal innervation.
Neurotrophic keratopathy is a degenerative disease characterized by decreased corneal sensitivity and poor corneal healing. This disorder leaves the cornea susceptible to injury and decreases reflex tearing. Epithelial breakdown can lead to ulceration, infection, melting, and perforation secondary to poor healing.
Prognostic indicators in neurotrophic keratopathy include the degree of sensory loss, the duration of the condition, and the presence of other ocular surface disease. The incidence of neurotrophic keratopathy increases with age.
The main goal of the diagnostic evaluation in a patient with neurotrophic keratoconjunctivitis is to accomplish the following:
- To establish the diagnosis of neurotrophic keratoconjunctivitis
- To establish appropriate therapy
- To relieve discomfort
- To prevent complications
- To educate patients and involve them in managing their disease
To obtain the information required to determine a clinical diagnosis of neurotrophic keratoconjunctivitis and to prescribe a treatment plan, the following service components of a medical eye examination should be performed.
- Patient history
- General medical observation
- Adnexal examination
- External ocular examination with biomicroscopy
Patient History
Patients with neurotrophic keratoconjunctivitis may present with any of the following abnormal clinical symptoms:
- Dry eyes
- Itchy eye
- Burning eyes
- Scratchy eyes
- Stinging eye
- Watery eyes
- Light sensitivity
- Gritty sensations
- Eye pain
- Blurred vision
Adnexal Examination
- The eyelids should be examined carefully for both diagnostic and prognostic information
- Eyelids that do not close properly may indicate a cranial nerve VII palsy
- Lagophthalmos leads to epithelial exposure and accelerates progression to stage 3 disease
External Ocular Examination with Biomicroscopy
Patients with neurotrophic keratoconjunctivitis may present with abnormal clinical signs in any of the following anatomical areas:
- Look for secondary damage like iris atrophy
- Look for signs of anterior chamber inflammatory reaction (e.g., cells, flare, synechia)
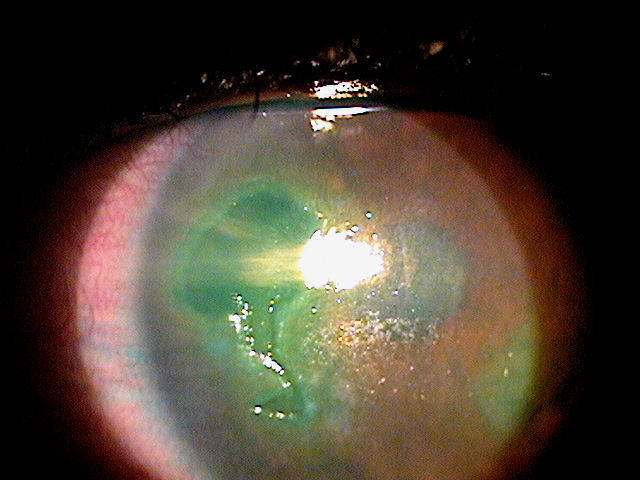
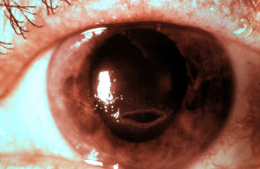
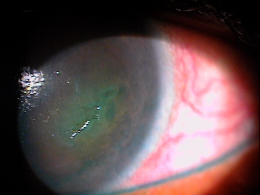
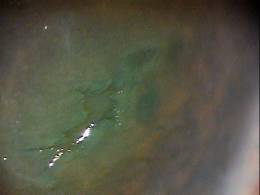
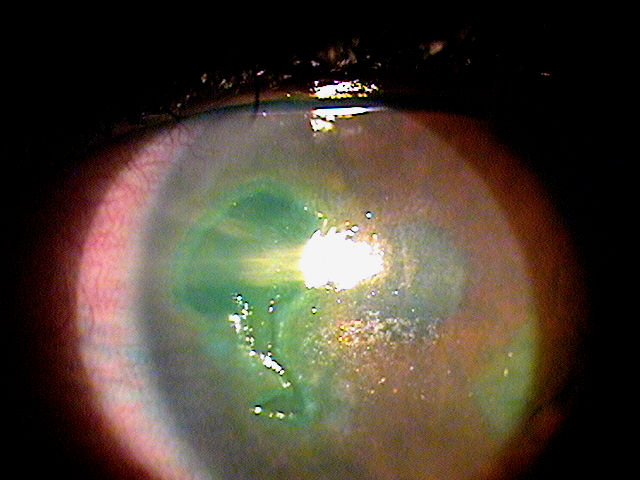
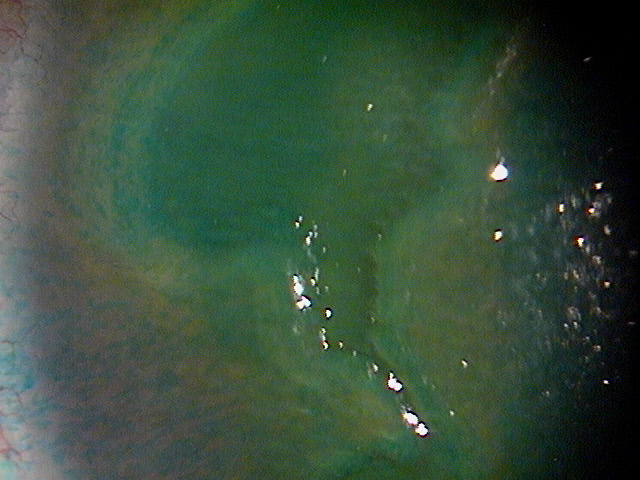
Neurotrophic keratopathy can be classified into three stages based on the Mackie classification:
Stage 1
- Rose bengal staining of the inferior palpebral conjunctiva
- Decreased tear breakup time
- Increased mucous viscosity
- Punctate epithelial fluorescein staining
- Vascularization
Stage 2
- Epithelial defect – usually oval and in the superior cornea
- Defect surrounded by a rim of loose epithelium
- Edges may become smooth and rolled
- Stromal swelling with folds in the Descemet membrane
- Sometimes associated with anterior chamber inflammatory action
Stage 3
- Stromal lysis/melting
- May result in perforation
Conditions to consider in the differential diagnosis of neurotrophic keratopathy include the following:
- Exposure keratopathy
- Limbal deficiency
- Topical anesthetic abuse
The following differential diagnoses could be considered:
- Corneal melt, postoperative
- Corneal mucous plaques
- Dry eye syndrome
- Herpes simplex
- Herpes zoster
- Keratitis, bacterial
- Keratitis, herpes simplex
- Keratoconjunctivitis, sicca
- Sjogren syndrome
Pharmocologic Treatment
No medications are available that can improve corneal sensitivity. The medications used in the treatment of neurotrophic keratopathy, including antibiotics, cycloplegics, and ophthalmic lubricants are adjunctive to surgical intervention. The number and types of medications vary according to the disease stage:
Stage 1
- Topical lubrication with preservative-free artificial tears, gels, and ointments
- Discontinuation of any topical ocular therapies, especially those that can decrease corneal sensitivity (eg, timolol, betaxolol, sulfacetamide, diclofenac, ketorolac) or that contain preservatives
- Reevaluation of the need for systemic drugs, such as neuroleptics, antipsychotics, and antihistamines
- Punctal occlusion may need to be considered
- Oral tetracycline (250 mg PO bid) or doxycycline (100 mg PO qod) can reduce the amount of mucus produced
- Weyns et al proposed scleral contact lenses as a valid long-term alternative to standard treatment options in patients with neurotrophic keratopathy
- Gaudilla et al note 20% autologous topical serum is an effective treatment for stages 1 and 2 neurotrophic keratopathy
Stage 2
- All of stage 1 treatments
- Topical tetracycline reportedly increases the healing of epithelial defects (not available in an ophthalmic drop preparation)
- Topical cycloplegia with atropine 1% or scopolamine 0.25% once daily in the presence of anterior chamber inflammation
- Patients with stage 2 disease are more likely to require surgical intervention than are those with stage 1 disorder
Stage 3
- All of stage 1 and stage 2 treatments
- Surgical intervention
Surgical Treatment
Surgical care may be necessary in stage 2 or 3. Such treatment has 3 goals:
- Protect the epithelium by lid closure
- Close a persistent epithelial defect
- Repair a deep ulceration
Closure of the eyelids
In the presence of severe or total loss of corneal sensation, keratitis sicca, or exposure keratopathy, a lateral tarsorrhaphy, palpebral spring, or botulinum A toxin injection in the levator muscle may prevent progression to stage 2.
Closure of a persistent epithelial defect
Repair options for such lesions include:
- Conjunctival flap — effective, but poor cosmetic and visual result
- Amniotic membrane transplantation
Repair of a deep ulceration
The following can be used in ulceration repair:
- Lamellar keratoplasty
- Penetrating keratoplasty — for large defects
- Multilayer amniotic membrane transplantation — has been used in defects as deep as 90% of the depth of the stroma
- Cyanoacrylate glue with a soft bandage contact lens — for defects smaller than 2 mm
Future Treatments
- Nerve growth factor — has been shown to induce healing of stage 3 keratopathy in an open, uncontrolled study
- Aldose reductase inhibitor, CT-112 — has been shown to reverse abnormal morphology of corneal epithelial cells and to increase corneal sensitivity
- Topical pindolol — has been reported to speed the healing of epithelial defects
1. Graham R. Neurotrophic Keratopathy. Medscape/EMedicine. 2 Sept 2014. http://emedicine.medscape.com/article/1194889-overview#showall. Last accessed January 25, 2015.
2. Wells J, Michelson M. Diagnosing and Treating Neurotrophic Keratopathy. American Academy of Ophthalmology. http://www.aao.org/publications/eyenet/200807/pearls.cfm. Last accessed January 25, 2015.
370.35
Neurotrophic keratoconjunctivitis
92285
External ocular photography
92132
Anterior segment imaging
92071
Bandage contact lens
68761
Punctal occlusion
92025
Corneal topography
65778
Amniotic membrane placement
Occurrence
The causes of neurotrophic keratopathy are conditions that decrease corneal sensitivity. The most common of these are herpetic infections of the cornea, surgery for trigeminal neuralgia, and surgery for acoustic neuroma.
- There are 40,000-60,000 cases of herpes zoster ophthalmicus occurring each year in the United States
- 50% have ocular involvement
- Of these, 16% demonstrate some form of neurotrophic keratopathy
Distribution
- Neurotrophic keratopathy is distributed evenly among patients with known risk factors
Risk Factors
Herpetic Infections of the Cornea
- Herpes simplex
- Herpes zoster
- Leprosy
Fifth-nerve Palsy
- Surgery for trigeminal neuralgia
- Neoplasia (acoustic neuroma)
- Aneurysms
- Facial trauma
- Congenital
- Familial dysautonomia (Riley-Day syndrome)
- Goldenhar-Gorlin syndrome
- Möbius syndrome
- Familial corneal hypesthesia
Topical Medications
- Anesthetics
- Timolol
- Betaxolol
- Sulfacetamide
- Diclofenac sodium
- Ketorolac
Corneal Dystrophies
- Lattice
- Granular
Systemic Diseases
- Diabetes mellitus
- Vitamin A deficiency
- Multiple sclerosis
Iatrogenic
- Contact lens wear
- Trauma to ciliary nerves by laser treatment and surgery
- Corneal incisions
- Laser in situ keratomileusis (LASIK)
Toxic
- Chemical burns
- Carbon disulfide exposure
- Hydrogen sulfide exposure
Miscellaneous
- Increasing age
- Dark eye color
- Adie syndrome




 Print | Share
Print | Share