ICD-10 Diagnosis Codes:
H16.211–Exposure keratoconjunctivitis, right eye
H16.212–Exposure keratoconjunctivitis, left eye
H16.213–Exposure keratoconjunctivitis, bilateral
Title
Exposure Keratoconjunctivitis
Category
Keratitis
Description
Exposue keratoconjunctivitis occurs when the surface of the conjunctiva or the cornea become dehydrated and damaged secondary to poor tear film wetting.
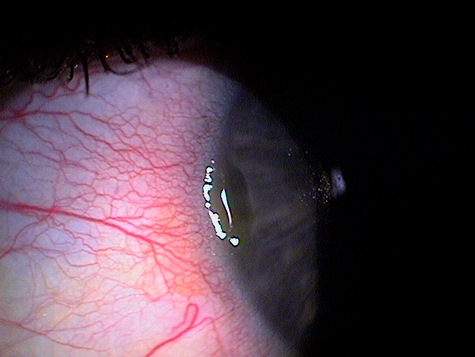
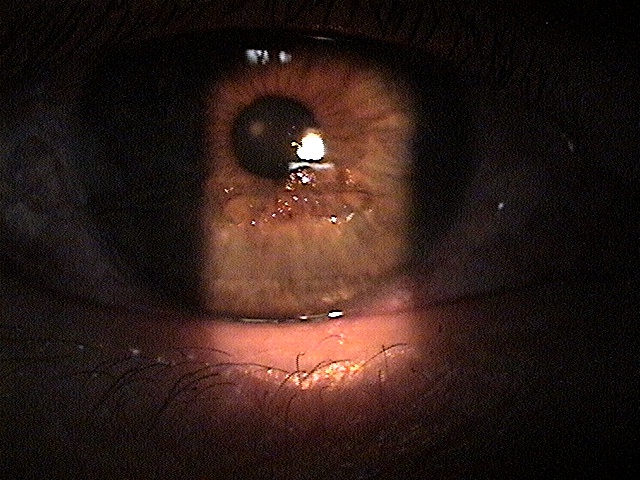
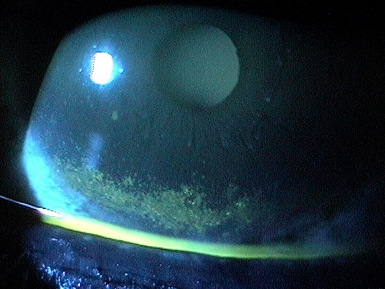
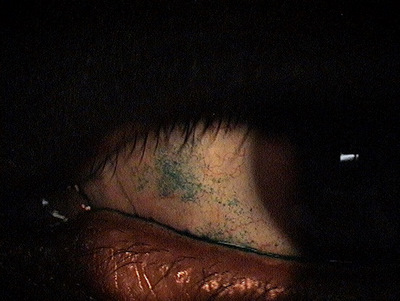
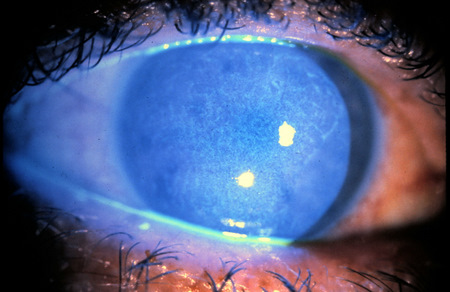
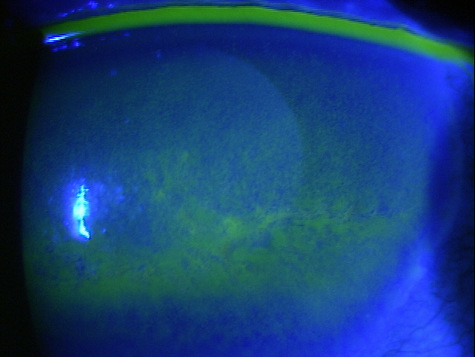
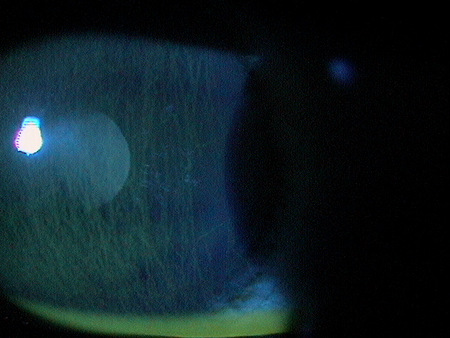
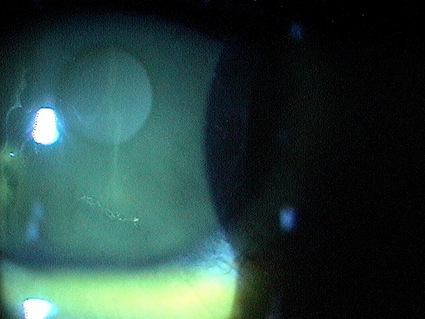
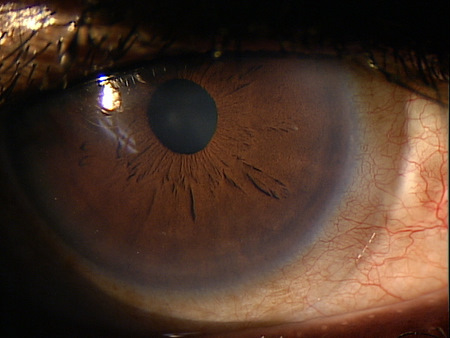
Exposure keratoconjunctivitis is an inflammatory disease of the cornea and conjunctiva caused by inadequate wetting of the ocular surface. Abnormal clinical findings include the following:
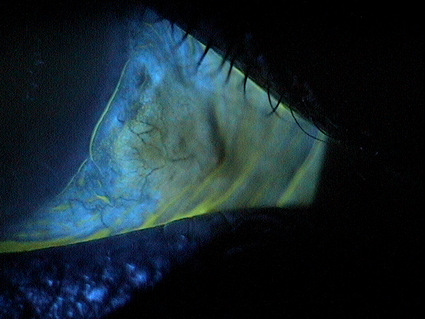
- Conjunctival epitheliopathy
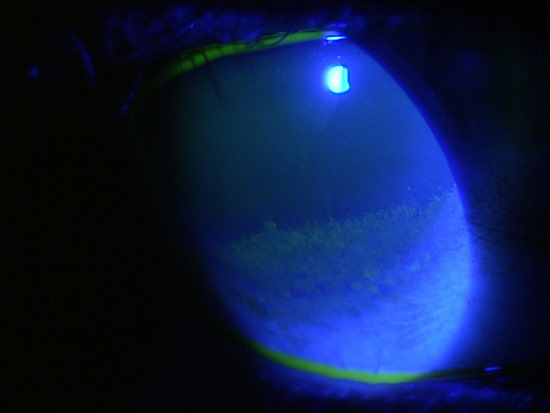
- Corneal epitheliopathy (punctate erosions)
- Conjunctival redness
- Corneal delle formation
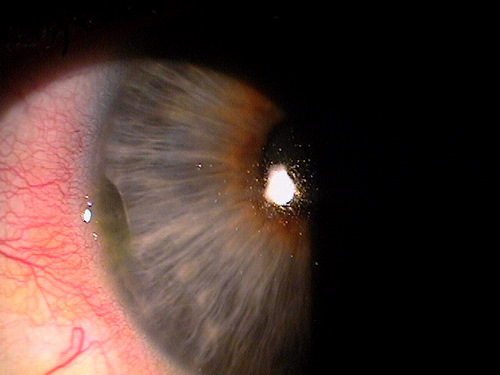
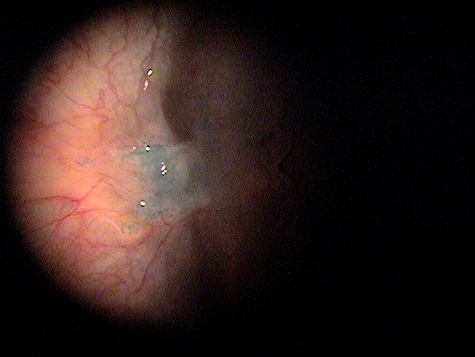
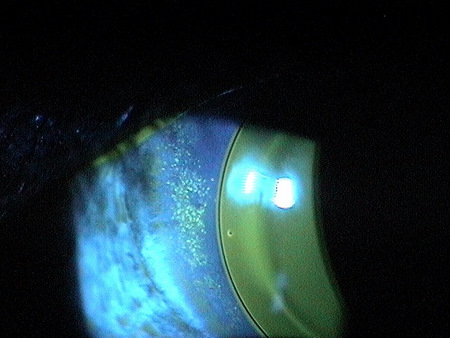
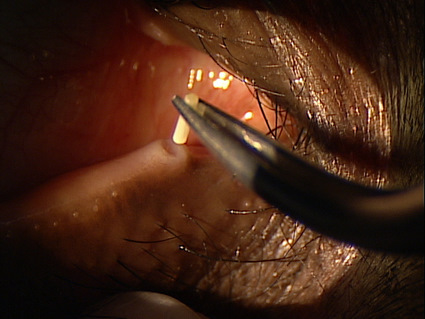
A corneal delle is a form of exposure keratoconjunctivitis. It represents an area of localized corneal thinning that usually appears as a small depression in the corneal periphery. The natural history of corneal delle formation is characterized by the following clinical events:
- Delle is produced when the corneal stroma loses an excessive amount of water
- Loss of water leads to stromal dehydration and reduced stromal thickness
- Loss of water is caused by improper wetting of the corneal surface by the tear film
- Poor wetting is usually caused by an elevated mass on the conjunctiva directly adjacent to the limbus
- The elevated mass prevents the eyelid from wetting the corneal surface with the blink
Structural Damage to the Eye
- Corneal thinning
- Corneal warping
- Epithelial abnormalities
- Conjunctival abnormalities
Functional Damage to the Eye
- Blurred vision
- Tear film insufficiency
- Eye pain
- Sensitivity to light
The main goal of the diagnostic evaluation in a patient with exposure keratoconjunctivitis is to accomplish the following:
- To establish the diagnosis of exposure keratoconjunctivitis
- To determine WHY there is poor wetting of the ocular surface
- To establish appropriate therapy
- To relieve discomfort
- To prevent complications
- To educate patients and involve them in managing their dry eye disease
To obtain the information required to determine a clinical diagnosis of exposure keratoconjunctivitis and to prescribe a treatment plan, the following service components of a medical eye examination should be performed:
- Patient history
- General medical observation
- Adnexal examination
- External ocular examination with biomicroscopy
Patient History
Patients with exposure keratoconjunctivitis may present with any of the following abnormal clinical symptoms:
- Dry eyes
- Itchy eye
- Burning eyes
- Scratchy eyes
- Stinging eye
- Watery eyes
- Light sensitivity
- Gritty sensations
- Eye pain
- Blurred vision
In addition to physiological conditions, symptoms can be worsened by exposure to environmental conditions such as wind, air conditioning, and temperature extremes. Activities that reduce blink rate (e.g., extended periods of reading, computer viewing, or driving) can produce more severe symptoms.
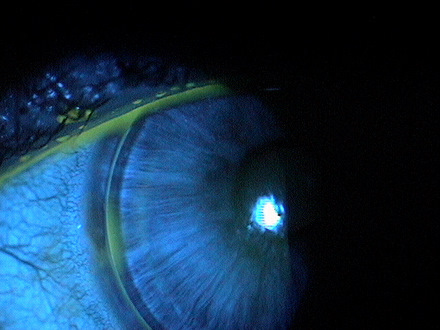
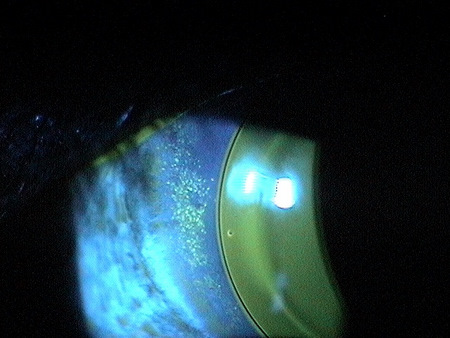
External Ocular Examination with Biomicroscopy
Patients with exposure keratoconjunctivitis may present with abnormal clinical signs in any of the following anatomical areas:
- Tear film
- Eyelid
- Conjunctiva
- Cornea
There is no classification system for exposure keratoconjunctivitis.
This would include other diseases that present with a superficial punctate keratopathy or conjunctival epitheliopathy.
To begin the treatment of exposure keratoconjunctivitis, the eye doctor must firmly establish the underlying etiology. In most cases, primary treatment of the resultant corneal condition is either supportive (moisturize) or prophylactic (antibiosis). But in most cases, unless the underlying causative factor is addressed, the condition tends to become chronic and more severe. Increased wetting of the cornea can be accomplished by prescribing artificial tears, lubricating ointments, or punctal occlusion.
Protection of the irritated cornea can be accomplished with a standard bandage contact lens or application of an amnionic membrane insert. Depending of the severity of corneal compromise, prophylactic antibiosis can be considered. Keratotoxic preparations should be avoided, especially aminoglycosides. Erythromycin or polysporin drops or ointment are excellent choices. To assist corneal healing, especially if waiting on a more permanent solution to the underlying eyelid pathology, taping the eyelids shut at night can be considered. Taping is rarely a definitive therapy and should be considered only for short-term treatment.
1. Bowling EL. Vital stains in cornea and contact lens practice. Review of Cornea and Contact Lenses. 2005 Jan/Feb: 25-28.
2. Silbert JA. Is it an ulcer or an infiltrate? RevOptom. 2007 June 15; (6): 91-101.
3. Edwards K, Brian G, Stretton S, Stapleton F, Willcox MD, Sankaridurg PR, Sweeney DF, Holden BA. Microbial Keratitis and Silicone Hydrogel Lenses. Contact Lens Spectrum. 2004 Jan: 38-42.
4. Snyder C. Solution Interaction with the Ocular Surface: The Significance in Making the Grade. Clinical & Refractive Optometry. 2005; 16(5): 134-140.
5. Raizman M. Maintaining Corneal Barrier Integrity. 2007 Oct 15; (10): 5-6.
6. Karpecki PM. Much Ado About Staining. RevOptom. 2006 Nov 15; (11): 135-136.
Exposure keratoconjunctivitis
92285
External ocular photography
92132
Anterior segment imaging
92071
Bandage contact lens
68761
Punctal occlusion
92025
Corneal topography
65778
Amniotic membrane placement
Risk Factors
- Contact lens wear
- Conjunctival degererations
- Allergic conjunctivitis
- Eyelid position disorders
- Glaucoma filtration surgery




 Print | Share
Print | Share