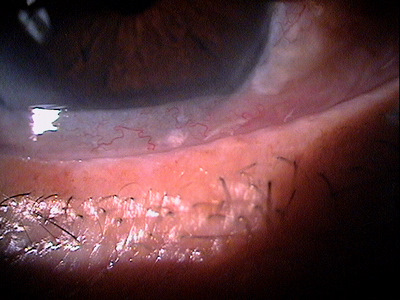
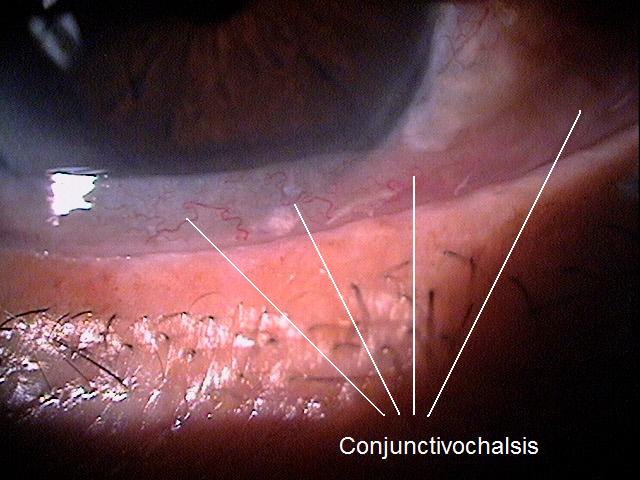
Conjunctivochalasis along the lower eyelid margin
ICD-10 Diagnosis Codes:
H11.821–Conjunctivochalasis, right eye
H11.822–Conjunctivochalasis, left eye
H11.823–Conjunctivochalasis, bilateral
Title
Conjunctivochalasis
Category
Disorders Of The Conjunctiva
Description
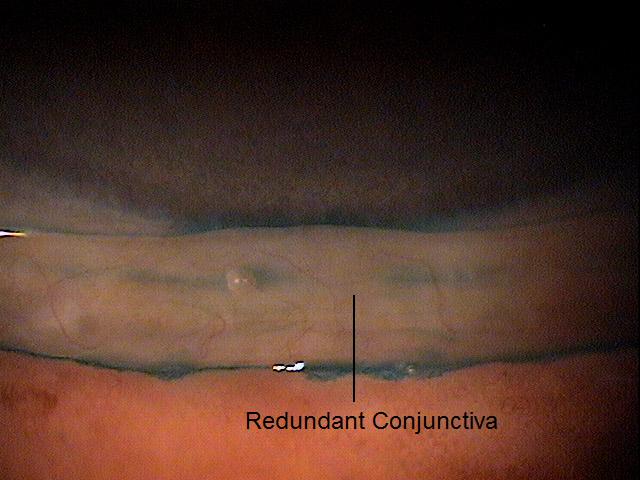
Conjunctivochalasis is a condition characterized by redundant or loose conjunctiva between the globe and eyelid.
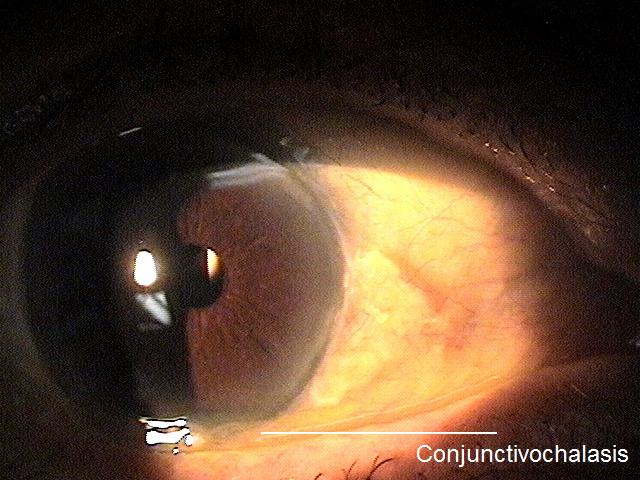
Conjunctivochalasis is a condition characterized by redundant or loose conjunctiva between the globe and eyelid and it can produce ocular surface irritation. The most common location for conjunctivochalasis is on the bulbar conjunctiva along the lower eyelid margin; however, it can affect any region on the surface of the eye.
The histopathological changes that contribute to the development of conjunctivochalasis are usually associated with advancing age.
 |
Lymphatic Flow Obstruction
Inflammation
|
Structural Damage to the Eye
- Damage to the eye is related to the effects of the conjunctivochalasis on the ocular surface
- Many patients complain of chronic epiphora because the redundant conjunctiva may occlude the lower punctum and reduces tear drainage
- The reduction in tear clearance causes a pooling of inflammatory mediators which results in ocular surface inflammation and irritation
- The excess conjunctival tissue can cause exposure related problems such as punctate keratitis, lagopthalmos or a corneal delle
- The constant movement of the abnormal vasculature in the redundant tissue can cause an avulsion of the blood vessels that results in recurrent subconjunctival hemorrhages
Functional Damage to the Eye
- Reduced visual acuity or blurred vision can occur secondary to chronic epiphora or exposure keratoconjunctivitis
The main goal in the diagnostic evaluation of a patient with conjunctivochalasis is to accomplish the following:
- Determine if the conjunctivochalasis is related to any other condition
- Evaluate any associated ocular surface disease
- Identify and exclude differential diagnoses
- Relieve ocular pain and discomfort
- Prescribe a treatment program
To obtain the information required to determine a clinical diagnosis of conjunctivochalasis and to prescribe a treatment plan, the following service components of a medical eye examination should be performed.
- Patient history
- General medical observation
- Adnexal examination
- External ocular examination with biomicroscopy
Patient History
Patient with conjunctivochalasis may present with any of the following abnormal clincal signs and symptoms.
- None
- Localized eye pain
- Foreign body sensation
- Chornic epiphora
- Burning
- Redness
- Itching
- Photophobia
- Excess mucous accumulation
- Problems with blinking
- Eyelid stickiness after sleep
- Tired eyes during reading or prolonged use of the eye
Clinical Appearance of the Conjunctiva
 |
Conjunctivochalasis
|
|
Clinical Appearance of the Conjunctiva
|
No specific classification exists for conjunctivochalasis. In a general sense, conjunctivochalasis may be classified as Mild, Moderate, or Severe.
 |
Mild Conjunctivochalasis
|
Dry eye syndrome
Although the symptoms are similiar, there are clinical differences between the two conditions. A patient with dry eye syndrome has dryness symptoms that are worse in the evening and in upgaze, unlike conjunctivochalasis patients have symptoms of dryness in downgaze. In addition, a dry eye patient’s symptoms may improve with blinking and punctal occlusion. Clinically they will have a normal to delayed tear clearance as well as fluorescein staining will show a low tear meniscus without interruption. There is also an exposure zone where the tissue shows dessication and will stain with rose bengal. Another difference is subconjunctival hemorrhages are infrequent in dry eye syndrome.
Blepharitis
Conjuctivolchalasis may also have similiar symptoms to blepharitis, but there are distinctive clinical differences. Patients with conjunctivochalasis can have dryness symptoms that are the same throughout the day and only get worse in downgaze, vigorous blinking or with punctal occlusion. Patients with conjunctivolchalasis will have frequent delayed tear clerance and fluorescein staining will show a tear meniscus interrupton or obliteration because of the redundant folds. On the eyelid margin, there may be an anterior migration of the mucocutaneous junction that stains with fluorescein, making it appear like conjunctivochalasis.
Conjunctivitis
Patients with conjunctivochalasis may present with conjunctival injection found in conjunctivitis. Another way to differentiate the two involves using lissamine green dye. Patients with conjunctivochalasis will have punctate staining on the bulbar conjuctiva adjacent to the region continuous with the stained eyelid margin.
The goal of treatment involves medications that reduce ocular surface inflammation and conjunctival edema. The intensity of the treatment depends on the severity of the condition and the patient should be educated on the potential need for long-term treatment and/or recurrent therapy.
Pharmacologic Treatment
- Non-preservative artificial tears to lubricate the eye and relieve ocular discomfort
- Topical steroids to inhibit the inflammatory response and reduce conjunctival edema
- Topical anti-histamines to reduce conjunctival edema
- Topical decongestants to reduce fluid volume in the tissue
Mechanical Treatment
- Patch the eye before bed time to reduce exposure keratopathy
Surgical Treatment
Consider surgical options if pharmacological and mechanical treatments do not provide any relief of symptoms.
- Conjunctival resection
- Superficial conjunctival cauterization
- Sutureless amniotic membrane transplantation with Tenon replacement
- Reconstruction with cryopreserved amniotic membrane
1. Thomas J. Is conjunctivochalasis on your dry eye radar? Ophthalmology Management. 2013 Sept; 17(9): 16-21.
372.81
Conjunctivochalasis
92285
External ocular photography
Occurence
The prevalence of conjuctivalchalasis is almost 90% of the population over 50 years old.
Distribution
Conjunctivalchalasis is not distrubuted evenly throughout the population. Its distribution increases dramatically with age and affects females more than males.
Risk Factors
- Advancing age
- Dry eye syndrome
- Allergic conjunctivitis
- Thyroid related ocular surace disease
- History of episcleritis
- History of prior ocular surgery
- History of conjunctival chemosis




 Print | Share
Print | Share