
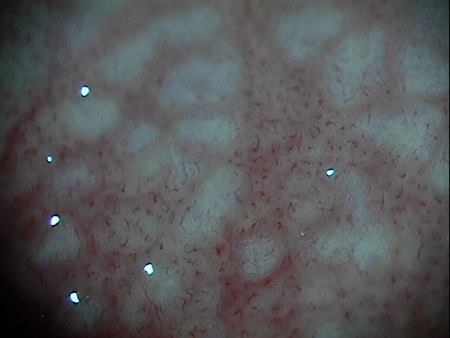
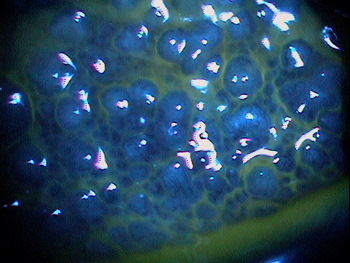
Giant papillae visible on upper eyelid eversion
ICD-10 Diagnosis Codes:
H10.411–Chronic giant papillary conjunctivitis, right eye
H10.412–Chronic giant papillary conjunctivitis, left eye
H10.413–Chronic giant papillary conjunctivitis, bilateral
Title
Giant Papillary Conjunctivitis
Category
Disorders Of The Conjunctiva
Description
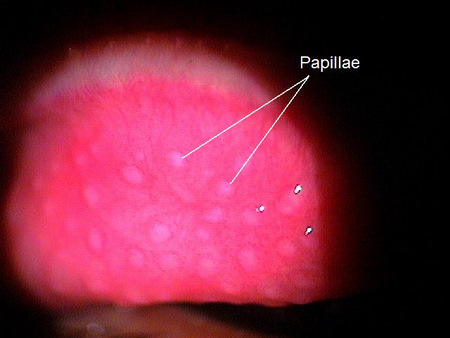
Giant papillary conjunctivitis (GPC) is a form of chronic conjunctivitis that is characterized by giant papillae on the superior tarsal conjunctiva.
Giant papillary conjunctivitis (GPC) is a form of chronic conjunctivitis that can be seen in patients with the following conditions:
- Patients who wear contact lenses
- Patients with exposed sutures after intraocular surgery
- Patients with a prosthetic eye
- Patients with hay fever or animal allergies
Giant papillary conjunctivitis is a result of the body’s over reaction to immunogen or allergen and is usually innate or acquired after multiple exposures to an antigen, however it has no seasonal variations.
 |
Papillary Hypertrophy of the Palpebral Conjunctiva
|
More recently, GPC is being seen in patients wearing silicone-hydrogel (SiHi) lenses. SiHi lenses can have a higher predisposition to deposit formation creating a roughened surface on the contact lens. The resultant GPC is considered more of a mechanical response to the frictional contact lens surface.
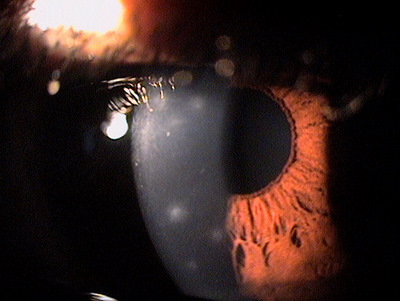
Structural Damage to the Eye
- Structural damage to the eye occurs from mechanical irritation of the tarsal conjunctiva of the upper lids resulting in histological changes in the tissue such as mast cell degranulation and the secondary inflammatory cascade
- There will also be an inflammation of the vasculature and superior lid hypertrophy
- Last, repetitive mechanical irritation can result in corneal abrasions with infiltrates
Functional Damage to the Eye
Giant papillary conjunctivitis can cause decreased vision as result of excessive lens deposits on the lens from the inflammatory response. Also, decreased vision can occur from displacement of the lens with blinking because of the superior lid hypertrophy.
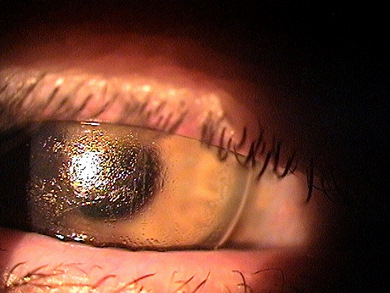 |
Contact Lens-Induced Giant Papillary Conjunctivitis
|
The main goal of the diagnostic evaluation in a patient with giant papillary conjunctivitis is to accomplish the following:
- Determine the underlying etiology of the giant papillary conjunctivitis
- Relieve ocular pain and discomfort
- Explain the condition to the patient
- Prescribe a treatment plan to treat the underlying condition
- Attempt to make changes that will lessen or prevent recurrence of the condition
Patient History
Patients with giant papillary conjunctivitis will present with the following signs and symptoms:
- Blurred vision
- Episodic tearing
- Blepharospasm
- Photophobia
- Conjunctival injection
- Mild foreign body sensation to severe pain
- Ocular itching that worsens with contact lens removal
- Increase mucous discharge in the tears especially in the morning
Contact lens intolerance characterized by any of the following clinical findings:
- Decreased wear time
- Increased lens awareness
- Excessive contact lens coating
- Excessive upward lens movement (typically, although can be random movement)
Clinical Appearance of the Conjunctiva
- Look for conjunctival injection
- Perform upper eyelid eversion
 |
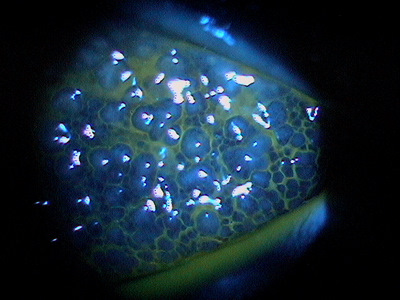
Giant Papillary Conjunctivitis
|
Clinical Appearance of the Tear Film
- Mucus strands can be seen in the tears in mild cases
- Mucus can be seen between the papillae in moderate-to-severe cases
- Papillae can be small uniform cobblestone lesions to irregular clusters of giant lesions with whitish centers that can ulcerate and stain with fluorescein
 |
 |
 |
DIAGNOSTIC TESTS
External Ocular Photography
- Document the progression or lack of progression of giant papillary conjunctivitis
- To help plan a treatment program
- Document the delivery and response to medical treatment
There is no official classification system for giant papillary conjunctivitis. It is often described based upon severity of the condition with mild, moderate, or severe descriptors. The severity of the condition determines the aggressiveness of the treatment.
This would include any other disease that presents with papillary response and/or ptosis.
Allergic Conjunctivitis
Patients with allergic conjunctivitis will present with symptoms of redness, watery eyes, mild discharge and the hallmark symptom of itchy eyes and conjunctival injection. Patients with allergic conjunctivitis usually do not describe a foreign body sensation like patients with giant papillary conjunctivitis do.
 |
Allergic Conjunctivitis
|
Vernal Conjunctivitis
The symptoms of discomfort or eye pain, redness, photophobia, foreign body sensation. The clinical signs are some what different and the case history is very important.
 |
Vernal Conjunctivitis
|
Viral Keratoconjunctivitis
The symptoms of discomfort or eye pain, redness, photophobia, foreign body sensation are the same except viral conjunctivitis patients also have watery eyes and the palpebral conjunctival redness is more of a diffuse pinkish color.
 |
Viral Keratoconjunctivitis
|
Congenital Ptosis
Giant papillary conjunctivitis can cause a ptosis that may be mistaken for a patient who has a congenital ptosis. In these cases ask the patient whether their eyelid has always looked droopy or smaller most of their life.
Treatment is based on the severity of the giant papillary conjunctivitis. The severity of the condition determines the aggressiveness of the treatment. In addition, the patient should be educated on the potential need for long-term treatment and/or recurrent therapy.
Pharmacological Treatment
Mild giant papillary conjunctivitis – Topical mast cell stabilizer
- Alocril b.i.d
- Alamast q.i.d
- Alomide q.i.d
- Crolom q.i.d
Moderate giant papillary conjunctivitis – Topical anti-histamine/mast cell stabilizer and NSAID
- Pataday q.d
- Patanol b.i.d
- Bepreve b.i.d.
- FML 0.1% t.i.d.
- Lotemax Gel t.i.d.
Severe giant papillary conjunctivitis – Topical anti-inflammatory and anti-histamine/mast cell stabilizer
- Pred forte t.i.d.
Mechanical Treatment
Discontinue contact lens wear and change contact lens treatment options:
- Change to daily wear disposables
- Decrease wearing time
- Change from soft contact lenses to gas permeable contact lenses
- If the patient is wearing a SiHi lens, change to hydrogel material with hydrogen peroxide disinfection and digital cleaning
- Prescribe bandage contact lens to cover exposed sutures after intraocular surgery
- Increase the frequency of cleaning a prosthetic eye
In all cases of giant papillary conjunctivitis, resolution of the disease can be highly variable. Giant papillary conjunctivitis from contact lens wear (especially extended wear lenses or when poor compliance is involved) may take several months of aggressive treatment to resolve. Resolution of giant papillary conjunctivitis induced by SiHi lenses can be fairly rapid, often as little as a week or two.
Surgical Treatment
- Remove exposed sutures
1. Brujic M. Kading D. Allergies and contact lens wear: finding the successful balance. Contact Lens Spectrum. 2013 March: 27-31
372.11
Simple chronic conjunctivitis
92285
External ocular photography
Occurrence
- The prevalence of GPC is 20% among patients who wear hydrogel contact lenses
- The prevalence of GPC is 5% among rigid gas permeable wearers
Distribution
- Giant papillary conjunctivitis is distributed evenly throughout the population
Risk Factors
- Children wearing contact lenses develop GPC more aggressively




 Print | Share
Print | Share