Acute primary canaliculitis with eyelid malposition
ICD-10 Diagnosis Codes:
H04.331–Acute lacrimal canaliculitis
of the right lacrimal passage
H04.332–Acute lacrimal canaliculitis
of the left lacrimal passage
H04.333–Acute lacrimal canaliculitis
of both lacrimal passages
Title
Acute Lacrimal Canaliculitis
Category
Disorders Of The Lacrimal System
Description
Canaliculitis is an inflammation of the lacrimal canaliculus secondary to infection or obstruction.
Primary lacrimal canaliculitis is an inflammation of the lacrimal canaliculi caused by infection from some type of microorganism. The most common causative organisms are the Actinomyces species, but recent studies indicate high rates of infection with streptococcal and staphyloccal bacteria.
The following microorganism prevalence was determined after a review of the literature on canaliculitis.
- Actinomyces – 30%
- No microorganism found – 21%
- Steptococcal bacteria – 12%
- Staphylococcal bacteria – 10%
- Fungus – 5%
- Nonspecific gram negative bacteria – 7%
- Nonspecific gram positive bacteria – 1%
- Other microorganism – 14%
Secondary lacrimal canaliculitis is most commonly associated with a punctal occlusion procedure using collagen or silicone plug implants. While the implants do not directly cause canaliculitis, they set the stage for opportunistic infection.
Closure of the Lacrimal Punctum, by Plug
|
 |
 |
Canaliculitis Secondary To Intracanalicular Plug Placement
|
The lacrimal canaliculus is a part of the lacrimal apparatus.
The lacrimal apparatus is a network of anatomical structures, appendages, ducts and glands that secretes the pre-corneal tear film and then drains the tears from the surface of the eye. The outflow of tears is accomplished by the lacrimal drainage system and it includes the following anatomical structures:
- Eyelid margin
- Lacrimal punctum
- Lacrimal canaliculus
- Lacrimal sac
- Nasolacrimal duct
Structural Damage to the Eye
- Chronic or severe inflammation of the canaliculus can lead to permanent scarring
- Canalicular scarring can produce partial or total obstruction of the lacrimal drainage system
- Eyelid induration and pyogenic granuloma can be associated with canaliculitis
- Erythematous pouting of punctum can rub against the conjunctiva and cornea resulting in mechanical damage to those structures
Functional Damage to the Eye
- Decreased vision secondary to frequent blinking and eye rubbing
Current literature states that it is more common to misdiagnose patients with lacrimal canaliculitis than to identify the condition.
The main goal of the diagnostic examination in a patient with lacrimal canaliculitis is to accomplish the following:
- Determine the underlying etiology of the canaliculitis and classify the disease (i.e., primary vs. secondary)
- Relieve ocular pain and discomfort
- Perform diagnostic probing of canaliculi and lacrimal system irrigation to rule out nasolacrimal duct obstruction
- Ensure this is not acute or chronic dacryocystitis
- Prescribe a treatment program to prevent future occurrences
Patient History
Patients with primary canaliculitis may present with any of the following abnormal clinical signs and symptoms:
- Lower medial eyelid tenderness and pain
- Increased tearing
- Non-resolving or recurrent conjunctivitis
- Ocular redness
- Ocular discharge
- Outward pointing or pouting of the inferior lacrimal puncta
- Expressed or voluntary mucopurulent discharge from the inferior puncta
- Mattering on the eyelids
- Concretions expressed from the punctum by massage
Patients with secondary canaliculitis may present with any of the following abnormal clinical signs and symptoms:
- Lower medial eyelid tenderness and pain
- Increased tearing
- Conjunctivitis
- Blood-tinged or mucopurulent discharge
- Intermittent blood-stained tears
- Granuloma formation
- Inflammatory mass projecting from the punctum
External Ocular Examination with Biomicroscopy
When examining the lacrimal drainage system, note any evidence of eyelid malposition and evaluate the dynamics of eyelid closure. Normally, the eyelid margins will be in close proximity and the puncta are apposed when the eyelids are closed. The normal punctum is in contact with the globe and is not usually visible without pulling the lower eyelid downwards and the upper eyelid upwards.
Abnormal findings involving the punctum include malposition, stenosis or obstruction. The lower canaliculus and the lacrimal sac should be palpated and compressed. Abnormal findings include any pain or tenderness during the examination or any reflux of pus or mucopurulent material.
In patients with canaliculitis, it is important to document pertinent negatives. For example, your medical record should reflect that there was no nasolacrimal duct obstruction on irrigation. Also, you should document the absence of nasolacrimal sac inflammation (i.e., sac distention).
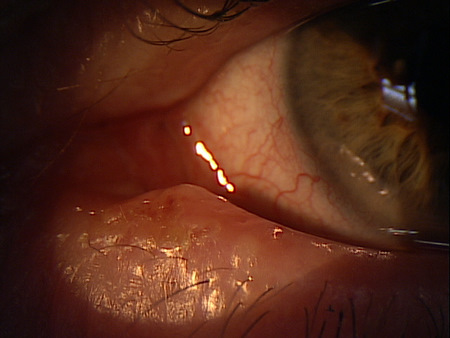
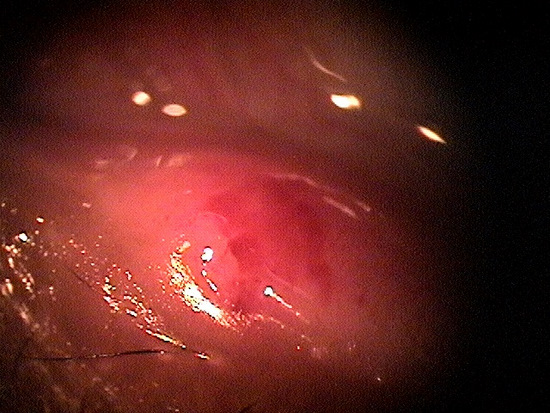
Clinical Appearance of the Eyelid
|
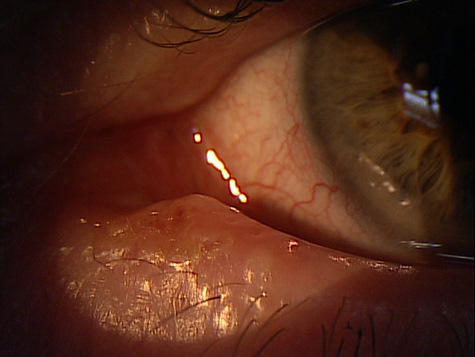 |
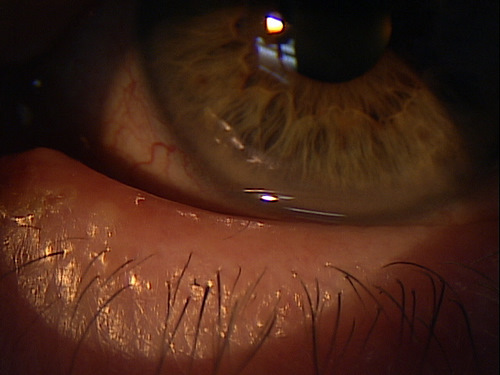 |
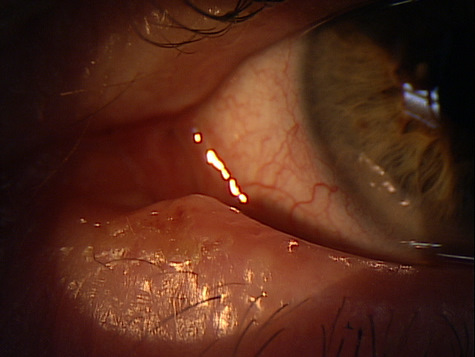
Clinical Appearance of the Conjunctiva and Tear Film
|
|
 |
Clinical Appearance of the Tear Film
|
|
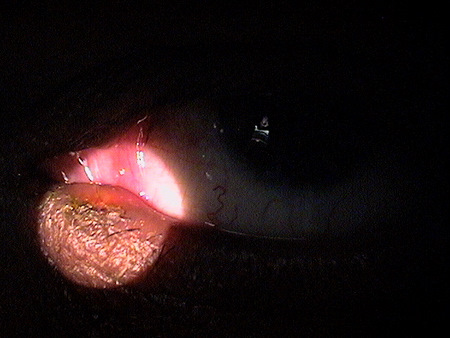 |
Clinical Appearance of the Lacrimal Punctum
|
|
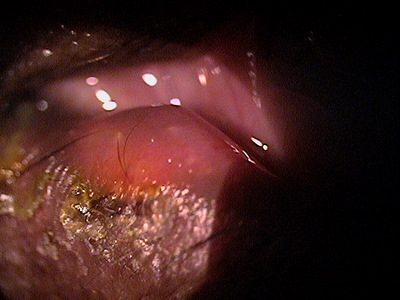 |
Clinical Appearance of the Lacrimal Punctum
|
|
Clinical Appearance of the Lacrimal Punctum
|
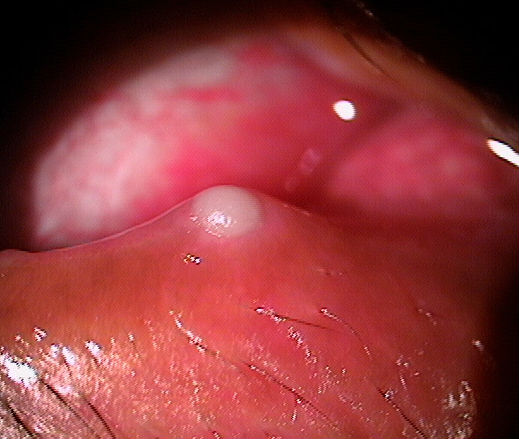 |
Clinical Appearance of the Lacrimal Punctum
|
 |
|
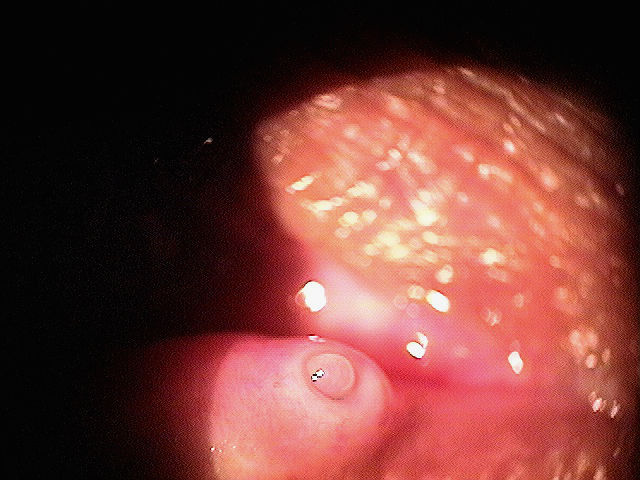 |
Clinical Appearance of the Lacrimal Punctum
|
Lacrimal canaliculitis is separated into primary and secondary presentations depending on the etiology.
- Primary canaliculitis is an inflammation secondary to infection by some microorganism
- Secondary canaliculitis presents as a complication of punctal occlusion or lacrimal intubation
Lacrimal System Neoplasm
- Unilateral tearing
- Unilateral discharge
Conjunctivitis
- No tenderness or pain on canalicular palpation
- No punctal discharge
Nasolacrimal System Obstruction
- No tenderness or pain on canalicular palpation
- No punctal dilation
Dacrocystitis
- More pain, swelling, discharge and tenderness than canaliculitis
- Skin will look swollen rather than a pouing of the punctum
Carunculitis
- An inflamed caruncle can cause medial eyelid tenderness, tearing and redness that is similar to canaliculitis
- Area of inflammation in carunculitis is more isolated to the area around the caruncle instead of the punctum
There are two treatment options for lacrimal canaliculitis — conservative treatment and surgical treatment.
Conservative Treatment
- Warm compresses
- Digital massage
- Topical and systemic antibiotics
- Intracanalicular antibiotic (or iodine) irrigation
If the patient’s canaliculitis is not clinically improved by 48 hours after the initial antibiotic irrigation, repeated intracanalicular antibiotic irrigation treatments may be necessary. Some studies demonstrate an average of four antibiotic irrigation treatments was needed to eradicate the infection.
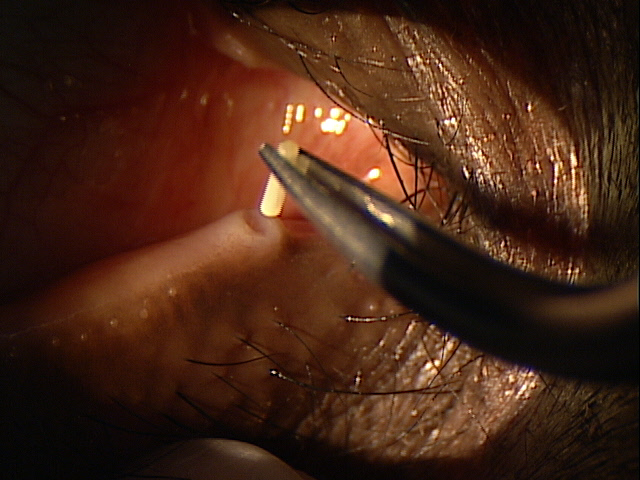
Surgical Treatment
- Canaliculotomy and canalicular cutterage
Primary Lacrimal Canaliculitis
|
 |
|
Resolved Lacrimal Canaliculitis
|
 |
Treatment of canaliculitis depends on the severity of the presentation and the suspected infectious agent. As bacterial infection is the most common etiology, most treatment is aimed at eradicating gram positive bacteria. Several therapies are advocated.
Palliative Therapy
- Warm compress b.i.d to q.i.d
This should be prescribed in addition to any other therapy prescribed.
Pharmacologic Therapy – (bacterial etiology)
Actinomyces israelii
- After removing the concretions, irrigate the canaliculitis with an antibiotic solution (penicillin G 100,000 U/mL) and systemic antibiotics (penicillin V 500 mg p.o q.i.d. for 7 days)
Nocardia asteroids and Fusobacterium
- Topical antibiotic (sulfactamide t.i.d) and systemic antibiotics (trimethorim-sulfamethoxazole [Bactrim] one double strength tablet p.o qd for 7-10 days)
Staphlococcus or general assumption of infectious agent
- Systemic antibiotics (Augmenten 875mg tablet p.o. tid for 10 days).
Pharmacologic Therapy – (fungal etiology)
Candid albicans
- Systemic antifungal (fluconazole 600 mg p.o. qd for 7-10 days)
Aspergillus
- Topical antifungal (amphotericin B 0.15% t.i.d) and systemic antifungal (itraconazole 200 mg p.o. qd for 7-10 days)
Pharmacologic Therapy – (viral etiology)
- Topical antiviral gel (Zirgan five times a day for 1 week)
- Topical antiviral eyedrops (trifluridine 0.1% five times a day for 2 weeks)
Surgery For Primary Canaliculitis
- Repeated intracanalicular antibiotic irrigation
- Canalicular concretions may be removed by manual expression using a cotton-tipped swab (apply gentle pressure over the lacrimal sac and roll the swab towards the punctum and look for turbid punctal secretions)
- If all the obstructing concretions cannot be removed by manual expression, a surgical canaliculotomy may be required
- Silicone tube intubation is sometimes required for definitive treatment
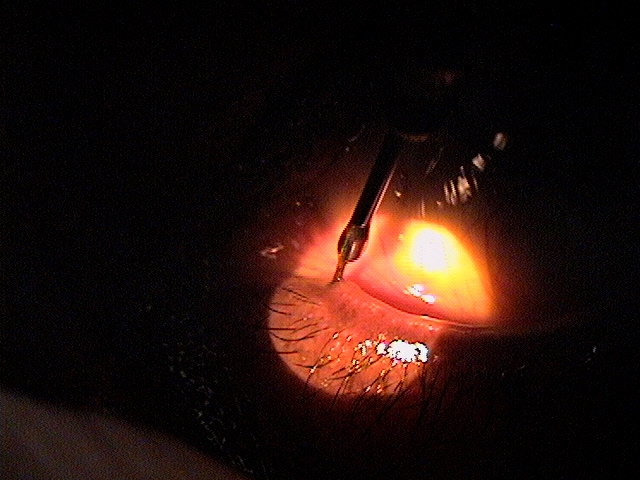 |
Irrigation of the Nasolacrimal Drainage System
|
Surgery For Secondary Canaliculitis
Medical management of secondary canaliculitis is rarely successful and plug removal should be a part of any treatment program.
- Punctal plugs should be removed with forceps
- Intracanalicular plugs may be flushed/probed distally into the lacrimal system
1. Freedman J, Market M, Cohen A. Primary and Secondary Lacrimal Canaliculitis: A Review of Literature. Surv Ophthalmol. 2011 Jul-Aug;56(4):336-47. http://www.ncbi.nlm.nih.gov/pubmed/21620429. Last accessed October 31, 2015.
2. Canaliculitis. RevOptom. Handbook of Ocular Disease Management. http://www.reviewofoptometry.com/cmsdocuments/2010/4/ro0410_hndbk.pdf. Last accessed August 21, 2014.
3. Dimmick T. Gurwood A. Disorders of the Nasolacrimal System. RevOptom.http://www.revoptom.com/continuing_education/tabviewtest/lessonid/109005/. Last accessed August 21, 2014.
375.31
Acute lacrimal canaliculitis
92285
External ocular photography
68801
Dilation of the lacrimal puctum
68840
Probing of the lacrimal canaliculus
68530
Removal of foreign body, lacrimal passages
Occurrence
- The prevalence of primary canaliculitis is unknown
- Estimates suggest 2% – 4% of the patients in an ophthalmic practice have symptoms associated with canaliculitis.
Risk Factors
- Woman are more affected than men in both primary and secondary canaliculitis
- 5:1 ratio in primary canaliculitis
- Advancing age (mean is 59-years-old)




 Print | Share
Print | Share